Clinical Dilemmas in Diabetes
Adrian Vella, Adrian Vella
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Clinical Dilemmas in Diabetes
Adrian Vella, Adrian Vella
About This Book
Clinical Dilemmas in Diabetes answers the clinical questions commonly encountered when diagnosing, treating, and managing patients with diabetes and its associated complications. Designed to support informed, evidence-based care, this authoritative clinical guide includes contributions from leading endocrinologists and diabetes researchers that discuss a diverse range of recent developments. Concise and focused chapters cover prediabetes, diabetes diagnosis, initial evaluation and management, disease complications, and cardiovascular disease and risk factors.
Now in its second edition, Clinical Dilemmas in Diabetes contains extensively reviewed and revised information throughout. New and updated chapters examine prediction, diagnosis, and management of early Type 1 diabetes, ophthalmic complications, screening asymptomatic patients for cardiovascular disease, new agents for treatment of dyslipidemia, closed loop systems in Type 1 diabetes, upper gastrointestinal manifestations, managing hyperglycemia in critically ill patients, and more. Edited by Dr. Vella at the Mayo Clinic, this highly practical resource:
- Encourages evidence-based clinical decision-making, rather than algorithm-based approaches
- Provides clear guidance on common problematic areas, especially in cases where conflicts in treatment for the disease and the complications occur
- Emphasizes the importance of translating the results of clinical trials to individual care and management of diabetes
- Contains effective learning and revision tools, including Learning Points, chapter introductions and summaries, tables and figures, color diagrams and charts, and full references
Part of the popular Clinical Dilemmas series, Clinical Dilemmas in Diabetes is a must-have guide for anyone involved in the treatment of patients with diabetes, particularly endocrinologists, diabetes specialists and consultants, cardiologists, residents, fellows, specialist nurses, and general practitioners with an interest in diabetes.
Frequently asked questions
Information
PART I
Prediabetes and the Diagnosis of Diabetes
1
“Is Prediabetes a Risk Factor or Is It a Disease?”
LEARNING POINTS
- Prediabetes is a heterogeneous condition with variable risk of progression to type 2 diabetes
- In addition to diabetes risk, it is associated with an increased risk of vascular disease.
- To date, lifestyle modification is the single most important tool for altering the natural history of prediabetes and progression to type 2 diabetes.
What is prediabetes?
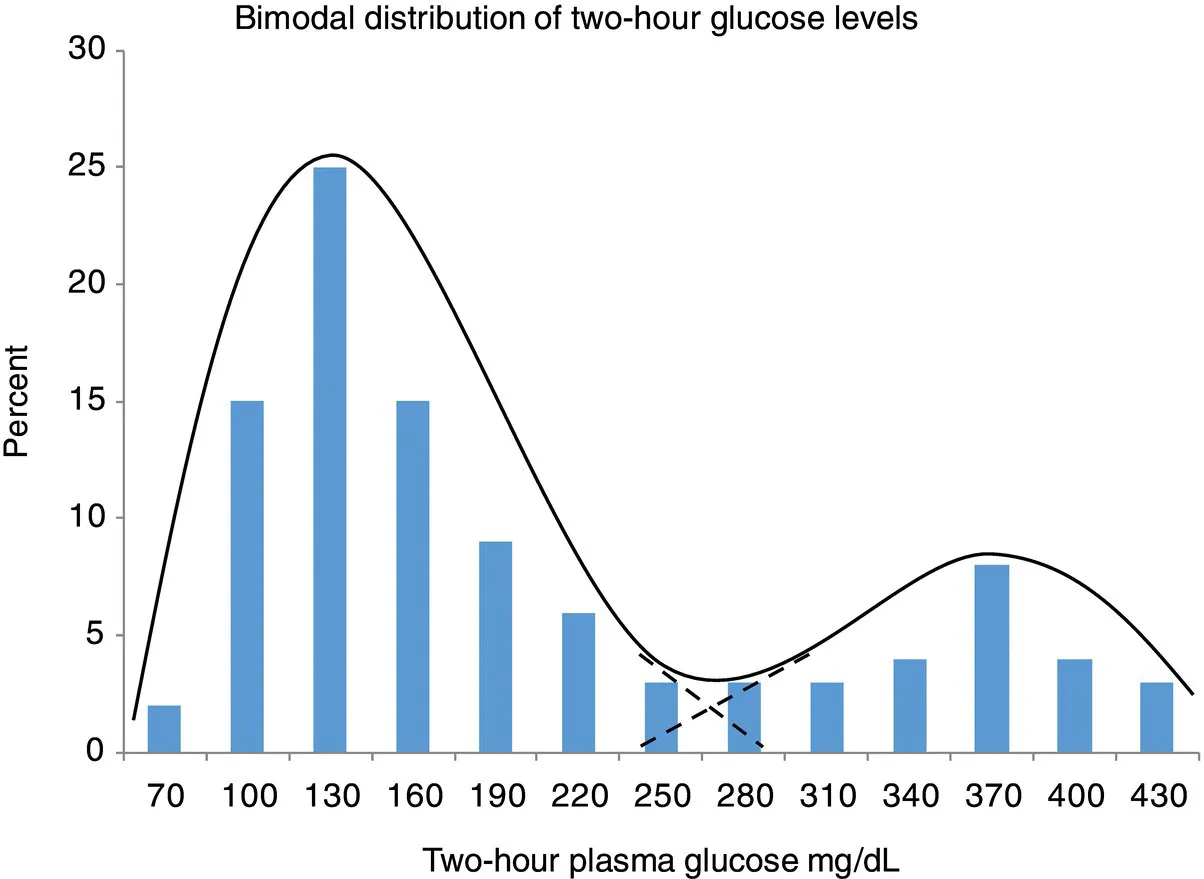
Rationale for the diagnostic criteria for diabetes mellitus and prediabetes