eBook - ePub
The Psychosomatic Assessment
Strategies to Improve Clinical Practice
- 254 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
The Psychosomatic Assessment
Strategies to Improve Clinical Practice
About this book
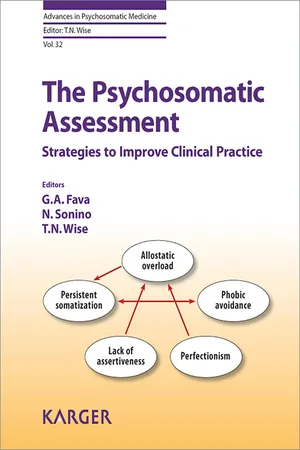
Patient reported outcomes have become more and more important in clinical practice and research. Evaluating subjective perceptions of patients has become mandatory for a full assessment of treatment responses. In this context, clinimetrics, the science of clinical measurements, provides unprecedented opportunities for psychosomatic assessment. This volume illustrates how this approach can be translated into everyday practice complementing and improving the medical interview. The most sensitive and reliable clinical methods are presented for evaluating specific psychosocial aspects of disease, i.e. childhood adversities, life events and chronic stress, lifestyle, sexual function, subclinical and affective disturbances, personality, illness behavior, well-being and family dynamics. Each chapter provides practical illustrations as to how crucial information can be obtained with specific methods individualized according to the patients' needs. A hyperlink is provided to a website that contains many of the instruments assessed in the volume. This book enables the reader to understand the value of patient reported outcomes in clinical practice. It is intended to expand and refine the skills of clinicians who work in general and specialized medicine and psychiatry, whether physicians, psychologists or other health professionals.
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
Fava GA, Sonino N, Wise TN (eds): The Psychosomatic Assessment. Strategies to Improve Clinical Practice.
Adv Psychosom Med. Basel, Karger, 2012, vol 32, pp 133–159
Adv Psychosom Med. Basel, Karger, 2012, vol 32, pp 133–159
______________________
Assessment of Personality in Psychosomatic Medicine: Current Concepts
Fiammetta Cosci
Department of Psychology, University of Florence, Florence, Italy
______________________
Abstract
The notion that personality variables can affect vulnerability to specific diseases has been widely promoted in psychosomatic medicine. Over the time, some personality patterns have been extensively studied. Among them, alexithymia, type A, and type D personality are the most relevant. However, also temperament and character has increasingly been object of studies. Alexithymia is currently recognized as a risk factor for medical, psychiatric, or behavioral problems; type A personality is recognized to increase the risk for coronary artery disease, and type D personality has been related to adverse cardiac events and cardiovascular outcomes. The growing interest and clinical role of the personality constructs in psychosomatic medicine has been favored by the revolutionary understanding that personality factors are not causes of medical disease but their moderators/ mediators, and by the decline of the psychometric distinction between state and trait. Indeed, it is nowadays recognized that psychological constructs traditionally conceived as trait dimensions may surprisingly display sensitivity to change in specific clinical situations. Assessing personality, thus, has become worth pursuing since it may give unique information about individuals with medical conditions and contribute to completely understand medical patients and their global health as well as formulating optimal decision-making and treatment planning. In this framework, the present chapter has the aim to provide insight into personality dimensions in psychosomatic medicine and describe the main instruments to assess it.
Copyright © 2012 S. Karger AG, Basel
The notion that personality variables can affect vulnerability to specific diseases was prevalent in the first phase of the development of psychosomatic medicine (1930-1960). Thereafter, this notion declined together with the prospects for psychosomatic medicine itself. In the last decades, changes in medicine provided a basis for an alternate approach to psychosomatic medicine [1]. Contributing to this process was the recognition of limitations of the narrow biomedical model and the emerging role of the biopsychosocial model of illness [2]. In this new psychosomatic perspective, personality received a relevant role.
Over the time, some personality patterns have been thought to be strictly linked to somatic illness and have been extensively studied. Moreover, new personality constellations have been developed attracting the attention of many researchers worldwide. One of the seminal personality constructs in psychosomatic medicine is undoubtedly alexithymia; one of the most influential constructs has certainly been type A personality, and one of the most promising constructs for the next years is type D personality.
The popularity of alexithymia in psychosomatic medicine has been highlighted by many authors. It has been conceived as a deficiency in the cognitive processing of emotions, which is not specific to psychosomatic disorders but it is currently recognized as a risk factor for medical, psychiatric, or behavioral problems that are influenced by difficulties modulating arousal, appropriately expressing or suppressing emotions, employing fantasy, and obtaining and using social support [3].
Type A personality has become a classic construct in psychosomatic medicine and indicates a 'specific emotion-action complex' of individuals aggressively committed to struggle to achieve more and more in less and less time [4]. Many data have accumulated, particularly in cardiology, according to which subjects with a type A personality might have an increased risk for coronary artery disease if compared to subjects without such personality characteristics.
Type D personality, a general propensity to distress that is defined by high scores on the 'negative affectivity' (NA) and 'social inhibition’ traits, is increasingly studied, and a growing literature shows that it is related to adverse cardiac events and, being characterized also by a general propensity to psychological distress, to cardiovascular outcomes.
In general, the above-mentioned personality constructs, together with additional emerging ones, have earned a growing interest and an increasing clinical role in psychosomatic medicine. Their assessment has become worth pursuing because it can give unique information about individuals with medical conditions that traditional medical methods cannot reveal [5].
In this framework, the present chapter has the aim to provide insight into the assessment of personality dimensions in psychosomatic medicine as a contribution to the understanding of medical patients and their global health. The main instruments to assess personality in psychosomatic settings will be described to encourage their use in daily clinical practice.
Alexithymia
The term alexithymia literally means ‘lacking words for feelings' and was coined to describe certain clinical characteristics observed among patients with psychosomatic disorders who had difficulty engaging in insight-oriented psychotherapy [6]. Alexithymic patients demonstrate deficiencies in emotional awareness and communication and show little insight into their feelings, symptoms, and motivation. When asked about their feelings in emotional situations, they may experience confusion (e.g. 'I don't know'), give vague or simple answers (e.g. 'I feel bad'), report bodily states (e.g. 'my stomach hurts'), or talk about behavior (e.g. 'I want to punch the wall').
The alexithymia construct was originally conceptualized by Nemiah et al. [7] as encompassing a cluster of cognitive traits including difficulty identifying feelings and describing feelings to others, externally oriented thinking, and a limited imaginal capacity. This original view of alexithymia has been the most influential in contemporary theory and research [3]. An alternative conceptualization, that alexithymia is a global impairment in emotional processing resulting in limited emotional expression and recognition, has been less influential thus far [8]. Yet, both definitions agree that alexithymia is a deficit, inability, or deficiency in emotional processing rather than a defensive process, and this deficit view is gaining increasing support from basic laboratory and neuroimaging research [9, 10]. For more details on alexithymia conceptualizations, see Taylor [11].
Alexithymia was first described in people with psychosomatic disorders, and subsequent research has confirmed elevated levels of alexithymia in people with rheumatoid arthritis, essential hypertension, peptic ulcer, and inflammatory bowel disease [3]. Yet, studies have found elevated alexithymia in patients with a range of other conditions (e.g. cardiac disease, noncardiac chest pain, breast cancer, diabetes, chronic pain, eating disorders, substance dependence, kidney failure, stroke, HIV infection, fibromyalgia). The growing recognition that alexithymia is not specific to psychosomatic disorders has led to the view of alexithymia as a risk factor for those medical, psychiatric, or behavioral problems that are influenced by disordered affect regulation [3, 12]. Indeed, alexithymia has been associated with a failure to use adaptive affect regulation processes such as modulating arousal, appropriately expressing or suppressing emotions, employing fantasy, obtaining and using social support, tolerating painful emotions, cognitive assimilation, and accommodation. Evidence shows that the alexithymic deficit in processing feelings is likely to affect mental and somatic health through behavioral actions as ways to regulate affective states (e.g. alcohol abuse, eating behaviors), psychopathology directly related to emotional dysregulation (e.g. somatoform disorder, panic disorder), posttraumatic shutdown of emotions (e.g. posttraumatic stress disorder, acute reactions to severe organic diseases), altered autonomic, endocrine, and immune activity (e.g. vulnerability to inflammatory processes), somatosensory amplification, health care-seeking behavior, and negative treatment outcomes [13, 14]. More recently, treatment studies on alexithymia showed, for instance, that it is not appropriate to assume that alexithymic patients have reservations about entering into a psychotherapeutic treatment [15] and that cancer patients may benefit from a multicomponent psychological intervention in terms of cancer pain and alexithymia [16]. Similarly, prognostic studies showed that lower levels of childhood sexual abuse decreased the risk of being highly alexithymic, thus reducing the likelihood and severity of depression [17], that the presence of alexithymia at the time of the percutaneous transluminal coronary angioplasty in coronary heart disease (CHD) patients is a unique significant psychological predictor of poorer physical functioning at 6 months [18], and that alexithymia is a strong risk factor for all-cause 5-year mortality in hemodialysis patients [19].
Several methods have been developed to measure alexithymia, including structured interviews, self-report scales, by proxy information, and the Rorschach. Currently, the most commonly used method is the 20-item version of the ...
Table of contents
- Cover Page
- Front Material
- Principles of Psychosomatic Assessment
- The Psychosomatic Interview
- Evaluating Childhood Adversity
- Evaluating Life Events and Chronic Stressors in Relation to Health: Stressors and Health in Clinical Work
- Assessment of Lifestyle in Relation to Health
- Assessment of Sexual Function in the Medically III: Psychosomatic Approach to Sexual Functioning
- Psychological Factors in Medical Disorders Assessed with the Diagnostic Criteria for Psychosomatic Research
- Mood and Anxiety in the Medically III
- Assessment of Personality in Psychosomatic Medicine: Current Concepts
- Illness Behavior
- Assessment of Psychological Well-Being in Psychosomatic Medicine
- Family Assessment in the Medical Setting
- Relational Ethics and Psychosomatic Assessment
- Author Index
- Subject Index
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn how to download books offline
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 990+ topics, we’ve got you covered! Learn about our mission
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more about Read Aloud
Yes! You can use the Perlego app on both iOS and Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Yes, you can access The Psychosomatic Assessment by G. A. Fava,N. Sonino,T. N. Wise,G.A., Fava,N., Sonino,T.N., Wise, T. N. Wise,T.N., Wise in PDF and/or ePUB format, as well as other popular books in Medicine & Cardiology. We have over one million books available in our catalogue for you to explore.