- 148 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
About this book
Acute kidney injury (AKI) is a serious disorder in which sudden impairment of kidney function occurs secondary to one or more of a variety of underlying conditions and exposures. It is very common in (elderly) ICU patients and associated with very high mortality. Many of those who survive suffer from permanent kidney failure and other long-term morbidities. Renowned experts from around the world have contributed to this new publication, creating a succinct yet complete review of the most controversial aspects of AKI. The topics range from epidemiology and basic science to pathophysiology and clinical issues. It is intended as a concise reference work for physicians and nurses who deal with AKI in clinical nephrology and intensive care wards on a daily basis.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Acute Kidney Injury - From Diagnosis to Care by X. Ding,C. Ronco,X., Ding,C., Ronco, Claudio Ronco,Claudio, Ronco in PDF and/or ePUB format, as well as other popular books in Medicine & Nephrology. We have over one million books available in our catalogue for you to explore.
Information
AKI Management
Ding X, Ronco C (eds): Acute Kidney Injury - From Diagnosis to Care.
Contrib Nephrol. Basel, Karger, 2016, vol 187, pp 84-93 (DOI: 10.1159/000442368)
Contrib Nephrol. Basel, Karger, 2016, vol 187, pp 84-93 (DOI: 10.1159/000442368)
______________________
Fluid Management in Acute Kidney Injury
Chiao-Lin Chuang
Division of General Medicine, Department of Medicine, Taipei Veterans General Hospital, and Department of Medicine, National Yang-Ming University School of Medicine, Taipei, Taiwan
______________________
Abstract
The goal of fluid therapy in critical care medicine is to restore hemodynamic stability and vital organ perfusion while avoiding interstitial edema. Acute kidney injury (AKI) is a common complication in critically ill patients. Decisions regarding fluid management in critically ill patients with AKI are difficult, as these patients often have accompanying oliguria as well as body fluid overload. Both hypovolemia and volume overload are associated with increased morbidity and mortality in critical care patients; therefore, accurate assessment of the intravascular volume status as well as the response to fluid replacement remains one of the most challenging and important issues for clinicians in daily practice. Newer dynamic preload indexes, such as stroke volume variation and pulse pressure variation in conjunction with the end-expiratory occlusion test and the passive leg-raising test, have been shown to be more reliable indicators for accurate evaluation of fluid responsiveness in critically ill patients than static pressure measurements, such as central vein pressure and pulmonary artery occlusion pressure. In patients with established AKI who are unresponsive to fluid administration, fluid restriction is the treatment of choice. When fluid therapy is indicated for AKI patients, isotonic crystalloids should be the preferred agents in the absence of hemorrhagic shock. Balanced solutions may reduce the risk of hyperchloremic acidosis and kidney injury. In summary, volume management is an integral part of the care of critically ill patients with AKI. An optimal strategy might involve a timely period of guided fluid resuscitation with appropriate solutions, followed by an appropriate fluid balance.
© 2016 S. Karger AG, Basel
Acute kidney injury (AKI) is a frequent, life-threatening complication in critically ill patients. The Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) study investigators revealed the fact that septic shock is the most common factor contributing to AKI in intensive care units (ICUs), accounting for 47.5% of AKI patients [1]. Due to a lack of effective pharmacotherapies, treatment aimed at reversing or preventing septic AKI remains primarily based on supportive hemodynamic management. As a result, intravenous fluids play a critical role in the resuscitation of critically ill patients with severe sepsis or septic shock [2, 3]. From a renal perspective, the expected physiologic benefit of fluid resuscitation is based on the improvement of renal blood flow (RBF) and renal perfusion pressure resulting from restoration of effective circulating volume. However, AKI appears to be irreversible after achieving a supra-normal cardiac index, despite the fact that renal hypoperfusion is believed to contribute to the development of sepsis-induced renal dysfunction [4]. Significant changes in stroke volume (SV) and mean arterial pressure (MAP) induced by fluid challenge did not improve renal perfusion in patients with AKI [5]. Furthermore, septic patients with AKI often present with accompanying oliguria as well as body fluid overload, which is associated with increased capillary permeability as well as interstitial and cellular edema. Since the kidney is an encapsulated organ, fluid accumulation related to tissue edema would lead to a decrease in RBF and the glomerular filtration rate. Fluid overload in critically ill patients may also predispose them to the development of intra-abdominal hypertension, which is an additional risk factor for AKI [6]. In this regard, fluid overload is both a consequence of and a causative factor for AKI in critically ill patients. Overzealous fluid resuscitation and the resultant positive fluid balance in AKI are associated with increased lengths of ICU and hospital stays, a higher risk of renal nonrecovery and mortality [7-9]. A subgroup analysis of patients who developed AKI in the Fluid and Catheter Treatment Trial (FACTT) showed that a positive fluid balance after AKI carried a ‘dose effect’ association with the risk of death, with approximately 1.6-fold higher risk per liter/day of fluid accumulated [10]. Therefore, an optimal strategy and optimal target endpoints for fluid therapy during the resuscitation of critically ill patients with AKI are extremely imperative. A number of randomized control studies that provide evolutionary knowledge regarding the timing, the dose, and the type of fluid management used for the treatment of critically ill patients have been published during the past decades.
Type of Fluid Therapy
Crystalloids or Colloids
The physiologic rationale for administering colloids during resuscitation is to expand the plasma volume more effectively. The large-molecular-weight solutes present in colloid solutions are theoretically resistant to passing through capillary membranes and hence preserve intravascular oncotic pressure and prevent fluid extravasation. However, the advantages of colloids have been questioned for years. The Saline versus Albumin Fluid Evaluation (SAFE) study, a landmark study comparing the effects of 4% albumin versus normal saline in 6,997 critically ill patients, found no difference in all-cause mortality at 28 days [11]. In addition, subgroup analysis revealed an association of albumin with higher mortality in patients with traumatic brain injury [12]. Similarly, the Albumin Italian Outcome Sepsis (ALBIOS) trial, which compared 20% albumin to crystalloid in septic patient resuscitation, showed no survival benefit [13]. These results may be accounted for by the fact that the vascular endothelium is disrupted in critically ill patients. In the setting of increased capillary permeability with extravasation of proteins into the extracellular space, colloids may worsen edema by increasing interstitial oncotic pressure and fluid accumulation, resulting in further impediment of tissue perfusion.
Recently, the clinical association of synthetic colloid use with renal dysfunction has been confirmed by several clinical trials. The Scandinavian Starch for Severe Sepsis/Septic Shock Trial (6S) [14] and the Crystalloid versus Hydroxyethyl Starch Trial (CHEST) [15] reported a significantly higher risk of AKI or requirement of renal replacement therapy in patients receiving fluid resuscitation with hydroxyethyl starch compared with crystalloid solutions. Several hypotheses have been formulated to explain AKI following colloid administration, including the accumulation of low-molecular-weight fractions in renal tubules and osmotic nephrosis [16]. Given the evidence of the lack of significant clinical benefit from and the potential harmful effects of colloids, the current consensus statement of the Kidney Disease: Improving Global Outcomes clinical practice guidelines suggests that isotonic crystalloids, rather than colloids (albumin or hydroxyethyl starch), be used as initial management for the expansion of intravascular volume in patients at risk for AKI or with AKI in the absence of hemorrhagic shock [17].
Are All Crystalloids the Same?
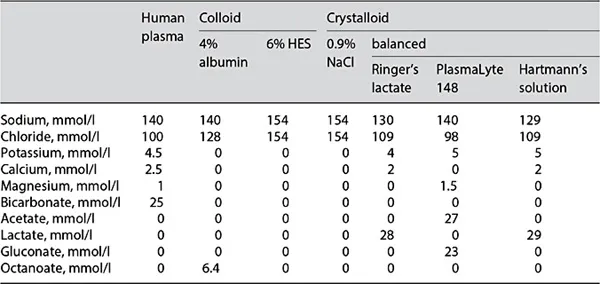
The most commonly used crystalloid in clinical practice is 0.9% saline with supra-physiologic levels of sodium and chloride. Resuscitation with moderate-to-large amounts of 0.9% saline induces hyperchloremia and metabolic acidosis [18], which has been associated with a decline in RBF in an animal study [19] and in healthy human volunteers [20]. Based on a study on 22,851 surgical patients with normal preoperative serum chloride concentrations and renal function, patients with postoperative hyperchloremia were more likely to develop postoperative renal dysfunction [21]. In this regard, current studies have largely focused on comparing the effects of different crystalloids. The ideal electrolyte solution may be one that reasonably parallels the plasma (table 1). Balanced fluids, such as lactate Ringer's, Hartmann's solution, and PlasmaLyte, have an electrolyte composition close to that of human plasma. The use of these chloride-restrictive fluids for volume resuscitation has been associated with significantly lower in-hospital mortality [22], a decreased incidence of AKI and the need for renal replacement therapy in ICUs [23]. More large-scale randomized control trials will be required to support the renal protectiveness of balanced solutions in the treatment of critically ill patients at risk for AKI or with AKI.
Table 1. Compositions of human plasma and commonly used solutions
Timing of Fluid Management
Rationale for Fluid Replacement in Acute Kidney Injury
According to this conceptual framework, AKI in critical illness is believed to be the consequence of reduced cardiac output (CO) and systemic hypotension, leading to a decrease in renal perfusion and the glomerular filtration rate. Thus, the resuscitation of patients in shock needs to be timely and adequate to prevent or attenuate AKI. For years, early goal-directed therapy (EGDT), aiming to optimize tissue oxygen transport by continuous monitoring of MAP, central venou...
Table of contents
- Cover Page
- Front Matter
- AKI Characteristics and Epidemiology
- AKI Pathophysiology and Diagnosis
- AKI Management
- Author Index
- Subject Index