![]()
Giustina A, Bilezikian JP (eds): Vitamin D in Clinical Medicine.
Front Horm Res. Basel, Karger, 2018, vol 50, pp 42–65 (DOI: 10.1159/000486065)
______________________
New Concepts in Vitamin D Requirements for Children and Adolescents: A Controversy Revisited
Emma M. Laing · Richard D. Lewis
Department of Foods and Nutrition, The University of Georgia, Athens, GA, USA
______________________
Abstract
North American and European authorities have identified thresholds up to 50 nmol/L serum 25-hydroxyvitamin D (25[OH]D) as optimal for pediatric vitamin D status. These recommendations are relative to skeletal endpoints, as vitamin D plays a pivotal role in bone mineral content (BMC) accretion. Suboptimal vitamin D consumption during youth may therefore hinder BMC acquisition, and contribute to an increased fracture risk. Though vitamin D requirements range between 400 and 800 IU/day, not all children achieve this. To encourage adequate vitamin D consumption, strategies such as supplementation, food labeling, and fortification, are currently being investigated. There is moderate support for the role of vitamin D supplementation on adolescent BMC accrual; however, factors such as age, maturation, population ancestry, and latitude, are not consistently accounted for across studies. Vitamin D is also linked with extraskeletal endpoints (e.g., muscle mass/function, adiposity, and metabolic health) in children, but the cross-sectional data do not necessarily align with results from experimental trials. Based on the evidence currently available, there is no need for a revision of the pediatric vitamin D recommendations at this time. Additional trials are required, however, to build upon the hypothesis-generating observational data, and to provide evidence for future vitamin D requirements across the globe.
© 2018 S. Karger AG, Basel
Introduction
In 2011, the Institute of Medicine (IOM) released the dietary reference intakes (DRI) for calcium and vitamin D for the United States and Canada [1]. Since the publication of these important guidelines, both the scientific community and the consumer have had a vested interest in understanding the health benefits of vitamin D and how these should be reflected in recommended targeted intakes for children. The IOM report is considered a landmark document that most national authorities have consulted when developing dietary recommendations for vitamin D [2]. Throughout the development of these recommendations, the IOM committee considered only data pertaining to skeletal outcomes, since the role of vitamin D in promoting extra-skeletal health are conflicting and based predominantly on observational studies. A recent report on vitamin D and calcium from the Agency for Healthcare Research and Quality, which reviewed data from studies published between 2009 and 2013 [3], also concluded that a relationship between vitamin D and functional health outcomes other than skeletal health cannot be made. Other advancements since the 2011 IOM report are reflected in key publications, including systematic reviews [4–7], randomized controlled vitamin D clinical trials (RCTs) generating both skeletal and extraskeletal outcomes [8–15], and various reviews and editorials on this topic [16–19], which collectively formed the basis for estimating the current European vitamin D intake recommendations [20–24].
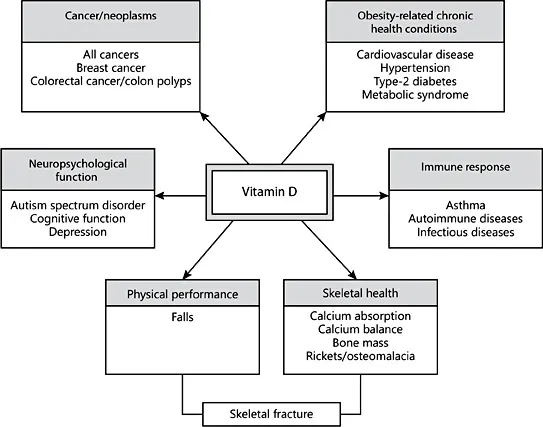
The US and Canadian DRIs and the European dietary reference values (DRVs) range from 400 to 800 IU/day and are based on targeted serum 25-hydroxyvitamin D (25[OH]D) concentrations of 25–50 nmol/L [1, 21–23]. While actual vitamin D intake varies widely based on country-specific fortification policies and supplementation practices, typical intakes are well below 400 IU/day [1, 25–27]. In contrast, recent NHANES data [28] show that the average 25(OH)D concentrations in US children aged 6–19 are between 66 and 72 nmol/L, and actually exceed IOM thresholds. Historically, low circulating 25(OH)D concentrations have been used in the clinical diagnosis of vitamin D deficiency rickets in children. More recently, low serum 25(OH)D has been linked to health conditions, such as diabetes, autoimmune diseases, cardiovascular disease, and cancer (Fig. 1) [29–33]. Despite lack of consistency in the evidence and appropriate RCTs, novel relationships between vitamin D and skeletal and extraskeletal health outcomes have prompted an upsurge in the number of laboratory 25(OH)D tests ordered by clinicians and in the use of vitamin D supplements by the public [34, 35].
There is much controversy, at least in adults, surrounding current vitamin D requirements in the realm of (1) the DRIs and dietary reference values for vitamin D, (2) the most recent estimations of deficiency and insufficiency in children, (3) the utility and appropriateness of laboratory 25(OH)D tests, and (4) the increased use of vitamin D supplements among the public. Some researchers challenge the interpretation of vitamin D requirements, arguing that they are overly conservative, or that both skeletal and extraskeletal outcomes should have been considered in reaching a consensus on optimal serum vitamin D values [2, 36]. Others challenge the requirements based on confounding factors that contribute significantly to the variation in serum 25(OH)D but are not consistent across the studies that were used to determine vitamin D requirements. These include age, sex, maturation, body composition, latitude, ultraviolet-B (UVB) exposure, season, degree of urbanization, population ancestry, family income, education, obesity, and genetic variation factors, among others [37–39].
Fig. 1. The link between low serum vitamin D and health conditions.
This chapter reviews estimations of vitamin D inputs needed to meet pediatric requirements. In addition, evidence from RCTs since the 2011 IOM report [1] will be evaluated with respect to the effects of vitamin D on skeletal and extraskeletal outcomes in children in light of serum 25(OH)D thresholds. The chapter also highlights knowledge gaps that will need to be addressed in order to ascertain the need for updated pediatric vitamin D requirements in the future.
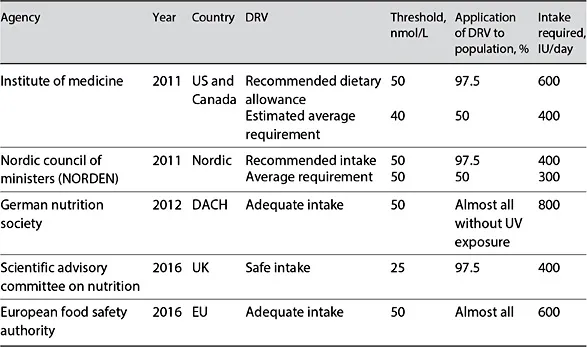
Estimation of Vitamin D Inputs to Meet Requirements
Table 1 shows North American and European national authority requirements for vitamin D as adapted by Ni Chaoimh et al. [40]. The IOM committee used a mixed-model approach to estimate the dose-relationship between total dietary intake of vitamin D to achieve the desired serum 25(OH)D levels [1]. The report stated that an increased risk of vitamin D deficiency should be defined using serum 25(OH)D concentrations <30 nmol/L, and that vitamin D supplementation should not be necessary with a vitamin D concentration >50 nmol/L [1]. Both the Pediatric Endocrine Society and the American Academy of Pediatrics use the 25(OH)D threshold of >50 nmol/L to define sufficiency in children [41, 42]. The US and Canadian estimated average requirement (EAR) for vitamin D reflects the most probable requirement for the population, and is used to estimate the probability that an individual’s 25(OH)D reflects an adequate intake, whereas the recommended dietary allowance (RDA) reflects the approximated requirement for those at the highest end of the distribution. That is, at least 97.5% of the population should have a requirement that is below the RDA, as this should be considered the upper end of the spectrum for human need, and should therefore most often meet the needs of generally healthy people. In contrast, the UK’s Scientific Advisory Committee on Nutrition proposed a serum concentration of 25 nmol/L as a “population protective,” defined as the minimum threshold that should be met by almost everyone.
Table 1. North American and European national authority requirements for vitamin D
Published as a “Perspective” in the New England Journal of Medicine [18], members of the DRI committee for vitamin D who contributed to the IOM report cautioned that using the RDA as a goal for vitamin D intake for a population inflates the prevalence of inadequacy. The authors stated, “A common misconception is that the RDA functions as a ‘cut point’ and that nearly the entire population must have a serum 25(OH)D level above 20 ng/mL (i.e., 50 nmol/L) to achieve good bone health. The reality is that the majority (about 97.5%) of the population has a requirement of 20 ng/mL or less” [18]. The National Academies of Medicine also published how the RDA for vitamin D was determined [43]. In this statement, it is explained that the EAR was determined as an “equivalent to an intake that produced a serum level of 40 nmol/L” and that “the goal is not, and should not be, to assure that 97.5% of the population exceeds the serum value linked to the RDA. Doing so would shift the distribution to a higher level that is associated with increased risk for adverse effects.” In essence, to bring serum 25(OH)D concentrations >50 nmol/L in nearly all children would require vitamin D intakes that far exceed the current EAR and the RDA [1]. A recent systematic review in adults shows that when groups are vitamin D deficient, there is significant value in providing an additional 400 IU/day of vitamin D above the RDA or requirement [6]. In children, vitamin D supplementation at levels above the RDA may likewise be ne...