![]()
1
ASK YOUR DENTIST
DO YOU HEAT-STERILIZE YOUR HANDPIECES AFTER EVERY PATIENT?
Everyone should have regular dental care. It not only saves your teeth; it may well save your life. As a microbiologist, I know how important it is to get regular dental checkups and maintain good dental hygiene. But, after conducting research on dental handpieces used to drill and polish teeth, I would never let a dentist or hygienist work on my teeth unless their handpieces have been heat-sterilized after every patient. Many don’t, and you should always ask to make sure.
Key Players
Research conducted by the author and his coauthors at the University of Georgia, Washington University’s Medical School, and Loma Linda University’s School of Dentistry prompted the CDC, the FDA and other public health organizations worldwide to recommend heat-sterilization for every item that enters the oral cavity before it can be reused on another patient.1 There were many key individuals and organizations in government, industry, and academia that fought on one side or the other. Here are some of the key players.
David Kessler, FDA Commissioner
Thomas Arrowsmith-Lowe, who handled dental issues for the FDA, walked into Kessler’s office in 1992 with a copy of our Lancet study and the journal’s editorial in hand. The editors summarized: “On p. 1252, Lewis and colleagues report that HIV-infected material can be sucked back into waterlines and expelled via a dental handpiece.”2 At a meeting at the headquarters of the American Dental Association in Chicago, Tom announced that the FDA was sending a letter to every dentist in the United States, and every possession of the United States, instructing them to heat-sterilize their handpieces after every patient.3
Harold Jaffee, CDC Director
In an interview with ABC Primetime Live producer Sylvia Chase in 1992, Jaffee watched a videotape of me operating a dental drill and “prophy angle” used for cleaning teeth after they had been exposed to blood and prepared for the next patient according to CDC guidelines. Traces of red blood could be seen streaming out as the devices were run over a container of clear water. “Is it not the same thing—this kind of blood transfer—as sharing a needle?” Chase asked.
Dr. Jaffee opened his mouth, but no words came out. After a long pause, he said, “Clearly, we don’t want one patient to be exposed to another’s blood.”
Diane Sawyer introduced the segment by announcing that the CDC had decided to change its guidelines. Dr. Donald Marianos, the head of the CDC’s dental section, called me the next morning to say what an impact the visual demonstration had on the staff at the CDC. Evelyn Lincoln, President Kennedy’s personal secretary, also called me. She said that he would have personally taken action had this surfaced on his watch.
Kimberly Bergalis, University of Florida Student
Despite suffering in the final stages of AIDS, and unable to speak louder than a whisper, Kimberly testified before Congress. She waged a national campaign to force the government to get to the bottom of how she and at least five other patients in a Florida dental practice contracted HIV from their dentist—and stop it from ever happening again. Barbara Webb, a retired schoolteacher who was one of the other five, donated a blood sample for us to use in a study we published in Nature Medicine.
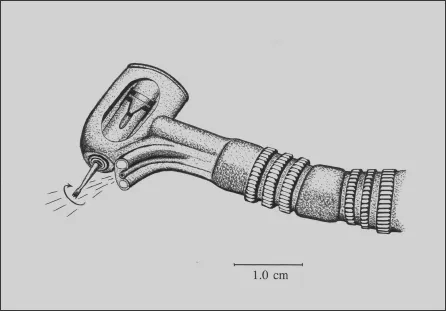
Dental handpiece drawing by David Lewis.
The Story
My older brother Mike joined the Navy in 1962, and was trained as a dental technician. After serving his four years, he worked for a dental supply company in Atlanta, Georgia. While visiting dental practices throughout the Southeast, he noticed traces of blood in the crevices of high-speed dental handpieces prepared for the next patient. Dental handpieces are divided into two categories: high-speed, for drilling, and low-speed, for polishing.
Dental drills run on air pressure controlled with foot-pedals. When the pressure is cut off, suck-back causes blood, saliva, and other patient materials to be drawn back into the handpiece. Although dental handpieces are re-lubricated between patients, they are not cleaned internally.
Slow-speed handpieces used to clean and polish teeth have the same problem. As hygienists scrape plaque from tooth surfaces along the gum line, bleeding occurs. Then, when low-speed handpieces equipped with prophy angles—rotating rubber cups—are run along the gum line, they suck back abrasive pastes contaminated with blood and saliva as the air-flow is disrupted. When reused, they expel the traces of blood and other patient materials directly into areas where tissues are bleeding in subsequent patients.4 Our studies published in Lancet and Nature Medicine demonstrated that, even when the devices are disinfected, they can still expel infectious levels of bacteria and viruses, including HIV.5 Only heat-sterilization can penetrate water-insoluble lubricants containing traces of patient materials trapped inside.
I mentioned to Mike that I often developed throat infections after routine dental procedures, and tested positive for strep throat. When I asked my dentist whether he autoclaved his dental tools, he replied, “Everything but handpieces.” I told Mike that I wanted to take a closer look at what’s inside handpieces, and he gave me an old one to play with. My dentist had assured me that nothing from patients gets inside handpieces because air blows through them during the procedures. So, the first thing I did was to get the contact information for a dental equipment repair company from my brother and give the owner a call. That was in the late 1980s, before the Bergalis case surfaced. I doubt that the owner would have been inclined to talk about the problem after the HIV outbreak caused widespread panic.
When I called the repair shop, I told them I was Mike’s brother and wanted to do a little research on handpiece contamination. I asked, “What do you see inside them when they’re repaired?”
He replied, “Tooth material, amalgam, bits of tissue, blood.”
“Well, if it’s going in,” I said, “then it must be coming back out when the handpiece is reused, right?”
“That’s right,” he replied. To check it out myself, I scooped some of the debris from inside the old handpiece my brother gave me, and took a look at it using an electron microscope with X-ray diffraction to detect heavy metals. Lots of red blood cells, tissue, and mercury-silver amalgam particles were clearly visible.
It was unsettling to me, as a microbiologist, to realize what had been injected into my bloodstream with dental drills over the years. All I could think about was the countless strains of antibiotic-resistant staphylococci and streptococci from thousands upon thousands of patients lodging on my heart valves, and remaining there—a few cells here, a few cells there. Little ticking time bombs buried in some microscopic scar tissue or cholesterol deposit, waiting for my immune system to go downhill from diabetes or some other chronic disease, just sticking it out until I grow old. There’s nothing in the world that can be done about it now.
I asked Mike if he knew any dentists who heat-sterilized their handpieces after every patient. He recommended Robert Boe, a dentist in the Atlanta area who was known for welcoming AIDS patients. Soon, I was taking my wife and two children to Dr. Boe to get our dental work done, and driving to his office after getting off work at EPA to experiment with dental handpieces. Dr. Boe was one of only 1 percent of dentists in the United States who was heat-sterilizing handpieces after each patient at the time.
HIV Outbreak in Florida
In July 1990, the Centers for Disease Control and Prevention (CDC) in Atlanta reported a possible case of HIV transmission in a Florida dental practice.6 It would eventually trace the source of the infection in a University of Florida student, Kimberly Bergalis, and five other patients with no identified risk factors to their dentist, Dr. David Acer.7 In 1991, Dr. Acer’s hometown newspaper published a front-page story about our research, which ran in more than seven hundred papers nationwide.8 One of our studies included a blood sample from one of Acer’s patients.9
The CDC considered the possibility of Dr. Acer directly transmitting his HIV infection to six or more patients through needlestick injuries to be highly improbable. It also considered transmission by dental devices to be highly improbable, but wouldn’t rule it out. The reasoning of CDC scientists was that HIV is highly sensitive to the 2 percent glutaraldehyde solution, which Acer’s staff used to disinfect his handpieces and reusable prophy angles.10 Moreover, a number of patients who contracted the dentist’s HIV only had cleanings done; the CDC considered these procedures to be noninvasive and, therefore, unlikely to transmit HIV.
By exposing reusable prophy angles to blood from HIV-infected patients, we demonstrated that prophy angles used to clean and polish teeth can transmit HIV to cultures of human white blood cells, even after submerging the devices in 2 percent glutaraldehyde for two hours.11 With prophy treatments, or cleanings, the boundaries between doctor and patient dissolve, as dentists have their own teeth cleaned by their hygienists. That’s when visible amounts of the dentist’s blood mix with the clear grease that’s squeezed from a tube into prophy angles between patients.
The reason prophy grease has to be replenished is because it leaks out during use. But it’s not a constant flow. Usually, it builds up until a dark glob of lubricant pops out as the hygienist is polishing a tooth, and then it gets scrubbed down into bleeding tissue with abrasive paste. The reason it’s dark is because it’s laden with blood. In the Florida dental practice where the HIV outbreak occurred, every patient that walked through the door was playing Russian roulette with Dr. Acer, but didn’t know it. That is, not until Kimberly Bergalis would not rest until the state public health department, the CDC, or Congress became involved in finding out how and why she contracted HIV.
By experimenting with dental drills and prophy angles, I noticed visible amounts of blood occasionally coming out of the devices when I ran them in contact with a small amount of water in a porcelain container after they had been used in a bloody dental procedure. And that was after they had been cleaned and disinfected for use on the next patient. When I demonstrated this to my own dentist using prophy angles he had prepared for reuse, he looked down at the floor and said, “My God, I hope I haven’t given my patients hepatitis.” The next day, he instructed his staff to heat-sterilize his handpieces after every patient.
Research Published
Dr. Boe and I published our first paper in the Journal of Clinical Microbiology in 1991, demonstrating that dental handpieces could potentially retract and later eject an amount of blood from previous patients equivalent to a needlestick injury, which carries a risk of infecting one in three hundred patients with HIV.12 We also showed that bacteria in blood could survive the superficial wiping with disinfectants, which is all that most dentists were doing with handpieces between patients. The following year, we submitted a second paper to the same journal, demonstrating that viruses also survived the high-level disinfection procedures recommended by the CDC and FDA. In that study, microbiologists at Loma Linda’s School of Dentistry and the Retrovirus Clinic at Washington University’s School of Medicine participated in the research. All three reviewers recommended that it be published, but the editor-in-chief rejected it.
He explained that our first paper was one of the most controversial the journal had ever published, and that this one would be even more controversial. I reformatted the paper and submitted it to The Lancet in London, while avoiding their editors in Washington, DC. I didn’t want to take a chance on any connections other editors in the US may have had with editors at the Journal of Clinical Microbiology. Lancet quickly accepted the paper with only a few minor grammatical changes.13
More HIV Cases
Compared with the HIV outbreak in Florida, potential problems with reusing unsterilized dental devices on HIV-infected patients were more clearly evident in the dental practice in Springfield, Massachusetts. In June 1989, James Sharpe, who was forty-three years old, made an appointment with Dr. Anthony Breglio. In contrast to Dr. Acer, Breglio was HIV-negative. Jim and his second wife, Jeanne, had recently moved back to Springfield from Miami, Florida. They worked together at the local Easy Quick Country Deli.
Jim hadn’t seen a dentist for years, and was surprised to see how parts of the community where his dentist worked had deteriorated in recent years. He told me that the neighborhood around Breglio’s office was riddled with crack houses, and a large house next to the dental practice had become a house of prostitution. Breglio, he said, even joked about working on the prostitutes. Jim had three teeth extracted, had several cavities filled, and was fitted with a partial denture. According to Jim, Dr. Breglio used a high-speed handpiece to section one of his molars.
Many dentists at the time would extend the burr—which is like a drill bit—then use it to section molars and extract them one piece at a time. This required burying the head of the handpiece in a profusely bleeding wound. This practice, which is not recommended, may be less common today, but it is still being done. About three weeks after having his teeth extracted, Jim developed night sweats and severe fatigue. He tested HIV-positive five months later, then developed AIDS in 1994.
Jim’s physician concluded that his HIV infection was dental-related after an investigation by the state health department failed to discover any other probable cause. A second HIV-infected patient in Breglio’s practice with no identified risk factors later surfaced after giving birth to an HIV-infected baby. Dental records showed that this patient had received dental trea...