- 318 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
About this book
Wound Healing Biomaterials: Volume One, Therapies and Regeneration discusses the types of wounds associated with trauma, illness, or surgery that can sometimes be extremely complex and difficult to heal.
Consequently, there is a prominent drive for scientists and clinicians to find methods to heal these types of wounds, with science increasingly turning towards biomaterials to address these challenges. Much research is now concerned with new therapies, regeneration methods, and biomaterials to assist in wound healing and healing response.
This book provides readers with a comprehensive review of the fundamentals and advances in the field of wound healing with regard to therapies and tissue regeneration. Chapters in Part One discuss fundamentals and strategies of wound healing, while Part Two reviews gene, stem cell, and drug delivery therapies for wound healing. Final chapters look at tissue regeneration strategies, making this an all-encompassing book on the topic of wound care and biomaterials.
- Provides more systematic and comprehensive coverage of specific therapies and biomaterials for wound healing
- Highlights research that is concerned with new therapies, regeneration methods, and the use of biomaterials to assist in wound healing and healing response
- Presents an organized layout of the material that is carefully arranged with clear titles and comprehensive section headings
- Looks at tissue regeneration strategies, making this an all encompassing book on the topic of wound care
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Wound Healing Biomaterials - Volume 1 by Magnus Ågren in PDF and/or ePUB format, as well as other popular books in Medicine & Medical Technology & Supplies. We have over one million books available in our catalogue for you to explore.
Information
Part One
Fundamentals and strategies for wound healing
1
Wound healing
S. Tejiram1, S.L. Kavalukas2, J.W. Shupp1, and A. Barbul2 1MedStar Washington Hospital Center, Washington, DC, United States 2Vanderbilt University Medical Center, Nashville, TN, United States
Abstract
Repair of an injured organ depends upon a complex physiologic process involving inflammatory cell migration, cytokine production, extracellular matrix deposition, and scar remodeling. Wound healing can be divided into four general phases that include hemostasis, an inflammatory response, remodeling, and maturation. There are a variety of wound types, both acute and chronic, that require their own specific method of treatment. The resulting scars that form include hypertrophic and keloid scars that require a wide variety of treatment modalities. A burn injury represents a special kind of injury and wound healing that requires a multidisciplinary approach to management. Finally, this work looks at current animal models and wound types used in research to explore and discover new treatment modalities, including novel biomaterials, and strategies.
Keywords
Animal model; Burn; Scar; Scar treatments; Thermal injury; Wound healing; Wound types1.1. Introduction
Mammals are generally incapable of tissue regeneration, so repair of an injured organ depends upon a complex process that involves inflammatory cell migration and cytokine actions, collagen and extracellular matrix deposition, and scar remodeling. With few exceptions, all wound healing results in the formation of scar. The process of wound repair differs little from one tissue to another and is generally independent of the nature of the injury. A number of elaborate and redundant mechanisms that complement one another facilitate healing and drive the wound healing process forward.
1.2. Skin layers
The skin represents one of the largest organs of the body whose key roles include protection against outside pathogens and excessive water loss. The skin is comprised of three layers: the epidermis, dermis, and subcutaneous layer (hypodermis) (Fig. 1.1). The epidermis is the top layer of the skin and produces keratin that makes up the outermost physical barrier and the pigment melanin for ultraviolet (UV) radiation protection. It is the foremost layer involved in barrier protection against the outside environment through tight junctions and Langerhans cells. The dermis contains the papillary and reticular dermis and houses the skin appendages hair follicles, sebaceous glands and sweat glands necessary for tissue regeneration. The hypodermis is the bottom layer of skin that serves to attach the dermis to muscles and bones, houses blood vessels and nerves, and helps control body temperature.
1.3. Phases of wound healing
Injury starts a complex cascade of cellular and biochemical events, resulting in a healed wound. The wound healing response can be divided into four separate, but overlapping, phases: hemostasis and inflammation, proliferation, maturation and remodeling, and wound contraction.
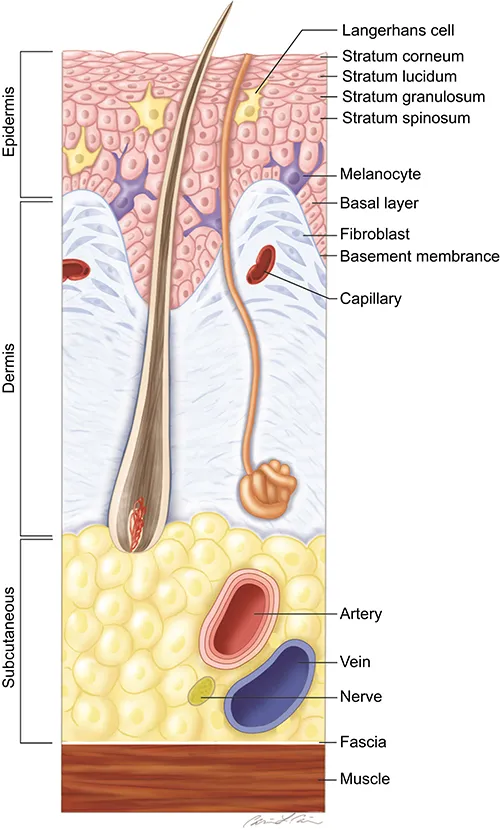
Figure 1.1 Anatomy of the skin depicting the important histological zones, skin structures, dermal appendages, and cell types comprising the layers of skin. Adapted from Shupp JW, et al. A review of the local pathophysiologic bases of burn wound progression. J Burn Care Res 2010;31(6):849–73.
1.3.1. Hemostasis and inflammation
Hemostasis precedes inflammation. The rupture of vessels that accompanies injury exposes the subendothelial collagen to platelets, which leads to the aggregation and activation of the coagulation cascade. The contact between collagen and platelets as well as the presence of thrombin, fibronectin, and their fragments results in the release of cytokines and growth factors from platelet α-granules, such as platelet-derived growth factor (PDGF), transforming growth factor (TGF)-β, platelet activating factor, fibronectin, and serotonin. The locally formed fibrin clot serves as a scaffold for migrating cells such as neutrophils, monocytes, fibroblasts, and endothelial cells (Fig. 1.2).
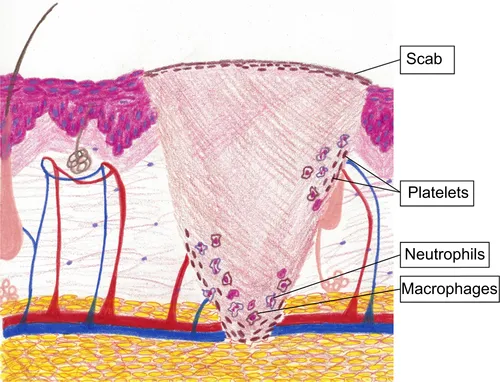
Figure 1.2 Schematic drawing depicting a full-thickness wound into hypodermis. Note the initial arrival of platelets to achieve hemostasis as well as neutrophils and macrophages to the healing-wound bed. The contact between collagen and platelets results in the release of cytokines and growth factors that ultimately provide chemotaxis for neutrophils, monocytes, fibroblasts, and more. Illustration by Katherine R. Parrish, ACNP, CNS
The inflammatory phase is characterized by increased vascular permeability, chemotaxis of cells from the circulation into the wound milieu, the local release of cytokines and growth factors, and the activation of migrating cells. Within 6 h of injury, circulating immune cells migrate into the wound. Neutrophils are the first blood leukocytes to enter the wound site, and their numbers peak at 24–48 h after injury. Increased vascular permeability caused by inflammation and the release of prostaglandin, together with a concentration gradient of chemotactic substances such as complement factors, interleukin (IL)-1, tumor necrosis factor (TNF)-α, TGF-β, platelet factor-4, and bacterial products, stimulate neutrophil migration. The main function of the neutrophils is phagocytosis of bacteria and tissue debris. The presence of neutrophils is not essential for healing to take place, provided that bacterial contamination has not occurred [1]. Macrophages, derived from circulating monocytes, migrate next within the wound and peak by day 3 after injury. Wound macrophages have a much longer life span than the neutrophils and persist in the wound until healing is complete. Macrophages play a central role in the orchestration of the wound healing cascade. Their appearance is followed by lymphocytes, which occur in significant numbers around the fifth day after injury. In contrast to neutrophils, the presence and activation of both macrophages and lymphocytes in the wound is critical to the progression of the normal healing process (Fig. 1.3(a)) [2–4].
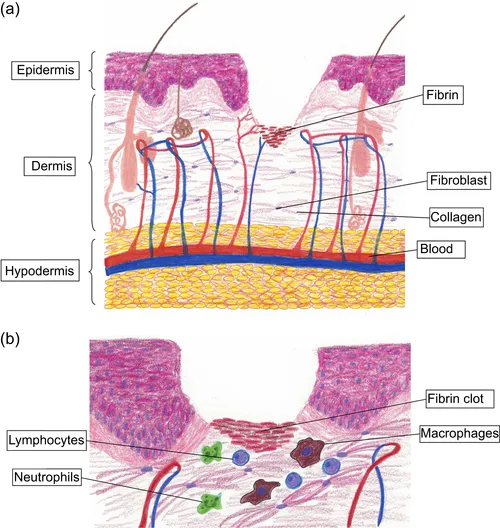
Figure 1.3 Schematic drawing of a partial-thickness wound in the inflammatory phase. (a) Each layer of the skin contributes to the wound healing process and associated extracellular matrix production. (b) Close-up of the wound bed depicting the arrival of neutrophils, macrophages, and lymphocytes to the wound bed. The fibrin clot helps achieve hemostasis while providing chemotaxis for the cells necessary to begin the wound healing process. Illustration by Katherine R. Parrish, ACNP, CNS
Chemotaxis of cells into the wound milieu is followed by cellular activation, which signifies the phenotypic alteration of cellular, biochemical, and functional properties induced by local mediators (Fig. 1.3(b)). Although neutrophils, macrophages, and lymphocytes predominate during inflammation, the contribution of each cell population to successful wound healing is variable.
The activation of macrophages has fundamental implications in several aspects of wound healing, such as debridement, matrix synthesis, and angiogenesis. The initial and brief release of factors from platelets is a first and strong stimulus of macrophage activation. Activated macrophages release cytokines that mediate angiogenesis, fibroplasia [5], and nitric oxide (NO) synthesis, which itself has antimicrobial properties and stimulates collagen synthesis [6,7]. Macrophages evolve phenotypically as healing progresses, switching from NO synthesis and inflammatory function to arginase expression and more synthetic functions [8]. The inflammatory phase of healing is vital to the proper evolution of subsequent wound healing phases. Reduced inflammatory responses profoundly affect subsequent hea...
Table of contents
- Cover image
- Title page
- Table of Contents
- Related titles
- Copyright
- List of contributors
- Woodhead Publishing Series in Biomaterials
- Part One. Fundamentals and strategies for wound healing
- Part Two. Therapeutics and tissue regeneration for wound healing
- Index