![]()
Güell JL (ed): Cornea. ESASO Course Series. Basel, Karger, 2015, vol 6, pp 1-25
DOI: 10.1159/000381489
______________________
The Ocular Surface: Functional Anatomy, Medical and Surgical Management
Harminder S. Duaa, b · Dalia G. Saidb
aAcademic Ophthalmology Section, Division of Clinical Neuroscience, University of Nottingham and bQueens Medical Centre, University Hospital, Nottingham, UK
______________________
Abstract
The ocular surface (OS) is a functional unit comprising the eyelids and blink reflexes, tear film and tear glands, the conjunctival mucus membrane and substantia propria, and the corneal epithelium and Bowman's zone. Its health is crucial for vision. The OS can be affected by a variety of degenerative, inflammatory and neoplastic diseases, as well as by trauma. Significant amongst these are dry eye disease, microbial infections and immune-mediated inflammatory disorders ranging from allergic conjunctivitis to destructive conditions such as ocular cicatricial pemphigoid and chemical burns. Several of these can lead to persistent epithelial defects with risk of perforation. Management principles include a thorough history and clinical evaluation of signs and symptoms to establish the diagnosis and determine the extent of disease. Treatment is tailored to the specific condition and ranges from lubricant drops to antimicrobial agents and anti-inflammatory drugs such as steroids and steroid-sparing agents. A variety of surgical procedures are often required both as adjunctive or primary interventions. These can be simple outpatient procedures such as punctal plugs and tarsorrhaphy or complex procedures such as amniotic membrane grafts, keratoplasty and limbal stem cell transplantation. In end-stage diseases where the OS is severely compromised and dry, keratoprosthesis remains the only hope to restore some sight.
© 2015 S. Karger AG, Basel
The Ocular Surface
The term ‘ocular surface’ (OS) was coined by Richard Thoft [1] to include the entire mucus membrane lining from the lid margins across the posterior surfaces of the eyelids, the superior, inferior, medial and lateral fornices, the eye ball, the limbus and the corneal surface together with the tear film. As an anatomical unit, the OS includes the entire conjunctival, the limbal and corneal epithelium. However, as a functional unit, the OS includes the eyelids and their movements together with the glands that secrete the various components of the tear film. As far as the depth of the OS is concerned, different authors have been fairly liberal in limiting it to the epithelium or extending it to the entire thickness of the conjunctiva and all layers of the cornea.
Functional Anatomy
The key player at the OS is the transparent cornea, which interfaces with light rays as they traverse to the retina. The other elements of the OS serve to maintain a healthy environment in which the cornea can retain its transparency and facilitate vision. Despite its very organized structure, the epithelium of the cornea is a poor optical surface without the ‘polish’ provided by the tear film.
Tear Film and Conjunctiva
This is a dynamic complex structure that is served by numerous cells and glands and that is continuously replenished and evenly distributed across the OS by the blinking action of the eyelids. The tears are primarily made of mucin derived from the epithelial cells and goblet cells of the conjunctiva, an aqueous component derived from the lacrimal and accessory lacrimal glands and an oil component derived from the meibomian glands of the eyelids. The hydrophobic surface of the corneal epithelium is rendered hydrophilic by the binding of mucin to the epithelial cells. This allows the aqueous component to form a relatively thick layer on the mucin bed, upon which the meibomian oil (meibum) spreads as a thin layer, delaying both evaporation and the breakup of the tear film. Though the tear film is described as a trilaminar structure, it is now known that the three laminae are not distinct and defined; instead, a gradient of mucin admixes with the aqueous component from the epithelium to the oil layer. In addition, the tears contain a myriad of proteins, growth factors, vitamins, electrolytes and a few cells that collectively contribute to the nourishment, defence and health of the OS [2].
In the interest of transparency, the cornea has to forsake an established blood supply, which is restricted to the limbal arcades. The cornea therefore relies on nutrients provided via the aqueous humour, the tear film and the limbal vessels. Oxygen from the atmosphere dissolved in the tear film reaches the cornea; hence, contact lenses can potentially interfere with this process and cause adverse consequences. Equally noxious agents such as carbon monoxide from smoke can also dissolve in tears and reach the cornea. The exposed position of the eyes renders the cornea especially vulnerable to injury and to microbial invasion from the environment [3]. Immunoglobulins, lysozyme, lactoferrin and a number of antimicrobial peptides provide innate defence, which is backed up by cell-mediated and humoral responses by the resident and circulating lymphocytes of the conjunctival mucosal immune system. The conjunctival substantia propria is known to express many high endothelial venules during inflammation to facilitate exit of mononuclear cells, and even to demonstrate follicular aggregations with germinal centres. This enables the conjunctiva to respond to a number of different insults, which in turn, can compromise its health. Conjunctival health determines corneal health [4].
The importance of the tears cannot be overestimated. Dry eyes cause troublesome symptoms and blurring of vision and considerably affect the quality of life of the patient. Many interventions to restore sight involve the transplantation of tissues such as corneal, limbal and amniotic membrane (AM) tissue. No living tissue transplant can survive for long in a dry environment.
The Limbus
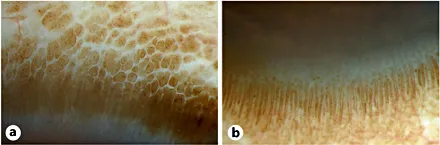
The microanatomy of the limbus reveals a defined stromal architecture with a unique blood supply, the palisades of Vogt, the interpalisade rete ridges, and the limbal epithelial crypts. Collectively, they provide the anatomical basis and the physiological microenvironment for the maintenance of corneal epithelial stem cells (SCs). The physiological turnover of the corneal epithelium throughout life requires new cells to take the place of those that are lost. This is facilitated by the limbus, which acts as a repository of SCs [5]. Though there is some evidence that the basal epithelium of the cornea (transient amplifying cells) can sustain the physiological demand, there is no doubt that in response to injury or insult, limbal SCs play an important role in regenerating the corneal surface [6]. Features of the normal and deficient/abnormal limbus have been defined clinically and by in vivo confocal microscopy. The palisade architecture is maintained in the stroma underlying the basal cells, and limbal epithelial crypts are often particularly detectable in pigmented palisades, where confocal visibility is better [7-10] (fig. 1a, b).
Fig. 1. Diffuse slit lamp image of limbal palisades of Vogt. Pigmented palisades are easy to visualise. The linear palisades (a and b) and the rounded accessory palisades seen at the conjunctival (a) and corneal (b) aspects of the linear palisades are clearly visible. The palisades and interpalisade rete ridges are repositories of stem cells.
Often, a large part of the central corneal epithelium can be lost whilst a rim of peripheral and limbal epithelium survives. This is due to the enhanced adhesion of peripheral/limbal basal cells to the underlying basement membrane, which allows these cells to survive and function to resurface the cornea. Such injuries to the corneal epithelium that retain an intact limbus heal via the formation of 2-6 centripetally migrating convex-fronted epithelial sheets that meet each other along adjacent surfaces, giving the defect a geometric shape (triangular, quadrilateral, pentagonal, or hexagonal), which eventually closes via the formation of Y-shaped contact lines that are visualized by fluorescein stain and represent the pseudodendrites associated with the healing of corneal abrasions (fig. 2a). In injuries in which the limbus is affected, healing occurs via the circumferential migration of tongue-shaped epithelial sheets that arise from each end of the surviving epithelium (usually in the upper half). These migrate along the denuded limbus until they meet. Thereafter, the defect behaves like one with an intact limbus following the same sequence as described above (fig. 2b). In some instances, the centripetally migrating conjunctival epithelium of the adjacent conjunctival defect can encroach on the denuded limbus and cornea, resulting in conjunctivalization of the cornea. This is considered as a hallmark of limbal SC deficiency (LSCD) [11-13] (fig. 2c).
Established concepts related to SC are now challenged by emerging clinical situations such as surviving central islands of epithelial cells in the presence of total LSCD [6] and by the transdifferentiation of the conjunctival epithelium into a corneal phenotype on the corneal surface. Mesenchymal SCs that have been shown in specific sites such as foetal liver, bone marrow and dental pulp have also been demonstrated in the corneal stroma. These cells have immense potential for clinical use for tissue regeneration.
Corneal Innervation
The principal nerve supply comes from the ophthalmic division of the trigeminal nerve via the long posterior ciliary nerves. These nerves arborize posterior to the limbus and form a perilimbal plexus from which nerves enter th...