![]()
Part I
Pathology and Diagnosis
![]()
Chapter 1
Disease Pathogenesis
Roopali Gandhi and Howard L. Weiner
Partners Multiple Sclerosis Center, Center for Neurologic Diseases, Brigham and Women's Hospital and Department of Neurology, Harvard Medical School, Boston, MA, USA
Introduction
Multiple sclerosis (MS) is a chronic inflammatory disease of the central nervous system (CNS) that primarily affects young adults [1]. The role of immune system in MS is indisputable. The primary function of the immune system is to protect the body against myriad ever-evolving pathogens and it broadly falls into two categories the “innate immune system” and “adaptive immune system.” The important difference in the innate and adaptive arms of immunity is that the adaptive immune system is highly specific toward an antigen. The immune-mediated inflammation of MS was initially recognized in 1948 by Elvin Kabat who observed the presence of oligoclonal immunoglobulins in the cerebrospinal fluid from MS patients. In following years, great strides have been made in understanding the role of both adaptive and innate immune system in Experimental Autoimmune Encephalomyelitis (EAE, an animal model of MS) MS but it is not known the degree to which the adaptive and innate immune systems interact in MS.
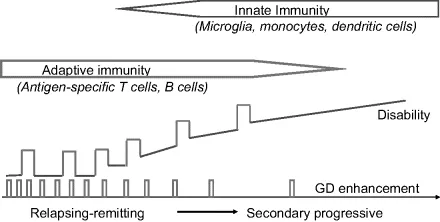
In most instances, MS begins as a relapsing remitting disease that in many patients becomes secondary progressive. Approximately 10% of patients begin with a primary progressive form of the disease. Although primary progressive MS differs clinically and in treatment response from relapsing MS [2], it is somehow related as there are families in which one member has relapsing MS and another the primary progressive form. Not all patients enter the secondary progressive stage and, in addition to these, there are benign and malignant forms of MS. This heterogeneity of the clinical course may relate to changes that occur in the adaptive and innate immune system over the course of the illness (Figure 1.1). The progressive forms of the disease are the most disabling and are likely similar in terms of pathogenic mechanisms. Epidemiologic studies have raised the question whether relapses are related to or are independent from the development of progressive MS [3]. This raises the central question: will current therapy that is effective in reducing relapses also delay or prevent the onset of progression? The understanding of MS pathology and immune system helped us to design various treatment strategies for MS and, given this progress, we must now ask: “What would it mean to cure MS?” and “What is needed to achieve this goal?” [4]. When one examines these questions, it becomes clear that there are three definitions of “cure” as it relates to MS: (1) halt progression of the disease; (2) reverse neurologic deficits; and (3) develop a strategy to prevent MS. We are making progress in halting or slowing the progression of MS, have approaches that may help to reverse neurologic deficits, and, for the first time, are beginning to develop strategies to prevent MS.
Clinical and pathologic heterogeneity of MS
Multiple sclerosis is a nondescript term that refers to “multiple scars” that accumulate in the brain and spinal cord. MS is more a syndrome than a single disease entity and the MS syndrome has both clinical and pathologic heterogeneity [5, 6]. The clinical heterogeneity is reflected in the different types and stages of the disease. An important question in MS is the relationship of the progressive to relapsing forms. Devic disease appears to be an MS variant associated with antibodies to the aquaporin receptor [7, 8]. There are rare malignant forms including Marburg's variant, tumefactive MS and Balo's concentric sclerosis. An unanswered question relates to why benign forms of MS exist [9, 10]. Although some cases of MS are defined as benign, and progress with prolonged follow up [11] there are clearly benign forms of the disease. By definition patients with benign MS do not enter the progressive phase. The ability to identify benign or malignant MS early in the course of the illness is very important for treatment strategies. We compared brain parenchymal fraction (BPF) over a 2-year period in benign vs early relapsing-remitting MS matched for age and the EDSS and found that patients with benign MS had a smaller loss of BPF [12]. As it impinges on the EDSS, the majority of disability in MS relates to spinal cord dysfunction. The relationship between spinal cord changes and brain MRI changes is not well known, but changes in the medulla oblongata which reflect spinal cord can be visualized on brain MRI and may correlate with entering the progressive phase [13]. In addition, an HLA-DR2 dose effect may be associated with a more severe form of the disease [14].
What triggers MS?
The etiology of MS is still debatable but the current data suggests that environmental factors in genetically susceptible background can predispose an individual to MS. Family studies assessing the risk of relatives suggests that first-degree relatives are 10–25 times at greater risk of developing MS than the general population [15–17]. The strongest genetic effect is correlated with HLA haplotypes. For instance HLA*1501, HLA-DRB1*0301, HLA-DRB1*0405, HLA-DRB1*1303, HLA-DRB1*03, HLA-DRB1*01, HLA-DRB1*10, HLA-DRB1*11, HLA-DRB1*14 and HLA-DRB1*08 have been shown to have either positive or negative association with MS [15]. Ethnicity and sex are other contributors in susceptibility to MS. The white population is more susceptible to disease than the African American population and women are at higher risk of developing MS than men [18], which is not associated with any MS-related gene present on the X chromosome but is more correlated with female physiology and hormones [19]. Other potential environmental risk factors are infections, vaccination, climate, and diet. Infections are considered the most common risk factor for MS as many infections and antibodies generated in response to these infections are present in sera or the cerebrospinal fluid (CSF) of MS patients at higher titers than controls. Epstein–Barr virus (EBV) is of great interest as >99% of MS patients and approximately 94% of age-matched controls are infected with EBV and increased antibody titers to EBV nuclear antigen 1 (EBNA-1) antigen are reported in MS [20, 21]. Other infectious agents linked to MS etiology are herpes virus 6, retroviruses and Chlamydia pneumonia [22]. Evidence for association of Chlamydia pneumonia with MS is debatable, as contradictory presence of this virus has been reported by different groups [23–26]. Decreased sunlight exposure, vitamin D level, and vitamin intake are also associated with MS incidence or protection [27, 28]. In addition, studies using different cohorts of MS patients have shown a strong association between smoking and MS [29, 30]. The etiology of MS is discussed in detail in the Chapter 3.
Top Tips 1.1: Risk factors for MS
| • HLA susceptible genes | • Climate |
| • Ethnicity | • Gender |
| • Infections | • Smoking |
| • Vaccinations | • Diet |
Pathology of MS
The pathology of MS lesion is defined by the presence of large, multifocal, demyelinated plaques, oligodendrocyte loss, and axonal degeneration. During the early development of MS lesions, the integrity of the blood–brain barrier is compromised, permitting the invasion of monocytes and T cells to the brain parenchyma. Mononuclear cells including activated microglia and peripheral monocytes are the primary cells involved in the demyelination of MS lesions. According to Trapp's classification, MS lesions are categorized into three groups, active (acute), chronic active, and chronic inactive. Active and chronic active lesions are characterized by the presence of evenly distributed MHC class II positive cells [31]. Chronic active plaques are characterized by the presence of MHC class II and myelin lipid positive cells that are distributed perivascularly [31], whereas, chronic inactive lesion have few MHC class II positive cells [31] (Figure 1.2). Microarray results of autopsies from acute/active vs chronic silent lesions revealed a number of differentially expressed genes present only in active lesions [32]. These differentially expressed genes are mostly related to cytokines and their associated downstream pathways [32]. According to another classification based upon a broad spectrum of immunological and neurological markers on a large set of MS pathological samples, MS lesions were characterized into four different patterns. Patterns I and II are defined by the T cell and macrophage-mediated inflammation where pattern II exclusively showed antibody and complement dependent demyelination [33]. Pattern III lesions also contained T cells and macrophages and are defined by distal oligodendrogliopathy [33]. Pattern IV is characterized by the complete loss of oligodendrocyte in addition to the presence of inflammatory infiltrates mostly dominated by T cells and macrophages [33] (Plate 1.1).