![]()
PART 1
Your patients
“What’s next in airline self-service: customer-piloted aircraft?” An aircraft manufacturer executive overheard at after-conference drinks.
At UCL Medical School, I teach a class called “Wiki Medicine.” The students have to create a wiki of medical information for patients to understand their illness. I ask them at the beginning: “if patients know more than ever before about medicine, and if patients with chronic diseases know more about their illnesses than the junior doctors you will become, what is the point of being a doctor?”
Take a moment to think about this. How are you helpful to your patients when patients can help themselves?
After a hesitant start, the students begin to raise their hands. A doctor can listen, to understand the patient’s problem, and to make the patient feel understood. This doctor can examine the patient, making objective observations that help with the diagnosis. With understanding and observation, the doctor can recommend lifestyle changes, prescribe medications, or refer to colleagues. With this advice and support comes reassurance and relief for the patient. When the doctor cannot cure, they can still care, gently squeezing the patient’s hand.
And as the executive at the aircraft manufacturer pointed out, passengers cannot pilot aircraft, and neither can patients carry out their surgery.
So what has changed because of technology? For any student who went to medical school so they could feel like the smartest person in the consulting room: the world has changed. Patients are getting a lot smarter, and they have far more time and interest than clinicians do to get smart about their own particular problems.
But for every other aspect of caring for patients, patients want their clinicians more than ever before. And as a clinician you can proceed free of the burden of needing to know more than your patient does. You can just take joy in caring about your patients as you care for them.
![]()
CHAPTER 1
Sharing data with your patient
How can we expect patients to participate in their health care if we don’t give them their data?
Dr. Daniel Sands, Beth Israel Medical Centre
Dr. Amir Hannan was apprehensive about his first day as a family physician. That was because he was replacing Dr. Harold Shipman, the family physician and serial killer convicted in 2000 of murdering 15 patients in his community. The subsequent enquiry (www.the-shipman-inquiry.org.uk) concluded that Dr. Shipman had probably killed 250 patients.
The remaining patients had trust issues with Dr. Hannan.
I am still amazed by Dr. Hannan’s response. Instead of backing away when he was told what surgery he would be working in, he stepped forward. Instead of ignoring the reason for his patients’ distrust, he discussed it openly with them. And instead of asking the patients to trust him, he asked that they join him. You can listen to my interview with him at podcast.patientsknowbest.com (Hannan 2008).
Over the past few years, Dr. Hannan has provided his patients with access to all their medical notes through the Houghton Thornley Medical Centre’s website at www.htmc.co.uk. Patients who signed up soon found what you would expect them to find: that Dr. Hannan is an honorable man, committed to the care of his patients. Hannan found that for most of his patients, knowing that he was being transparent was all they needed to know. Most of them did not register, simply choosing to benefit from his clinical expertise now that they had established a relationship of trust.
But Hannan also found out how important record access is to clinical care. He began encouraging each patient to sign up so that they could work together, as a team, to improve the patient’s health.
Nobody is as smart as everybody
Across the Atlantic, Vanderbilt University Medical Center has an excellent patient portal at www.myvanderbilt.com. Dr. Jim Jirjis, a physician and VUMC’s Chief Medical Information Officer, told the story of a patient who came in complaining of chest pain. He ordered a CT scan to check for aortic dissection and was relieved when the radiology report showed the patient did not have this diagnosis. A few days later, however, the patient contacted him asking about the “lump” in the radiology report. The radiologist had mentioned this incidental finding in the throat. Sure enough, the lump was from thyroid cancer, and this story has a happy ending. Surgeons excised the cancer early, and the patient has not had a recurrence.
Like Hannan, Jirjis now encourages his patients to sign up because it is the safe thing to do. While some doctors worry that accessing the records means that patients will discover errors and begin litigating, Jirjis and Hannan believe that the best defense against litigation is enlisting patients’ help with finding the errors.
Safety from numbers
But what about the dangers from access? A common fear among clinicians is what happens when patients see test results without the benefit of counseling from their clinicians. For example, what would happen if patients found out from a website that they are HIV positive, or if they read and misunderstood a test result because a clinician was not there to interpret it with them?
The short answer is that in most cases, the fears are theoretical while the benefits are tangible. But it is worth explaining why and showing a few cases of how different clinicians picked the work flow that best suited them and their patients.
And the first thing to say is that you do have a choice. The original reason that test results were delivered with clinicians is that test results were printed on pieces of paper, and the piece of paper had to go to the clinician. It was easiest for the clinician to read out that piece of paper to the patient than to print off another copy and send it to the patient separately. These are reasonable choices given the limitations of paper, but technology removes these limitations. Sending out hundreds of digital copies of a test result costs the same as sending just one copy.
So what should you choose? One extreme example is MD Anderson Cancer Center, one of the top cancer referral centers in the world. There, all test results are made available to the patient instantly. But that is not the extreme part. MD Anderson is special because they were doing this from their early days when results were printed out on paper. The results would be stored in the paper notes, and the paper notes were stored at the foot of each patient’s bed. The patients often read the results before the clinicians came for their ward round.
MD Anderson did this because their patients know that they have cancer. There is no harm from bad news because the patients already know the bad news and their clinicians need them to know the bad news. Everyone is on the same team fighting cancer, and everyone on that team needs to have all the information as soon as it is available.
The second thing to say is that the distress from receiving bad news without a clinician’s counseling is not as bad as the distress of waiting for news until a clinician has time to counsel you. For the clinician, waiting for a result is fine because they have so many other patients to care for and because reading bad news is something they do all the day as they provide that care. But for a patient, that test result is all they can think about. And if the news can be bad, they will assume it is bad until they are told otherwise.
This is what prompted to the genitourinary medicine staff at Chelsea and Westminster Hospital to offer their SMS service. HIV is on the mind of most of their patients as they come in for testing, and the stress of waiting is terrible. Staff offered patients the choice of receiving the test results by a text message on their cell phones. Patients overwhelmingly opt into the service because it reduces the wait and because cell phones allow an intimate setting in which to read the result.
No one is told that they are HIV positive through a text message. Instead, most patients are HIV negative, and those patients are instantly told through text messages that they are fine. For the few who are sadly HIV positive, the message they receive is that they should call the clinic to arrange an appointment. A member of staff then delivers the news in person, with counseling and follow-up care. The time to diagnosis and treatment was shorter when delivering news through text messages (Menon-Johansson 2006).
The third thing to say is that your choices can be nuanced. At Vanderbilt Medical Center, the clinical team divided tests into three groups of “information toxicity.” Most tests have low information toxicity, for example, hemoglobin levels of sodium concentration. Results from these tests are released immediately. High information toxicity tests include those for HIV. They are only released with a clinician’s permission, and this is usually after the clinician has seen the patient. The remaining results are released after a clinician gives permission, or 2 weeks, whichever happens first. Because after 2 weeks, the benefits of clinician counseling are definitely outweighed by the patient access.
And finally, it is worth saying that most patients are more resilient than most clinicians give them credit for being. To a lay person, SOB does not instinctively mean shortness of breath. And to a patient with a psychiatric illness, reading the opinions of their clinical team can be distressing. But early experiences show that patients wait to talk to their doctor before assuming the worst about abbreviations such as SOB. And for psychiatric patients, understanding that different people have different interpretations of the same events is an important part of treatment.
But the evidence is not yet definitive, which is why the Robert Wood Johnson Foundation funded the OpenNotes Project in 2009. On the website, www.myopennotes.org, it will document the experiences of clinicians in sharing all medical notes, all the time, with patients who participate in the study. As we await the full outcomes, it is worth spelling out the benefits of sharing as most clinicians instinctively worry about the risks.
Early sharing gives your patients time to do their homework
Perhaps the strongest argument for giving patients early access to their data is that this gives them time to think about the data before they come in for an appointment. Because during the appointment, their thinking is far from perfect. There is a large body of evidence to support this view. For example, 40–80% of the medical information you provide is forgotten immediately. And the more information you provide, the lower the proportion your patient can correctly recall (McGuire 1996). Furthermore, almost half the information they remember is incorrect (Anderson et al. 1979).
But with a personal health record (PHR) at home, the patient can read all the data, look up what they mean, and prepare questions. They will make better use of their time with you.
Patients can be very good at doing their homework
Patients have incredible tools available to them. It is not just the growth in patient-friendly health care encyclopedias, but the widespread availability of tools originally designed for clinicians.
On the web, one of the earliest data points for this was membership of Medscape, a website for clinicians that had gained one million users by the turn of this century. But as early as 1996, the creators of the site had noticed that 30% of registrants were not health care professionals. For some of them it was a matter of not minding the difficulties of understanding the complex information, but for others it was about spending the time to learn to understand what their doctors and nurses already understood.
Policy makers recognize this demand. In the United States, President Bush and Congress both backed efforts to ensure that research paid for by the public would be available to the public without further payment. In the UK, the NHS Evidence website is freely available at www.evidence.nhs.uk and makes huge amounts of primary medical papers freely available. Your patients are reading primary papers.
They are even reading materials you did not think they were allowed to read. In 2009, Dr. James Heilman from Saskatchewan, Canada, posted the Rorschach test, and its answers, onto the Wikipedia. Anyone can see the ten blots (Figure 1.1) and how psychiatrists interpret patients’ responses, at http://en.wikipedia.org/wiki/Rorschach_test. The posting was a controversial one, with psychiatrists and psychologists explaining that the test is not valid if a patient can read the interpretations before taking the test.
This is a shame, but it is not something you can prevent. In this case, the plates had been publicly available as far back as 1983 as part of the book Big Secrets, by William Poundstone. Publication in the Wikipedia simply made it easier for the public to understand the test. Clinical care that relies on keeping secrets from patients is bound to fail as the web allows easy access to these secrets.
So instead you should embrace the opportunity. And it is huge. Because just as patients now have easy access to useful data, so do you: your patients can now give you access to all the symptom diaries and home test results that can guide your care, but which were previously too laborious to collect and collate.
Patients have lots of data to share back with you
At most you have one hour with each patient each year. That leaves over 8,700 hours, which the patient spends without you. For many conditions, such as diabetes, asthma, and rheumatoid arthritis, it is difficult but important to find out what goes on during these hours. Paper diaries are common but inadequate. Filling these out is inconvenient, so they arrive to you incomplete and inaccurate. They are also out of date, and you cannot be sure whether they were filled out on the day of observation, or later on from memory.
Technology is beginning to help. This is because medical devices are increasingly digital, able to output their data streams to medical databases. The data streams are increasingly in the Continua data standard, which is compatible with an increasing number of PHRs. The details are further discussed in Chapter 7, but the point is that you can overcome many of the burdens of paper diaries.
So what data can you start collecting from your patients today?
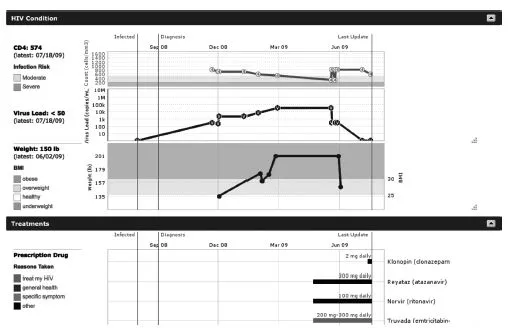
PatientsLikeMe (Figure 1.2, www.patientslikeme.com) has demonstrated the value of symptom diaries. Thousands of patients post data in each of its patient communities. The figure above shows the clarity this brings to a patient’s history and current status. Before encouraging your patient to sign up though you should explain that publishing should not mean publicizing identity. Patients should withold identifying information such as their name, address, and photograph. The next chapter discusses steps you can take to protect your patients’ privacy and you can listen to the podcast interview with their director of research and development at http://podcast.patientsknowbest.com (Wicks 2009).
The nice thing about sites such as PatientsLikeMe is the printouts they provide. They are easy to understand, and each diagram shows what currently occupies several pages of handwritten notes.
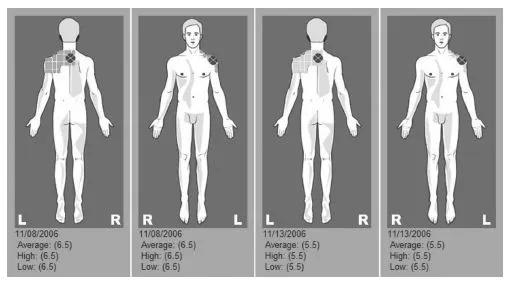
But it is also possible to use PHRs to show what is impossible to explain in the notes. For example, ReliefInsite (www.reliefinsite.com) documents what the patient explains to you when they wince and grip their shoulder. Pain is complex and tactile, and while there is no substitute for examination, there is great benefit from understanding how the pain has changed in character and location. For patients, there is relief even in being understood—of finally being able to document what their pain is like and how it changes.
The website (Figure 1.3) does this through standard diagrams and templates that have been approved by pain specialists. Repeated data entry is possible through telephone voice prompts, as well as the website, for patients with too much joint pain to use the keyboard, for example. Automated time tracking means you can trust when the patient entered the observation, rather than paper diaries where the patient may be filling out their recollections long after the event happened. And animations on the website tell the story the patient wants you to understand. You can listen to the interview with the CEO at http://podcast.patientsknowbest.com (Eberlein 2009).
Beyond documenting what happened, the patient can document what they did about it. For example, patients using ZumeLife (www.zumelife.com) enter what time they actually t...