
eBook - ePub
Handbook of Chronic Total Occlusions
George D. Dangas, Roxana Mehran, Jeff Moses, George D. Dangas, Roxana Mehran, Jeff Moses
This is a test
Share book
- 262 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Handbook of Chronic Total Occlusions
George D. Dangas, Roxana Mehran, Jeff Moses, George D. Dangas, Roxana Mehran, Jeff Moses
Book details
Book preview
Table of contents
Citations
About This Book
Chronic total occlusions (CTO) are common, and found in approximately one third of patients with significant coronary artery disease who undergo angiography. CTO constitute one of the main criteria when selecting between angioplasty and bypass surgery. Angioplasty for CTO is intricate andrequires excellent operator skill, but even when perfor
Frequently asked questions
How do I cancel my subscription?
Can/how do I download books?
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
What is the difference between the pricing plans?
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
What is Perlego?
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Do you support text-to-speech?
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Is Handbook of Chronic Total Occlusions an online PDF/ePUB?
Yes, you can access Handbook of Chronic Total Occlusions by George D. Dangas, Roxana Mehran, Jeff Moses, George D. Dangas, Roxana Mehran, Jeff Moses in PDF and/or ePUB format, as well as other popular books in Medizin & Medizinische Theorie, Praxis & Referenz. We have over one million books available in our catalogue for you to explore.
Information
Chapter 1
Patient selection and general approach to CTO revascularization
Charles Perry and George D Dangas
Clinical outcomes • Patient selection • General approach • Vascular access • After successful wire crossing
A considerable variety of unsettled issues surround the field of chronic total occlusions (CTOs) as a target for revascularization procedures. There is continual refinement of the following issues: establishment of robust indications, optimal technique, and the ultimate impact of revascularization on patient outcomes. An international expert consensus document has recently addressed these subjects.1,2
Although other types of revascularization procedures have been established over time based on early results, and then expanded through new indications based on long-term data, this has not been the case for approaching CTO lesions. Difficulty achieving predictable procedural success, together with duration of CTO procedures, (with implications for optimal laboratory time personnel), equipment resource utilization, radiation exposure, and complications, have all posed a unique set of hurdles for routine CTO targeting. Although CTO lesions are observed in approximately one-third of diagnostic coronary arteriograms, recanalization is attempted in less than 15% of patients undergoing percutaneous coronary intervention (PCI).3,4 Indeed, the most common reason for referral to bypass surgery or exclusion from clinical studies comparing outcomes of angioplasty to bypass surgery has been the presence of a CTO.5,6
Clinical Outcomes
In a large meta-analysis of 4400 patients, Freed et al demonstrated a long-term success rate of 69% in patients after CTO angioplasty, with a major acute cardiovascular event rate of 2%.7 Long-term success was defined as restriction of lower recurrence of ischemia, improvement of left ventricular function, and higher event-free survival rate. The majority of failures (80%) were free of complications and due to an inability to cross the lesion with a wire, a fact which emphasizes the importance of appropriate patient and material selection. The SICCO trials demonstrated favorable results with stent implantation after successful recanalization; the cardiovascular event rate during 3 years of follow-up was found to be 24% in patients with stents, compared with 59% in conventional angioplasty alone.8
The Mid-America Heart Institute Study,9 British Columbia Cardiac Registry,10 and Total Occlusion Angioplasty Study (TOAST-GISE)11 reported on the clinical impact of successful percutaneous CTO revascularization on long-term clinical outcome. The Mid-America Heart Study retrospectively analyzed a consecutive series of 2007 patients over 20 years (1980–1999) of performing PCI for non-acute coronary occlusions. Importantly, long-term survival was similar in patients with successful CTO recanalization compared with a matched cohort of patients undergoing successful angioplasty of non-occluded lesions, and significantly longer than in patients where attempted CTO revascularization failed (10-year survival 74% with CTO success vs 65% with CTO failure; p <0.001). By multivariate analysis, failure to successfully recanalize the CTO was an independent predictor of mortality.
The British Columbia Cardiac Registry studied 1458 patients with CTOs, which constituted 15% of the attempted revascularizations. Successful percutaneous revascularization of CTO was not only associated with increased survival and reduced need for surgical revascularization over 7 years of follow-up but also with a 56% relative reduction in late mortality.
In the prospective TOAST-GISE of 390 CTO (in 369 patients), a successful PCI was associated with: a reduced 12-month incidence of cardiac death or myocar-dial infarction (1.1% vs 7.2%), a reduced need for coronary artery bypass surgery(2.5% vs 15.7%) and greater freedom from angina (89% vs 75%).
In the overall study population, the only factor associated with enhanced 1-year event-free survival was successful CTO recanalization (odds ratio=0.24; p <0.018).
Patient Selection
The interventional cardiologist must weigh the individual risks and benefits for each patient when deciding to attempt PCI of a CTO vs two other alternatives: aortocoronary bypass surgery or medical therapy. Clinical, angiographic, and technical considerations must be considered in combination.
From a clinical point of view, age, symptom severity, associated comorbidities (e.g. diabetes mellitus and chronic renal insufficiency), and overall functional status are major determinants of treatment strategy. Angiographically, the extent and complexity of coronary artery disease, likelihood for complete revascularization, and the presence and degree of valvular heart disease and left ventricular dysfunction are all very important factors. The technical probability of achieving successful recanalization of the PCI without complications, as well as the anticipated restenosis rate, must also be heavily weighed in the decision-making process.2
When the CTO is the lone obstructive lesion in the coronary vasculature tree, there are three conditions which, when present, favor PCI. The first condition is the presence of symptoms. An average chronic total occlusion with well-developed collaterals is hemodynamically similar to a 90% coronary stenosis without collateral vessels.12 In a consecutive cohort of 127 patients with visible collaterals and successful CTO recanalization, Werner et al showed that collateral function, measured by intracoronary Doppler and pressure wire indices, was similar in patients with and without post-PCI regional left ventricular functional recovery.13 Therefore, although considerable recovery of ventricular function after recanalization can be expected (occurring in 39% of patients with baseline ventricular dysfunction in this series), it is independent of invasively determined parameters of collateral function. Coronary collateral development is not closely linked to myocardial viability but is rather the result of the recruitment of preexisting interarterial connections. When successful, the majority of patients with successful CTO recanalization can expect significant reduction or complete resolution of anginal symptoms. In a sample of 10 studies involving 829 patients total, Puma et al found symptom relief is 70% for patients who experienced successful recanalization of the CTO vs only 31% when the attempt was unsuccessful.
The second condition to consider is the presence of viable myocardium. Recovery of left ventricular function in chronically ischemic myocardium depends on the presence of hibernating viable myocardium. In a cohort of 97 patients with CTO, Sirnes et al demonstrated that successful recanalization improved left ventricular ejection fraction by 8.1% (rising from 62% to 67%), with the greatest improvement of 10% occurring in those patients with left anterior descending artery disease.14 Additionally, they showed that the Wall Motion Severity Index (WMSI), a marker of global left ventricular dysfunction, also increased after CTO recanalization. The WMSI is obtained by averaging the wall motion of all the individual (analyzable) myocardial segments (values: –1 = dyskinesis, 0 = akinesis, 1 = hypokinesis, and 2 = normal).15 It is notable that the history of MI, the duration of an occlusion, and the incidence of a non-occlusive restenosis had no influence on left ventricular recovery, whereas reocclusion did have an adverse influence.13
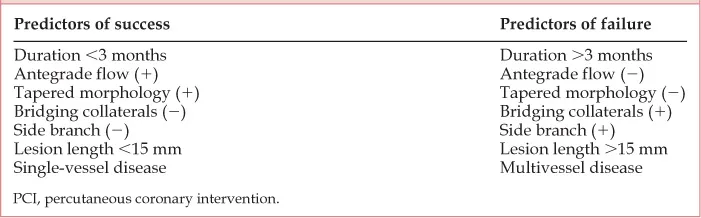
Finally, the probability of success should steer an operator towards performing PCI in a CTO when the likelihood of success is moderate to high (more than 60%) and the likelihood of complications is low (i.e. anticipated risk of death <1% and MI <5%).16 Should the PCI attempt prove unsuccessful, further management will depend on the symptomatic status and the extent of jeopardized ischemic myocardium. The operator should therefore be very familiar with the predictors of success when performing PCI of a CTO. Although each condition in Table 1.1 is an independent predictor of success or failure, several factors typically coexist.
Bridging collaterals, which are well-developed vasa vasorum unique to CTO lesions, are proportional to the duration of the CTO and therefore are more common in lesions older than 3 months. If antegrade flow is observed beyond the CTO, it is essential to differentiate the cause as microchannels in the true lumen vs perivascular bridging collaterals: the first is a predictor of success and defines a functional CTO (no longer considered a ‘true’ CTO), the latter is a predictor of an unsuccessful procedure. The distinction can usually be made by obtaining multiple angiographic projections of the occlusion; however, it sometimes only becomes apparent at the time of PCI. Extensive bridging collaterals that form a ‘caput medusae’ around the occluded vessel are generally unsuitable for PCI due to the very low success rate as well as high complication rate from perforation of the fragile small collateral vessels. However, these classic unfavorable features may no longer constitute unsurpassable hurdles with the employment of the innovative technical approaches described in later chapters of this book. Indeed, several experienced operators consider the absence of avisible distal vessel as the only contraindication to a CTO attempt.
Table 1.1 Predictors of success and failure in PCI of CTO
In patients with multivessel disease and one or more CTO lesions, the following conditions suggest careful consideration of referral to bypass surgery in place of attempting PCI: left main stem disease or occluded proximal left anterior descending artery supplying a viable anterior wall, complex triple vessel disease and insulin-requiring diabetes mellitus; severe left ventricular dysfunction; chronic kidney disease. Finally, multiple CTOs with low probability of success or high probability of complication should be treated surgically.
Specifically for patients after a myocardial infarction, two recent trials examined the older concept of “open-artery hypothesis.” According to their results,17–18 sustained potency of an occluded artery can be achieved successfully with percutaneous revascularization. However, in a population that is clinically stable (without significant ischemia of heart failure) and without residual myocardial viability who are submitted to PCI of an occluded artery at least 3 days post-infarction, the revascularization did not seem to confer clinically measurable benefit.
General Approach
Despite the outlined reservations, there has been a gradual increase in technical and procedural success rates for percutaneou...