eBook - ePub
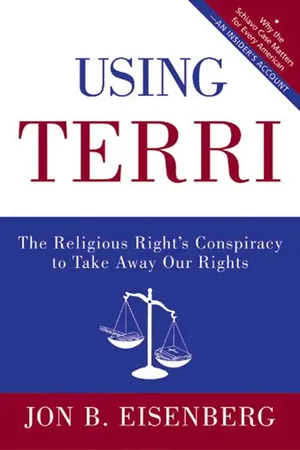
Using Terri
Lessons from the Terri Schiavo Case and How to Stop It from Happening Again
- 304 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Using Terri
Lessons from the Terri Schiavo Case and How to Stop It from Happening Again
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
PART ONE
Whence It Came
1
My Cousin Ros
I joined Michael Schiavo’s legal team in March 2005 because I understood well his painful task. It is not easy to “pull the plug” on someone you love. I know from personal experience.
In 1998, my cousin Roslyn August suffered a devastating stroke that left her with what doctors called “global aphasia.” As one of them put it, “Nothing is getting through to her, and nothing can come out.” I spent days at her bedside trying to communicate. I held her hand and asked her to squeeze it. Nothing. I told her to blink if she could hear me. Nothing. I kissed her cheek. Nothing.
Yet she was not in a coma. Her eyes were often open, and sometimes they tracked me as I crossed the room. She seemed lost somewhere between life and death.
On one visit to her bedside, I brought my favorite photograph of her. The photographer had caught her standing in a grove of trees at the base of Yosemite Falls wearing a big, silly grin, facing upward with her arms held up to the sky, as if to say, “How lovely!” I handed her the photograph. She took it in one hand, seemed to look at it uncomprehendingly, and then dropped it and went blank again.
Was she in a persistent vegetative state? None of the doctors ever said. Was she in a minimally conscious state? That diagnosis did not yet even exist. Could she improve? This the doctors could tell me: no. There was nothing they could do.
Except for one thing: They could keep her alive with a feeding tube inserted through her nose into her stomach.
Ros was seventy-nine years old and had been in failing physical and mental health for three years. She was my second cousin once removed: her great-grandparents were my great-great-grandparents. But she was more like a favorite aunt to me than a distant cousin. She had been part of my innermost family circle since my early childhood, and we became good friends in my adult years. The only other relatives with whom Ros had regular contact were a brother in New York City, a niece in San Francisco, and my parents and grandmother in Los Angeles. Ros lived alone in a one-room apartment in Oakland, California—just a few miles from me and my wife, Linda Hillel—subsisting on a small government pension.
Ros often had Linda and me over for dinner. Her cooking was…well, not so hot. But she did one thing superbly—the Spanish seafood and rice dish, paella. And she was great company. Dinner with Ros was fun.
Ros was a free spirit. She had been married briefly in her youth, and after that she knocked around for years before settling down in Northern California and putting herself through college and graduate school, from which she emerged with a masters degree in social work. She became a psychiatric social worker, employed by a county agency to evaluate mentally disturbed people for government conservator-ships. She came to know intimately the world of mental institutions and nursing homes.
Ros retired in her early sixties. She kept close friends. She cultivated many hobbies—weaving, stained glass, poetry, hiking. She traveled widely.
In her seventies, Ros began to slow down. Travel became more difficult. She grew impatient with friends. She became forgetful. She sometimes got lost during her goings about town, which frightened her terribly.
Over the years, our dinner conversations occasionally turned to the subject of death and dying. Ros said she did not want to be kept alive at all costs. We discussed the high-profile “right to die” cases of the day —Karen Ann Quinlan, the New Jersey woman whose parents disconnected her respirator in 1976; Nancy Cruzan, the Missouri car accident victim whose 1990 case in the U.S. Supreme Court established the constitutional right to refuse tube feeding and other medical treatment; and several local cases that were widely publicized in California. Ros made her position clear: “No machines or tubes for me.”
Most Americans feel that way.
Ros even went so far as to get information from the Hemlock Society on how to end her life with drugs, which she planned to buy on a trip to Mexico.
From 1988 through 1996, Ros made several wills appointing me her executor. She had also given me legal power of attorney over her financial affairs should she become unable to handle them, and she executed several advance health-care directives naming me as her surrogate decision-maker. Her most recent health-care directive, on a form I had given her in 1996, said: “I do not want efforts made to prolong my life and I do not want life-sustaining treatment to be provided or continued” under any circumstances “where the burdens of the treatments outweigh the expected benefits.”
Ros gave me power over her life and death. But her health-care directive said nothing about feeding tubes. Back then, none of the standard form advance directives did so.
In the fall of 1997, Ros’s downhill progression advanced considerably. She became confused, incontinent, and reclusive. She began setting kitchen fires. One day I went to visit her and discovered smoke pouring from her open front door. She had left a skillet of hamburger meat on an open flame. The Oakland Fire Department came and extinguished the smoldering remains.
After a handful of fires, I had her oven disconnected and arranged for daily deliveries of meals-on-wheels from a senior services provider. She asked, “How am I going to make coffee?” I bought her an electric kettle.
I begged Ros to let me place her in an assisted living facility. She was adamantly against it, saying, “I’ve seen those places. I know what they’re like. I’m not ready yet.”
But she was oh-so-ready. She just didn’t realize it. Or couldn’t face it.
Eventually, Ros stopped eating. This was truly alarming, for food had become the central focus of her life, all she had left. She loved to eat, and she ate a lot. After her death, I discovered this entry in one of her journals: “I eat because I experience a lack of control over my world. Eating takes care of all feelings good or bad. It’s a safety net psychologically, a spontaneous impulse to eat to achieve control.” Control over her life—personal autonomy—meant a lot to Ros. She always knew and did what she wanted. Who wouldn’t want to live that way?
On December 24, 1997, I discovered Ros lying on the floor of her apartment, unable to move. She begged me not to call the paramedics, but of course I did. She spent twelve days in the hospital being treated for a severe urinary tract infection. I had her discharged to a skilled nursing facility. After some initial resistance, she agreed to it. There was no fight left in her.
Ros spent three weeks in the nursing home, lying in bed staring into space. She would not read—a lifelong passion—or even watch television. Once, when I caught her in a lucid moment and asked what she was thinking about, she responded, “How I can get out of here.”
On January 28, 1998, Ros had her stroke.
Within a few days, the doctors told me that Ros was profoundly brain-damaged. She would never again eat, read, communicate, or even think in any meaningful way. One of the doctors said that I might soon have to decide whether to withhold life-sustaining measures. Ros had been periodically pulling out her feeding tube, which the doctors reinserted. They might have to restrain her to keep it in.
I telephoned Ros’s brother Ted in New York and asked him to come to Oakland to help me decide. He and his wife arrived two days later. We had a meeting at the hospital—Ted, his wife, his daughter (the San Francisco niece), Linda and me, Ros’s attending physician, and a hospital chaplain. Then we five family members retreated to a local coffee shop, where we spent three hours of tearful agonizing and soul-searching before deciding to remove the tube for good. It was to come out that evening.
Late that night, however, a floor nurse telephoned me at home and said the nursing staff was “uncomfortable” with our decision to remove Ros’s feeding tube, and further action would be deferred until a meeting of the hospital’s ethics committee three days hence.
I had never heard of a hospital ethics committee. I learned that it’s typically an assemblage of doctors, nurses, lawyers, medical and law school professors, and clergy—as many as a dozen or more—who provide advice on ethical questions that arise in the practice of medicine, guided by a mélange of moral, philosophical, and legal principles called bioethics. These days, nearly all hospitals have an ethics committee. Given the nurses’ concerns, Ros’s attending physician wanted advice before removing the feeding tube.
I was to attend the meeting and make the case for withholding ANH—the doctors’ shorthand for artificial nutrition and hydration. Evidently Ros’s advance directive wasn’t good enough for the doctors, because it said nothing about her specific wishes and nothing about feeding tubes.
This was new to me. I have been a lawyer for twenty-six of my fifty-two years and have represented all sorts of clients—architects, engineers, and doctors; drunk drivers, bar fighters, and prostitutes; billion-dollar chemical and oil companies; and even a multiple murderer. But I had never represented Death.
At the meeting, I told the ethics committee about how Ros had lived her life and what she had said about death and dying. I explained how Linda and I had become Ros’s closest relatives and virtually her only remaining friends in her waning years; how I knew the life she had lived and the life she would not want to live; how she would abhor being kept alive in her current condition.
Linda and two of Ros’s old friends attended the meeting, too, and said similar things. Ted had returned to New York by then.
I told them how I had gone through Ros’s papers the day before the meeting and discovered a note in her handwriting with the address of the Hemlock Society in Los Angeles and what appeared to be a somewhat misspelled recipe for pharmaceutical suicide: “Norflex, orphenadrine, sliokol, barbiturates, morphine, 30–100 mg.”
Finally, I concluded: “I am now called upon to speak for Roslyn, who cannot speak for herself. I abhor the idea of speaking as Death’s lawyer. Let me speak instead in Ros’s voice. Here is what I think she would say: ‘I have lost my greatest joy in life—eating. There is an impenetrable wall between me and the people I love, for I can no longer speak to them. My greatest fear in life—institutionalization—has been realized. Please, leave me alone and let me go.’ ”
And that is what they decided to do.
The doctors told me it would take a week or two for Ros to die, of what they called terminal dehydration. I feared she would suffer. They assured me that she was not cognitive enough to suffer. They told me of medical studies showing that terminal dehydration under such circumstances is not painful and that any possible discomfort can be effectively treated by moistening the patient’s mouth and skin and by administering morphine if necessary. I was skeptical. I asked, “Why don’t you give her morphine anyway, just in case?” This plainly made them nervous. One of them said, “That could hasten her death, and we can’t do anything that seems like euthanasia.”
I resolved to watch Ros closely to make sure, as best I could, that she wasn’t suffering as she slowly died. I made the doctors promise that they would give her morphine if there were any sign of suffering. But it never seemed necessary.
She died on the tenth day. It was a quiet death, I would even say peaceful.
But it was still difficult to watch. This was, after all, someone I loved, and she was slowly, silently dying. Her urine output, through a catheter, slowed to a trickle and turned dark. Her breathing became shallow. She lay motionless and expressionless while the nurses gently moistened her lips and turned her from time to time in order to prevent bedsores.
One day near the end, I helped a nurse change Ros’s bedding, which required us to move Ros around on the bed a few times. I was grateful to be able to have a part, however small, in her care as she gradually slipped away.
On the fifth day, Ros’s long-lost brother Alex intervened.
Until Ros had her stroke, I had never even known that she had another brother. She had never mentioned him to me. Ted told me about Alex when I telephoned to inform him of the stroke. Ted said that Ros detested Alex. She and Alex had not seen each other in forty years. Alex was an ultraorthodox Jew; Ros was defiantly nonobservant. Alex was a political conservative; Ros was a passionate leftist. Alex had tried to tell Ros how to live her life; Ros had resented it. Alex was just like their father, and Ros had clashed bitterly with her father.
I guess that’s why she had never mentioned Alex.
A few days after the stroke, Alex telephoned me and introduced himself. It was a strange conversation. All he seemed to care about was whether she would be cremated, which he adamantly opposed. His rabbi had instructed him to make sure she wasn’t cremated. As it happened, however, her will called for cremation, and she had told me several times that she wanted her ashes scattered. But I figured it was premature to discuss the point, so I said nothing. I gave Alex the telephone numbers for Ros’s doctor and nurses.
When the ethics committee meeting was scheduled, I telephoned Alex and invited him to attend. He declined, saying he would defer to my decision on whether to withhold the feeding tube. He didn’t seem to care much about it. After the meeting, when I called him and told him what had happened, it still seemed that his only concern was that she not be cremated. This time, however, I told him of her instructions. He became distraught.
Five days later, as Ros lay dying, Alex telephoned one of the nurses and demanded reinsertion of the feeding tube. Her attending physician called me; I called Alex. He told me something had changed. “My rabbi says that as long as the heart beats and she is not dying, she must be fed. Life is sacred.” I said, “Do you just automatically do whatever your rabbi tells you?” He seemed surprised by the question. “Of course!”
The conversation turned ugly. I said he had no business insisting on how Ros should die, just like he had never had any business telling her how to live. I said, “She told me what she wants, and I’m her voice now.” Alex replied with a warning: “If you don’t put that tube back in, I’m going to have a hundred Jews picketing that hospital tomorrow.” This was something I never anticipated. Why, I wondered, would a bunch of devout Jews object to letting Ros die?
Years later, I would find out why.
But Alex’s threat never materialized. I just told him to “do whatever you feel you need to do,” and I heard nothing more from him. The doctors were unsettled by his intervention but decided to ignore it. Five days later, Ros was dead. We had her ashes scattered over San Francisco Bay.
So I know what Michael Schiavo has gone through. He did what I had to do, but in far more painful circumstances, under intense public scrutiny, suffering accusations of murder and abuse and enduring the meddling of religious activists and politicians who knew nothing of his and his wife’s wishes and values.
And now I understand Alex better—where he came from, and who was behind him—for Alex’s rabbi morphed into a far more potent force in the Terri Schiavo case. Alex was my first battle in the religious Right’s cultural war on America. By the time the Schiavo case exploded onto the national scene, I understood whence it came and I knew where it would go.
2
A Family Tragedy
What a cruel irony that Terri Schiavo was named after St. Theresa of Avila, a sixteenth-century Carmelite nun who, at the age of twenty-four, took ill and fell into a coma but then revived, living a productive and spiritual life for another forty-three years.
Born Theresa Marie Schindler near Philadelphia, Pennsylvania, on December 3, 1963, the first of Bob and Mary Schindler’s three children, Terri as a child was shy and overweight. The family was suburban, middle-class, Catholic, and by all accounts quite ordinary. Bob was a businessman, Mary a homemaker. Terri wrote fan letters to television st...
Table of contents
- Cover
- Title Page
- Introduction
- Part One
- Part Two
- Part Theree
- Appendix
- Acknowledgments
- Chapter Sources
- About the Author
- Copyright
- About the Publisher
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn how to download books offline
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 990+ topics, we’ve got you covered! Learn about our mission
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more about Read Aloud
Yes! You can use the Perlego app on both iOS and Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Yes, you can access Using Terri by Jon Eisenberg in PDF and/or ePUB format, as well as other popular books in Theology & Religion & Social History. We have over one million books available in our catalogue for you to explore.