![]()
1
HISTORY AND EXAMINATION
INTRODUCTION
In the assessment of a patient with eye disease, it is important to take a good history, examine the eyes with adequate illumination and test the visual function. Macular diseases and glaucoma have become more common as causes of severe visual loss. In these cases, a fundal examination with dilatation of the pupils in a darkened room is necessary in order to assess the macula and optic disc.
Altered vision or pain in the eye usually indicates eye disease and must be explained. A detailed history, thorough clinical examination, and in some cases, relevant imaging are required for accurate diagnosis and timely treatment.
HISTORY
Past ocular and systemic history can provide useful clues to diagnosis as can family history.
Note previous allergies and current medications.
OCULAR SYMPTOMS
These include blurred vision, distorted vision, double vision, floaters, flashes, central or peripheral field defect, ocular pain, itching, watering, photophobia and mucopurulent discharge. Altered colour vision and poor night vision may also occur.
Decreased Visual Acuity
Decreased visual acuity must always be investigated and the cause found. The cause of a sudden loss of vision could be vascular in nature, such as retinal vein occlusion, retinal artery occlusion or vitreous haemorrhage. It could also be due to acute glaucoma, retinal detachment or inflammatory conditions such as acute uveitis and optic neuritis.
Gradual loss of vision is usually caused by a refractive error, such as myopia or presbyopia, or to degenerative conditions, of which cataract is the most common. It could also be due to macular degeneration or chronic glaucoma.
Distorted Vision
This may be due to macular distortion from an epiretinal membrane, drusen or a choroidal new vessel in wet macular degeneration. Astigmatism and corneal scars can also cause it.
Double Vision (Diplopia)
It is important to note if double vision is true separation of the images or just overlapping, where it may in fact be due to distortion of the image from one eye.
Binocular diplopia is due to extraocular muscle nerve paralysis or muscle injury or dysfunction as in myasthenia gravis.
Monocular diplopia is caused by diseases of the eyeball including cataract, corneal opacity and iris defects.
Floaters
These are small semitranslucent particles of varying shapes which tend to move across the field of vision with eye movements. They are noticeable by almost every adult against a white background and are due to vitreous gel degradation. A sudden onset of floaters with flashes may mean vitreous detachment or vitreous blood from a retinal tear or diabetic retinopathy.
Flashes
Single flashes in one eye, sometimes with eye movement and usually projected to the side, are due to stimulation of the retina by vitreous traction or impending vitreous detachment. Retinal tear must be excluded.
Flickering lights or colour sensations are usually of cerebral origin and most often due to transient vascular changes such as in migraine. They may be bilateral and homonymous in the corresponding part of each visual field.
Eye Pain and Headaches
Scratchy surface pain may be due to dry eyes but occurs with a foreign body or inturned eyelashes, corneal epithelial defects and ulcers.
Deep aching pain may be due to acute glaucoma, iritis, scleritis, trauma and endophthalmitis. These are blinding conditions and severe pain must never be ignored.
Uncorrected refractive error, migraine and neuralgia referred to the eye are common causes of eye ache and may involve more diffuse headache.
Itchy Eyes
Itchy eyes and surrounding skin is often due to allergy. Itch may also occur with blepharitis.
Watering Eyes
In infants, watering is usually due to congenital blockage of the nasolacrimal duct. A rare but important cause is congenital glaucoma.
In adults, watering is caused by blockage of the drainage system or excess production from irritation of the surface, such as with a foreign body, trichiasis, entropion, conjunctivitis and keratitis.
Photophobia
Excess sensitivity to light can be due to a large pupil or damaged iris, acute corneal changes, iritis, cone dystrophy or ocular albinism.
EXAMINATION
Visual Acuity
The assessment of distant and near visual acuity is important, as it reflects the state of the macular function (central vision). The visual acuity can be tested by asking the patient to cover one eye with a cardboard or the palm of his hand. By testing the ability of the patient to see objects such as a clock or newspaper in his own environment, it is possible to get a gross assessment of the visual acuity as blind, grossly defective, subnormal or normal.
Distant visual acuity
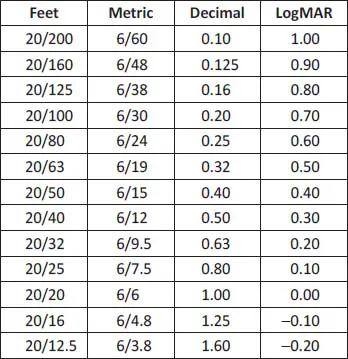
It is usual to record a patient’s distant visual acuity more accurately using the Snellen chart. This is read at 6 m, with the letters diminishing in size from above. The patient has normal vision if he is able to read the line of letters designated as 6/6 at or near the bottom of the chart. The scale for decreasing distant visual acuity is 6/9, 6/12 (industrial vision and requirement for driving), 6/18, 6/24, 6/36 and 6/60 (legal blindness in some countries). Thus, the normal subject can read the 6/18 line at 18 m. Countries which do not use the metric system, including the USA, record Snellen chart findings in feet — 20/20 down to 20/200. Other countries record decimal fractions — 0.1 to 1.0.
Clinical trials and many retinal clinics now use a logMAR (logarithm of the minimum angle of resolution) Bailey–Lovie chart. A Snellen score of 6/12 or 20/40 means that the subject can resolve details down to 2 minutes of the visual angle or a logMAR score of 0.3. This is recorded as the number of actual letters read on the logMAR chart.
If the patient is unable to read the letters, he is asked to count the examiner’s fingers, which are held a metre away. If his answers are correct, he has a distant visual acuity of “counting fingers” at a metre. If he is unable to count the fingers, the examiner should move his hand in front of the patient’s eyes. The visual acuity is then said to be “hand movement”. If he can see only light, the visual acuity is recorded as “perception of light”. If he cannot see any light, the visual acuity is recorded as “no perception of light”, which is total blindness.
Four Ways to Record Visual Acuity Used in Different Countries
Each line on the logMAR chart represents a change of 0.1 log unit in the acuity level, with each of the five letters having a value of 0.02 log unit. Therefore, a patient reading correctly all the letters on a specific line will score the f...