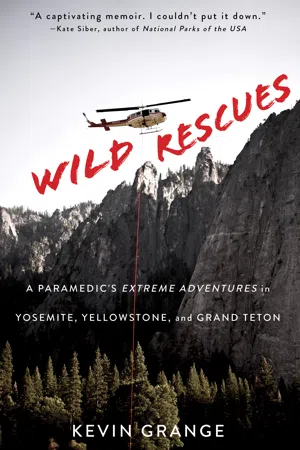
![]()
PART I
I went to the woods because I wished to live deliberately, to front only the essential facts of life, and see if I could not learn what it had to teach, and not, when I came to die, discover that I had not lived.
—Henry David Thoreau, Walden
![]()
1
THE DEFINITION OF INSANITY
MY WILD ADVENTURE with the National Park Service began long before that traumatic cardiac arrest call in California’s Yosemite National Park. The first national park I worked at was Yellowstone, which occupies parts of Wyoming, Idaho, and Montana. I arrived there from Los Angeles during a snowstorm in early May 2014. (Yes, they have snowstorms up there even in May.) I hadn’t even stepped out of my car before the first 9-1-1 call came in. As I parked in front of the Old Faithful Ranger Station, the apparatus bay opened, and the ambulance slowly emerged, its emergency lights turning the white snow globe that surrounded me red and blue.
Spotting my California plates in the near-empty parking lot, the driver rolled down the window and gestured. “You must be the new paramedic,” she yelled above the squall. “We have a call!”
Was this an invitation? Or a warning about the busy summer that awaited me? Either way, I quickly parked and sprinted to the ambulance, hopping in the back.
“I’m Kevin,” I hollered as we drove.
“Emily,” the driver said loudly, glancing in the rearview mirror. “And this is Cody!”
Emily Wilde worked as Old Faithful’s fire officer. She was in her early thirties, with brown hair, freckles, and a friendly smile. Cody Riley, a grizzled guy in his late forties, sat in the front seat next to her.
The rest of our introductions would have to wait. There was a sixty-eight-year-old woman with dizziness and a racing heart at the visitor center who needed our help.
“I’ll take lead,” Cody said, pulling on a pair of blue exam gloves. “Emily will get a set of vital signs, and I want you to place the patient on the cardiac monitor so we can look at her EKG.”
“Copy,” I replied, catching my reflected smile in the side window. I was about to run my first call in a national park and couldn’t have been happier. Months earlier, I had been working on an ambulance in Compton, California, and my life was at a dead end.
After working for years in the restaurant and real estate industries, I’d signed up for an EMT class at age thirty-five, hoping to help people in a more direct and meaningful way. An EMT certification was the bare minimum for someone operating on an ambulance, and the class consisted of 120 hours of instruction in providing basic life support on emergency calls that ranged from broken bones and cuts to diabetic emergencies, heart attacks, strokes, and cardiac arrest.
From the moment I walked into my first EMT class, I knew I’d found my calling. I loved everything about prehospital medicine—the challenge and unpredictability, the unique blending of critical thinking with practical skills, the team-based approach, and of course, running all the crazy calls and helping people. Hoping to deepen my knowledge base—and become certified to operate at the highest level—I attended UCLA’s Paramedic Education Program. Paramedic school was 1,500 hours of didactic instruction, written exams, high-stress skills stations, and a grueling field internship with a local fire department or EMS agency that many students described as “the best time in my life that I’d never want to repeat again.” Along with basic life support, as paramedics we were trained to provide advanced life support by placing IVs, inserting breathing tubes, administering dozens of medications, and using a cardiac monitor to speed up, slow down, or restart a patient’s dying heart.
I’d assumed things would get easier after attending paramedic school—the hardest physical and mental thing I’d ever done—but as soon as I stepped off the graduation podium, I’d taken my place at the back of a long, serpentine hiring line composed of thousands of men and women who, like me, sought firefighter paramedic jobs in Los Angeles. I hadn’t prepared at all for the hiring process to be so competitive—or to take such a long time. There were over ten thousand applicants when I applied to the Los Angeles Fire Department for an initial recruit class of seventy firefighters, and the hiring cycle took months.
With no other options, I accepted a paramedic job with a private ambulance company in Compton. Our headquarters was located on Kona Drive, just off Mahalo Place. The street names brought to mind Maui’s sunny beaches and bottomless mai tais, but I quickly learned that in reality, it was merely a drab area of industrial buildings. And when you took a right on Central Avenue and crossed over the 91 Freeway, the Compton I’d long heard about on rap albums emerged: single family homes with barred windows, liquor stores, and gang graffiti along palm-tree-lined streets like Crenshaw, Slauson, and Rosecrans Avenue—as famous (and notorious) as the hip-hop artists who sang about them.
“Just don’t get out of the ambulance alone,” my partner warned.
At the private ambulance company, we occasionally provided mutual aid and 9-1-1 response for the Compton Fire Department—when gang life got “hot” and the number of patients exceeded their supply of ambulances—but mainly we handled simple transports, like taking patients from nursing facilities to dialysis clinics, convalescent homes to community hospitals, or halfway houses to psychiatric wards.
While I enjoyed helping people and interacting with my patients, the hours were long, the pay was low, and the scene was never safe. My partner and I were often sent alone into LA’s worst neighborhoods, where our dark blue uniforms and silver badges made us look a lot like cops. Our back muscles strained and tore from struggling to lift morbidly obese patients with a team of two, and we were routinely exposed to methicillin-resistant Staphylococcus aureus (MRSA), clostridium difficile (C-diff), feces, and scabies, microscopic bugs that lay eggs in the upper layer of skin. Nurses would send us into patient rooms, claiming we didn’t need any isolation precautions, but then arrive at the bedsides after us wearing protective gowns, gloves, face masks, safety glasses, and surgical caps.
We picked up schizophrenic patients on involuntary psychiatric holds—threatening to kill themselves and others—along with tattooed prisoners from Twin Towers Jail downtown, the largest correctional facility in the world. Once we arrived at one of the rundown community hospitals where we transported our patients, we often had to wait for hours in the hallway to get a bed. “Holding up the wall” with a patient for hours at a time was common; my record was seven hours, on one particularly busy Monday.
In between transports, we waited for the next assignment by “posting” our ambulance in empty lots and city parks frequented by prostitutes and drug dealers. In addition to the tedium, since I wasn’t running 9-1-1 calls anymore, I wasn’t using the full extent of the training that I’d received at UCLA, and I feared I was losing the quick and efficient patient assessment skills I’d worked so hard to achieve.
Along with having a crappy ambulance gig, I was also broke. The fire department jobs for which I was applying required me to make—and pay for—repeated trips across the country for written exams, work capacity tests, interviews, polygraphs, and drug tests. And as if that all wasn’t enough, my girlfriend, Chantal, broke up with me. My job difficulties reminded her too much of her deadbeat ex-husband, she said, and she’d lost respect for me.
Chantal had slammed the door in my face, refusing to talk, and then assumed a cross-legged seat on her yoga mat and started chanting for the peace and happiness of all sentient beings.
“Please, Chantal,” I’d pleaded. “Just let me back in.”
“Ommmmmmmm … Ommmmmmmm … Ommmmmmmm …”
“We can work this out!” I said.
“Ommmmmmmm … Ommmmmmmm … Ommmmmmmm …”
In short, I was at a low point in my existence, both personally and professionally. My life felt like the standstill traffic on the 405 Freeway.
But everything changed one November morning with the sound of snow chains.
I was camping with my parents in California’s Yosemite National Park. An unexpected snowstorm had blanketed the Sierras, so we were relaxing in our RV, sipping coffee, and playing cards while admiring the Narnia-like snowy splendor that surrounded us. I’d just laid down three aces in a game of gin rummy when I heard the hum of a diesel engine and the rattle of snow chains hanging off a rear axle. I looked out the window and spotted an ambulance, painted white with a forest-green stripe, belonging to the National Park Service. The park ranger, a handsome guy in his late twenties, smiled and waved. He was a shepherd, checking in on his flock after the freak snowstorm. I waved back and he continued on.
Until that moment, it had never dawned on me that there were paramedics serving in our national parks, responding to medical and traumatic emergencies in some of the most remote and wild parts of the United States. However, given the isolation, dangerous terrain, inclement weather, and abundance of things that bite, claw, and sting, it certainly made sense.
“Now there’s a job you should get,” my dad said.
I couldn’t believe I hadn’t thought of it myself.
Although I was living in Southern California at the time, I’d grown up on forty-six acres in New Hampshire. Family camping trips were a staple of my childhood, and I’d once dreamed of being a ranger after encountering one in Moose Brook State Park when he’d stopped by our tent to politely ask us to quiet our laughter since it was after 10:00 pm.
Questions immediately fluttered around in my mind. What kind of emergencies did a national park paramedic run? How was it working in a wild, remote area with the closest hospital hours away? Running an emergency call with limited personnel?
I suspected there was a whole new side of the paramedic profession I hadn’t yet witnessed.
“I’d love to work here,” I exclaimed.
I needed a change. Working for the private ambulance service and applying to fire departments in Los Angeles and elsewhere felt like an endless treadmill of disappointment, and working for the National Park Service seemed like an ideal reset button.
“It’s the perfect plan,” I told my parents. “I’ll do a season with the Park Service while I’m waiting to get hired by a department in LA.”
In the weeks that followed, I researched emergency medical services with the NPS. With over four hundred units in the National Park System, spread out across our country like natural, cultural, and historical diamonds, I discovered EMS was handled quite differently at each. The smaller park units (such as historic sites, national seashores, monuments, and preserves) typically delegated fire and EMS response to outside agencies serving the gateway towns that bordered them. But the bigger parks—like the Grand Canyon, Lake Mead, Mount Rainier, or the Great Smoky Mountains—had robust fire, EMS, and search-and-rescue programs and operated their own ambulances, staffed by rangers who were EMTs and paramedics, or park medics, a variation of the two.
The certification levels for EMS providers were an ever-evolving and often confusing subject. In brief, emergency medical technicians could provide basic life support (BLS) interventions like controlling bleeding, splinting, operating an automatic external defibrillator, providing oxygen, and assisting with medications like aspirin for a heart attack, glucose for a diabetic patient with low blood sugar, or epinephrine for a bad allergic reaction. Along with BLS care, advanced life support providers such as NPS park medics and paramedics could insert a breathing tube down a patient’s windpipe, start IVs, use a cardiac monitor to treat abnormal heart rhythms, and administer dozens of medications.
Most of the paramedic jobs with the NPS were summer seasonal positions starting in May and lasting into October. If candidates performed well, they were eligible for rehire status and often hired to work at other parks. The NPS was like the Mob in that way: once you were in, you were in.
As I read about the positions, I could barely contain my excite...