![]()
McCullough PA, Kellum JA, Mehta RL, Murray PT, Ronco C (eds): ADQI Consensus on AKI Biomarkers and Cardiorenal Syndromes. Contrib Nephrol. Basel, Karger, 2013, vol 182, pp 99-116
DOI: 10.1159/000349969
______________________
Pathogenesis of Cardiorenal Syndrome Type 1 in Acute Decompensated Heart Failure: Workgroup Statements from the Eleventh Consensus Conference of the Acute Dialysis Quality Initiative (ADQI)
Michael Haasea · Christian Müllerb · Kevin Dammanc · Patrick T. Murrayd · John A. Kellume · Claudio Roncof · Peter A. McCulloughg · for the Acute Dialysis Quality Initiative (ADQI) Consensus Group
aDepartment of Nephrology and Hypertension, Diabetes and Endocrinology, Otto von Guericke University Magdeburg, Magdeburg, Germany; bDepartment of Cardiology, University Hospital, Basel, Switzerland; cDepartment of Cardiology, University Medical Center Groningen, University of Groningen, Groningen, The Netherlands; dNephrology and Clinical Pharmacology, University College Dublin School of Medicine and Medical Science, Dublin, Ireland; eClinical Research, Investigation, and Systems Modeling of Acute Illness Center, Department of Critical Care Medicine, University of Pittsburgh, Pittsburgh, Pa., USA; fDepartment of Nephrology, International Renal Research Institute (IRRIV), San Bortolo Hospital, Vicenza, Italy; gSt. John Providence Health System, Warren, Mich., Providence Hospitals and Medical Centers, Southfield and Novi, Mich., St. John Macomb Oakland Center, Madison Heights, Mich., St. John Hospital and Medical Center, Detroit, Mich., USA
______________________
Abstract
Pathophysiological mechanisms of cardiorenal syndromes (CRS) types 1-5 are still sparsely characterized. In an attempt to address this issue, a consensus conference on CRS was held in Venice, Italy, in November 2012 under the auspices of the Acute Dialysis Quality Initiative (ADQI). Working group 1 discussed monodirectional mechanisms of CRS type 1 which is characterized by a rapid worsening of cardiac function leading to acute kidney injury (AKI). Pre-conference we performed a systematic search and review of the available literature using a modified Delphi analysis. Hereby identified and in this review discussed questions were: (i) What are the predominant pathophysiologic mechanisms of CRS type 1 in acute decompensated heart failure? (ii) Could biomarker profiling identify pathomechanisms or hemodynamic phenotype of patients with CRS type 1? Could predictive biomarkers improve renal safety of therapy in CRS type 1? (iii) How do the timing, severity and duration relate to the mechanisms and outcomes of CRS type 1 ? In summary, after discussion and appraisal of the best available evidence, working group 1 makes consensus recommendations for future research on pathologic mechanisms of CRS type 1 and recommendations for clinical practice where treatment is in either proof or disproof of a mechanism.
Copyright © 2013 S. Karger AG, Basel
ADQI 11 Workgroup members are listed in Appendix 2.
Bidirectional acute and chronic disorders of heart and kidney are today classified as cardiorenal syndromes (CRS) types 1-5, however pathophysiological mechanisms are sparsely characterized with regard to correct identification and treatment at clinical presentation. In an attempt to address this issue, a consensus conference on CRS was held in Venice, Italy, in November 2012 under the auspices of the Acute Dialysis Quality Initiative (ADQI).
Working group 1 addressed these issues for CRS type 1 which is characterized by a rapid worsening of cardiac function leading to acute kidney injury (AKI) [1, 2]. CRS type 1 most frequently appears in the setting of acute decompensated heart failure (ADHF) [3] and follows ischemic (cardiac surgery, myocardial infarction) or non-ischemic (valve dysfunction, aortic dissection, pulmonary embolism, etc.) cardiac events. Up to 40% of patients hospitalized for ADHF develop AKI [4]. These patients require a more complex management and experience more complicated hospital courses and higher mortality. Preliminary data point towards the importance of timing in the development of AKI with regard to severity of the renal stressor versus iatrogenic effects.
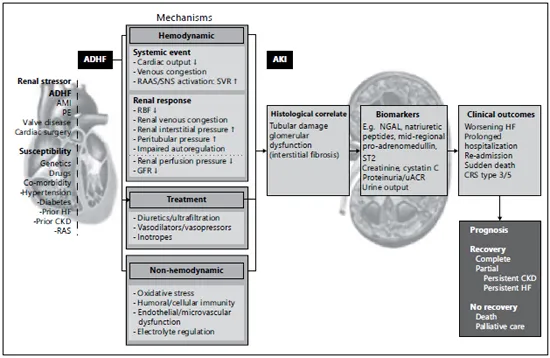
Classical mechanisms of CRS type 1 include low cardiac output (CO) and neurohormonal activation and release of vasoactive substances resulting in low renal perfusion and possible renal ischemia with AKI. In addition, high central venous pressure (CVP), increased intra-abdominal pressure leading to venous congestion, activation of the sympathetic nervous system and the renin-angiotensin-aldosterone system (RAAS) and release of other vasoactive substances such as endothelin, anemia and a marked alteration of immune and somatic cell signaling have all been implicated as important contributors of kidney injury (fig. 1).
As far as understanding CRS type 1 pathophysiology is concerned, treatment approaches including agents targeting vasoactive and neurohormonal pathways and strategies to correct renal congestion through negative fluid balance are briefly discussed.
Methods
Pre-conference we performed a systematic search and review of the available literature, as described in the ADQI 11 conference summary statements elsewhere in this issue. Specifically, we focused on the identification of pathomechanisms of the acutely dysfunctioning heart damaging the kidney and their potential to be correctly identified in daily practice. Treatment effects in CRS type 1 were only considered either as proof or disproof of a mechanism. Experiments and studies were identified via Medline and Web of Science using the terms ‘cardiorenal’, ‘(acutely/acute decompensated) heart failure’, and ‘acute kidney injury (AKI)’ or ‘(worsening) renal (function)’ combined with ‘animal (experiment/model)’, ‘(paťho)mechanism’, or ‘paťhophysiology’, ‘pathway’ or ‘RAAS’, ‘fluid retention’, ‘sympathetic nervous system’, ‘biomarker’ or ‘immunity’. In view of the volume of the retrieved literature, only representative publications are cited in this review. Furthermore, we opted to limit this summary to clinical scenarios in which there was ample data. We did not include the specific clinical situations of cardiac surgery procedures with the use of cardiopulmonary bypass or contrast media application as we rank both scenarios as antecedents to CRS type 1.
Fig. 1. Overview on mechanisms, histological correlates biomarkers and outcomes in CRS type 1 in the setting of acute decompensated heart failure. Reproduced with permission from ADQI [53]. ADHF = Acute decompensated heart failure; AKI= acute kidney injury (the term AKI also covers the term ‘WRF’, ‘worsening renal function which is usually defined as doubling in serum creatinine); AMI = acute myocardial infarction; PE = pulmonary embolism; SVR= systemic vascular resistance; HF = heart failure; CKD = chronic kidney disease; RAS = renal artery stenosis; GFR = glomerular filtration rate; NGAL = neutrophil gelatinase-associated lipocalin; IL-18 = interleukin-18; KIM-1 = kidney injury molecule 1; L-FABP = liver-type fatty acid binding protein; NAG = N-acetylglucosamine.
This report is the result of a modified Delphi analysis [5] which is a structured and standardized process for collecting, summarizing and disseminating knowledge from a group of experts focused on a specific problem or task. A detailed description of the ADQI methodology is available at www.adqi.net.
Based on the literature identified prior to the conference, the following key questions were identified:
Question 1: What are the predominant pathophysiologic mechanisms of CRS type 1 in ADHF?
Question 2: Could biomarker profiling identify pathomechanisms or hemodynamic phenotype of patients with CRS type 1? Could predictive biomarkers improve renal safety of therapy in CRS type 1?
Question 3: How do the timing, severity and duration relate to the mechanisms and outcomes of CRS type 1?
At the conference, after a systematic literature review and the appraisal of the best available evidence, group 1 discussed monodirectional mechanisms of CRS type 1 generating from the heart affecting the kidney.
Results
Ad Question 1: What are the predominant pathophysiologic mechanisms of CRS type 1 in ADHF?
Hemodynamic Mechanisms
Observations from experiments and the clinical setting suggest that hemodynamic mechanisms seem to play a major if not predominant role in CRS type 1 in the setting of ADHF. Various animal studies suggest an initial hemodynamic event as a CRS type 1 trigger leading to decreased renal arterial flow, renal oxygen consumption and glomerular filtration rate (GFR) and increased renal vascular resistance whereas hemodynamic counteractive measures such as renal-selective blood perfusion restored all of these hemodynamic parameters and renal function back to normal [6].
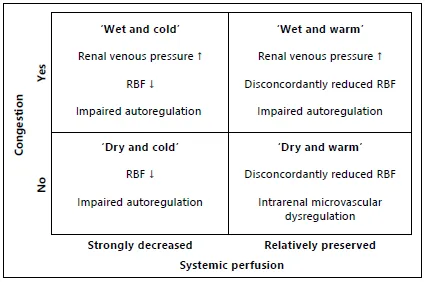
In the general setting of ADHF, different hemodynamic profiles have been proposed based on the clinical phenotype of individual patients [7]. This approach consists of categorization of patients dependent of their systemic hemodynamics, including adequacy of perfusion (decreased CO and decreased effective circulation fluid volume (ECFV)) and extent of (pulmonary) congestion (increase in CVP or wedge pressure). As such, these can be combined into four distinct profiles deemed wet or dry and warm or cold (fig. 2).
It is within each of these profiles of ADHF where CRS type 1 may develop. Since hemodynamics, patient characteristics, treatment, and even outcome are different in each of the four profiles, it is likely that also the pathophysiology of CRS type 1 may differ dependent of the hemodynamic profile of ADHF [8]. In addition, the occurrence of AKI in this setting may not only be restricted to within a certain profile, but may also be related to the dynamic process of shifting between profiles during either treatment or deterioration of ADHF.
Fig. 2. Systemic hemodynamic profiles of ADHF and renal hemodynamic consequences in CRS type 1. Adapted from Stevenson and Perloff [7]. This figure combines profiles of ADHF with systemic hemodynamics and possible hemodynamic renal mechanisms that can cause CRS type 1 in each of the profiles. In the ‘cold’ profiles, AKI may develop as a consequence of reduced RBF when autoregulation is unable to preserve GFR. In the ‘dry and cold’ profile, this may include anemia or stringent diuresis/ultrafiltration with associated blood pressure reductions. In the ‘wet’ profiles, increased central venous pressure leads to increased renal venous pressure, that reduces renal perfusion pressure, increases renal interstitial pressure, opposing filtration by collapse of tubules. In the ‘warm’ profiles, although systemic perfusion is relatively preserved, RBF is disconcordantly reduce...