Chapter 1
Identifying the Problem
THERE’S NO POINT IN TRYING a bunch of solutions for a sleep problem you don’t have. But you’d be surprised how frequently people are treated for the wrong thing or aren’t treated at all.
One reason this happens is that sleep disorders don’t always present with their most well-known symptoms or red flags. Without the detailed knowledge of a sleep specialist, many patients—and sometimes their doctors—assume they have a different sleep disorder, a different problem entirely, or no problem.
People also tend to assume that if they’re not sleeping well, they must have insomnia, and studies show that most people with insomnia don’t seek professional help. That means a huge chunk of people are missing out on learning that their insomnia is treatable or that their problem’s not actually insomnia.
It’s also very possible to have more than one sleep issue. Treat only one of them and you’ll still be left with a problem.
Of course, the best way to determine what’s keeping you awake is to see a sleep specialist, but there are a few things you can do at home to narrow down the possibilities. This chapter aims to give you a quick summary of some of the more common sleep disorders and tools to help you determine which, if any, you might have.
Insomnia
Insomnia is the most common sleep disorder in the world, and arguably the most misunderstood. Even sleep experts can’t seem to settle on one definition for what insomnia actually is. Sometimes it’s a symptom, sometimes a disorder. Read three different books and you might get three different answers.
For the purpose of this book, I’m going to define insomnia as unexplained difficulty falling asleep or staying asleep, despite adequate opportunity to sleep, resulting in impairment.
Have you ever felt like crap because you couldn’t fall asleep or stay asleep the night before for no apparent reason? Just couldn’t stop . . . thinking? You have experienced insomnia.
The next question is for how long? If you just have the occasional bad night, that’s completely normal and doesn’t require any special interventions. But if you have insomnia on a regular basis, there are several steps you can take to address it.
Because insomnia is such a complicated beast, we’re going to spend a lot more time in this book discussing why it happens and how to fix it. Still, even if you feel confident you have insomnia, be sure to read the rest of this chapter. Insomnia is especially easy to confuse with other sleep issues and frequently coexists with them. Let’s ensure you’re addressing the right problem and the whole problem.
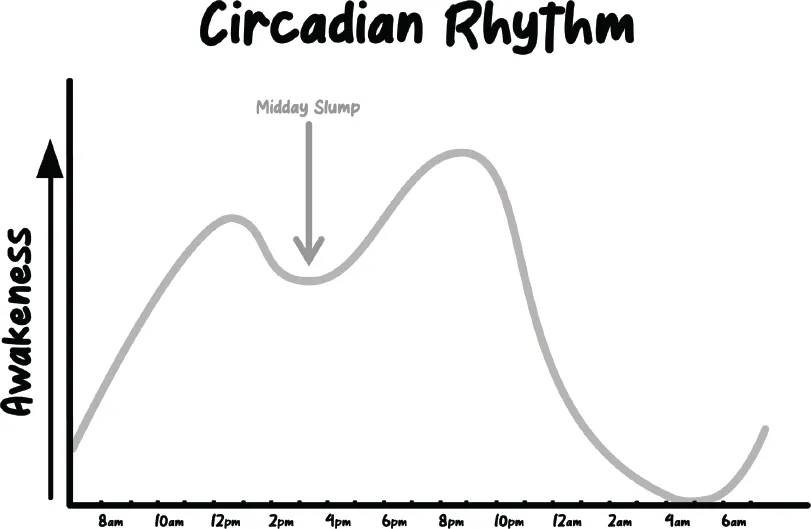
Circadian Rhythm Disorders
Circadian rhythm disorders are a timing issue. They happen if we regularly try to sleep when our body naturally wants to be awake. But it can be tricky to differentiate a circadian rhythm disorder from insomnia because they present in the exact same way: you have trouble falling asleep or staying asleep, with no symptoms to indicate anything else is wrong.
In fact, even doctors can confuse the two conditions. A 2017 study led by Dr. Steven Lockley at Harvard Medical School found 10 to 22 percent of patients diagnosed with chronic insomnia actually had a circadian rhythm disorder.
This is also another area where the definition of insomnia gets muddied. Some sleep experts consider a circadian rhythm disorder to be a type of insomnia. Others tell me it’s a separate condition. For clarity and ease I’m going with the latter group because the two problems have different causes and different solutions.
The easiest way to tell the difference between a circadian rhythm disorder and insomnia is that those struggling with a circadian rhythm disorder can get a good night’s sleep when they’re able to do it on their schedule. For example, if you struggle to fall asleep and wake up during the workweek but sleep fine when allowed to stay up late and sleep in on weekends, it’s likely your circadian rhythm that’s causing your sleep issues, not insomnia.
Luckily, as with insomnia, there’s a lot you can do at home to troubleshoot circadian rhythm issues—some as simple as wearing sunglasses at the right time. If you suspect this is your issue, be sure to check out part 3 of this book.
Still, it is very possible to have both circadian rhythm issues and insomnia, like I did. In this case, you will need to resolve both. Parts 2 and 3 of this book should be a big help.
Sleep Apnea/Sleep Disordered Breathing
Sleep apnea is another common sleep disorder that’s generally not taken seriously enough. It should really be called “sleep suffocation” because that’s basically what’s happening. Those who suffer from it repeatedly stop breathing in their sleep for at least ten seconds at a time—up to a hundred times per hour! Imagine someone was smothering you with a pillow or choking you over and over again all night long while you tried to sleep—you’d probably make it a top priority to remedy that problem ASAP. But while the body does wake up from an apnea to breathe again, those awakenings are usually so brief you don’t remember them. So despite the severity of the condition, many sleep apnea patients don’t even realize they have it.
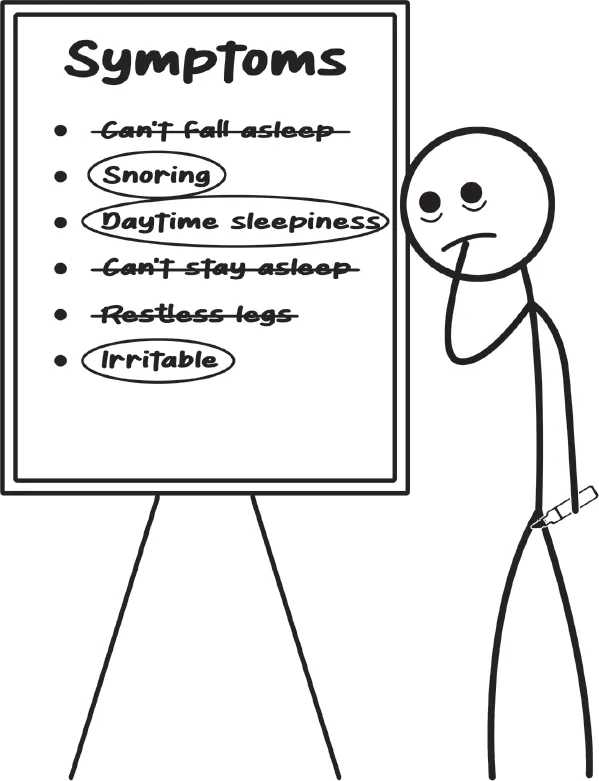
For my dad, it wasn’t until my mom pushed him to get a sleep study that he finally got diagnosed with sleep apnea. But Dad says in retrospect there were warning signs. “I thought I slept all night . . . but I felt tired,” he tells me. Throughout the day, during moments of stillness, Dad would even feel the strong urge to nod off. “I would get involved with doing something else to distract my body, so I would not fall asleep,” he says.
Dad now calls his CPAP machine a “godsend,” saying as soon as he started using it, he felt “great.” He explains, “[It’s like] when you take medication for your headache and then the headache goes away.”
Since Dad started treating his sleep apnea, his boost in energy and mood is obvious to anyone around him, and I couldn’t be happier for him and for us. But he does have a heart condition and high blood pressure, which led to a nearly fatal stroke last year, and I wonder how much of that is due to the decades he likely spent with untreated sleep apnea. Because those breathing interruptions don’t just disrupt your sleep, they also cause sudden drops in blood oxygen levels. According to the Mayo Clinic, these leave you at higher risk for high blood pressure, recurrent heart attack, stroke, and even sudden death from an irregular heartbeat. Sleep apnea can also put you at higher risk for type 2 diabetes, metabolic syndrome, liver problems, and of course car crashes and workplace accidents.
Adam Amdur, chairperson of the American Sleep Apnea Association, says he believes the heart condition and early-onset dementia that killed his father were due to sleep apnea. “My father had triple bypass at thirty-eight. I was six months old,” he tells me.
Adam also had his own issues but could never seem to pinpoint why. “I was always a smart kid who got an A in calculus [tests] but a C in the class because I was too tired to do my homework. I started and stopped so many different film projects . . . I literally fell asleep at the wheel when I was twenty-seven years old in Miami with my best friend in the car—drove through a gas station,” he says.
After the crash Adam went to doctor after doctor trying to figure out what was wrong. “They just said you’re young and dumb. They assumed that I was doing drugs or I was drinking,” he says.
Then years later Adam’s best friend, Brian, had just finished med school and joined Adam and his family on vacation. Adam explains, “He saw me nod off in a chair in the afternoon . . . then that night heard me snoring through the walls. The next morning, he looks right up at my mother, through me, says, ‘I know what’s wrong with Adam, and Mrs. Amdur, I know what was wrong with your husband.’”
At Brian’s urging, Adam went for a sleep study immediately upon returning home. He says within twenty minutes of being asleep, the tech paused the study and immediately started him on a CPAP machine, the first-line treatment for sleep apnea.
Adam says he woke up at 5:36 the next morning feeling like he’d been “shot out of cannon.” “I was thirty-five years old at the time, and my brain felt like it was ten years old. I hadn’t felt that fresh and that energetic and that clear in over twenty-five years,” he says.
But Adam didn’t stop there. Noticing warning signs in other members of his family, he pushed his mother to get tested for sleep apnea and even took his two-year-old daughter to get evaluated. Both came back positive. “I then realized not only that this was my life’s problem, this ran in my family,” Adam says, “and it was time to reach out and help others.”
Both my dad and the Amdurs have what’s called obstructive sleep apnea, the more common form of the condition. This is when the airway is blocked during sleep, usually between snoring. But contrary to popular belief, not everyone who snores has sleep apnea—and not everyone who has sleep apnea snores. In fact, the rarer type, central sleep apnea, has nothing to do with the airway at all. It happens because the brain fails to send a signal to the body to breathe, usually due to a severe underlying condition like heart failure. Central sleep apnea is harder to flag than obstructive sleep apnea, but thankfully, it’s also extremely rare, estimated to affect less than 1 percent of the general population.
Obstructive sleep apnea, on the other hand, is estimated to affect 33 percent of U.S. adults between thirty and sixty-nine years old. It’s even more common in advanced age. And many of those people are going untreated. For some, it’s because they’re avoiding the treatment, not realizing how many options are actually available. For others, as explained above, it’s because they have no idea they even have sleep apnea. The latter is especially true for four groups: insomniacs, racial and ethnic minorities, women, and children.
Sleep Apnea and Insomnia
While sleep apnea and insomnia are completely different conditions, science is showing they may be more linked than previously thought. Several studies now indicate a large majority of insomniacs—up to 99 percent!—who wake in the middle of the night are unknowingly being woken up by sleep apnea or other sleep disordered breathing. Unlike standard sleep apnea patients, who don’t realize they’re briefly waking up, those with insomnia are sent into a state of arousal (not that kind of arousal) and have trouble falling back asleep. These patients often complain about waking to go to the bathroom, racing thoughts, anxiety, fatigue, but most don’t complain about respiratory issues. So their sleep disordered breathing goes untested, undiagnosed, and untreated. They might even use sleeping pills to treat their insomnia, not realizing the pills can make their sleep disordered breathing worse.
Minorities and Sleep Apnea
While sleep disorders affect people of all races and ethnicities, according to the Sleep Foundation “there are strong indications that they have a disproportionate impact on racial and ethnic minorities.” Sleep apnea, for example, “was found to be noticeably more com...