eBook - ePub
Case Studies in Clinical Cardiac Electrophysiology E-Book
John M. Miller, Mithilesh K. Das, Douglas P. Zipes
This is a test
Share book
- 800 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Case Studies in Clinical Cardiac Electrophysiology E-Book
John M. Miller, Mithilesh K. Das, Douglas P. Zipes
Book details
Book preview
Table of contents
Citations
About This Book
Keeping up with the use of new technologies in cardiology is becoming increasingly challenging. Case Studies in Clinical Cardiac Electrophysiology helps to bridge the gap between knowledge and application with 28 cases spanning both common and uncommon arrhythmias and ablation scenarios, each of which includes the clinical presentation, baseline ECG, ECG during arrhythmia, stepwise electrophysiologic diagnostic maneuvers and some of their pitfalls, and optimal therapy.
- Includes 28 cases spanning the spectrum of what an electrophysiologist is likely to see in practice.
- Shows the correct way of conducting procedures, as well as "detours" that an unwary practitioner may take: misdiagnoses and why they are wrong; incorrect therapeutic choices and why these may be not only unsuccessful but even harmful.
- Encourages you to read and interpret the ECGs, mapping diagrams, and other diagnostic information before revealing the expert opinion or actual results of each case.
- Summarizes the key learning points in each case.
- Discusses potential procedural complications, including anticipation, avoidance, recognition, and response and resolution.
- Covers complex ablations (atrial fibrillation, ventricular tachycardia) as well as prior failed ablations.
Frequently asked questions
How do I cancel my subscription?
Can/how do I download books?
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
What is the difference between the pricing plans?
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
What is Perlego?
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Do you support text-to-speech?
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Is Case Studies in Clinical Cardiac Electrophysiology E-Book an online PDF/ePUB?
Yes, you can access Case Studies in Clinical Cardiac Electrophysiology E-Book by John M. Miller, Mithilesh K. Das, Douglas P. Zipes in PDF and/or ePUB format, as well as other popular books in Medicina & Cardiologia. We have over one million books available in our catalogue for you to explore.
Information
Topic
MedicinaSubtopic
CardiologiaPART 1
Sinus Node, AV Node, and His-Purkinje System
Outline
1. Sinus node and atrioventricular conduction disease
Chapter 1
Sinus node and atrioventricular conduction disease
Case presentation
A 56-year-old man experienced syncope while walking at work. Coworkers called emergency medical services (EMS). Upon the arrival of EMS, he was awake and feeling normal but was convinced to go to the emergency room (ER). The patient had a history of anterior wall myocardial infarction (MI), percutaneous coronary intervention (PCI), to left anterior descending coronary artery (LAD) several years before, and a negative stress test within the last 6 months. Examination results were normal except for obesity. ECG showed sinus rhythm, long PR, right bundle branch block (RBBB), left anterior fascicular block (LAFB), and anterior scar. Echocardiogram revealed ejection fraction (EF) 40% and anterior hypokinesis. The patient was referred for electrophysiology (EP) study.
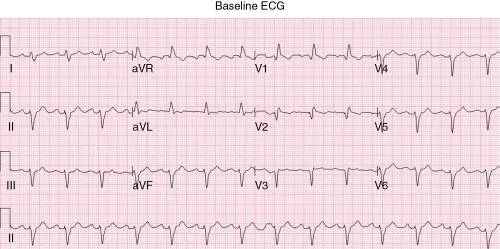
The ECG in Fig. 1-1 shows sinus rhythm with a prolonged P wave (left atrial abnormality), slightly prolonged PR interval, RBBB and left anterior fascicular block, and an extensive anterior infarction. On the basis of this, there are many possible causes of syncope—atrial arrhythmias (atrial flutter and fibrillation, other reentrant atrial tachycardias), heart block (either in AV node or His-Purkinje system), or ventricular arrhythmia (ventricular tachycardia or fibrillation). There is nothing in the ECG to favor one cause of syncope over another, and because treatment strategies are very different depending on the cause (medications or ablation for atrial arrhythmias; pacemaker for heart block; implantable defibrillator for ventricular arrhythmias), further investigation is needed.
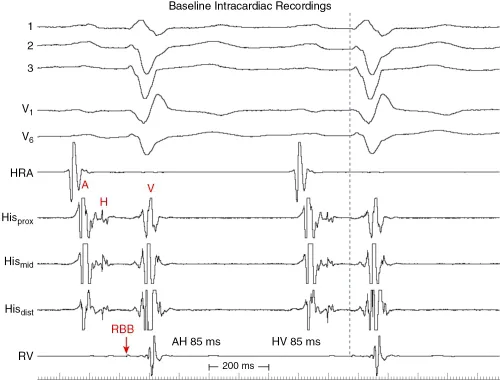
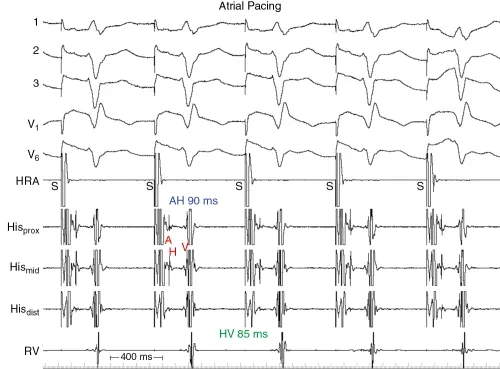
Evaluation
Intracardiac recordings during sinus rhythm (Fig. 1-2) show atrial (A), His (H), and ventricular (V) recordings as noted. This confirms the presence of His-Purkinje disease, with an HV interval of 85 ms—prolonged (normal, 40 to 55 ms), but not enough to implicate His-Purkinje dysfunction as a cause of heart block. Surprisingly, though the PR interval is somewhat prolonged, the AH interval is normal (85 ms [normal, 60 to 125 ms]). Usually, prolongation of the PR interval is caused by the AV nodal (AH) component, because to prolong the PR even 60 ms from His-Purkinje disease would require a lengthening of the HV to a degree (that is, from 40 ms to 100 ms) that 1:1 conduction would be unlikely. Note also that there is a delay between the distal His recording and right bundle branch (RBB)—there is usually <10 ms between these—and that the RBBB is further caused by delay or block between the RBB and RV apical electrogram, with a QRS onset (dashed blue line) to RV electrogram of 75 ms (normal, 10 to 35 ms).
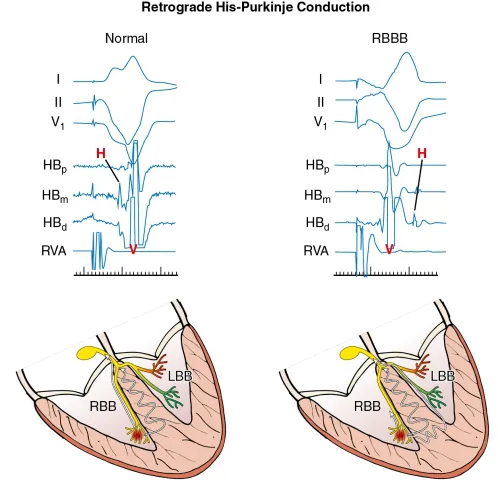
The left side of Fig. 1-3 shows a sinus rhythm complex as in the previous figure for reference, whereas the 2 complexes on the right are during pacing from the right ventricular apical region. Note that there is retrograde conduction to the atria, with the His bundle activated from distal to proximal as expected. Usually, the timing of the His potential is before the local ventricular electrogram in the His recoding, because conduction proceeds more rapidly up the RBB to the His than does muscle-to-muscle propagation from apex to base. Because there is RBBB in this case, the impulse cannot ascend the RBB as it normally would and instead must traverse the interventricular septum, enter the left bundle branch, and then activate the His retrogradely. These findings just confirm the His-Purkinje disease but give no further insight as to the cause of syncope.
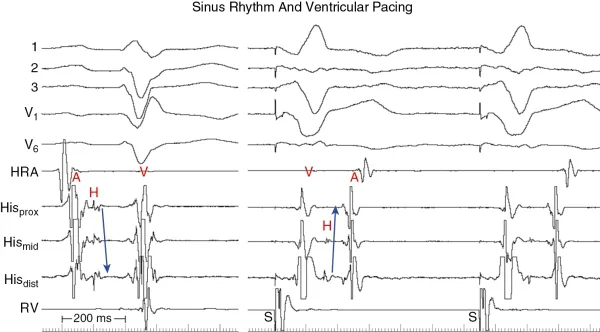
As illustrated in Fig. 1-4, in patients with normal His-Purkinje function (at left), pacing from the right ventricular apex (red circle) results in retrograde conduction over the RBB (white line) that is more rapid than muscle-to-muscle conduction (wavy line in septum), resulting in a His potential (H) inscribed before the larger local ventricular recording (V). At right, in the presence of anterograde RBBB, the paced wavefront cannot ascend the blocked right bundle and instead crosses the interventricular septum (wavy horizontal line) to engage the left bundle, and then proceeds rapidly to the His that now appears after the local ventricular recording (that is again generated after muscle-to-muscle spread).
Rapid pacing can often reveal abnormalities of AV conduction that were not very evident at rest. In Fig. 1-5, pacing the atrium (S) slightly faster than the sinus rate shows minimal change in either AH (90 ms) or HV (85 ms) intervals. It is useful to display multiple electrode pairs of His recordings because the signal amplitude may vary enough between complexes that the His potential may be poorly visible or even absent in one electrode pair (Hisdist in this case), whereas it is readily visible in other electrode pairs.
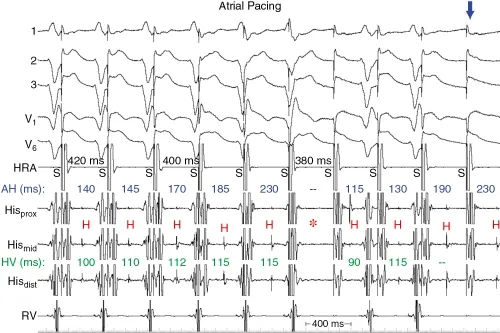
More rapid pacing starts to reveal some abnormalities. As the pacing rate increases (cycle length decreases), the AH is expected to prolong but the HV interval usually remains constant. In Fig. 1-6, the AH (in blue) does prolong, but so does the HV interval (in green). The asterisk denotes where AV nodal block occurs (no subsequent His potential), but three cycles after this, there is a His potential not followed by a QRS (infra-His block; green dash) and the HV intervals on the prior two cycles had prolonged (thus, infra-His Wenckebach). This is distinctly abnormal and likely warrants pacemaker implantation. However, this may not be the reason that syncope had occurred (there may be other abnormalities that have not yet been uncovered during the study).
In Fig. 1-7, pacing is repeated for 1 min at the same cycle lengt...