
eBook - ePub
Advanced Nutrition and Dietetics in Nutrition Support
Mary Hickson, Sara Smith, Mary Hickson, Sara Smith
This is a test
Share book
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Advanced Nutrition and Dietetics in Nutrition Support
Mary Hickson, Sara Smith, Mary Hickson, Sara Smith
Book details
Book preview
Table of contents
Citations
About This Book
Written in conjunction with the British Dietetic Association, Advanced Nutrition and Dietetics in Nutrition Support provides a thorough and critical review of the fundamental and applied literature in nutrition support.
Extensively evidence-based and internationally relevant, it discusses undernutrition, nutritional screening, assessment and interventions, as well as key clinical conditions likely to require nutrition support, and the approaches to managing this in each of these conditions.
Clinically oriented, Advanced Nutrition and Dietetics in Nutrition Support is the ideal reference for all those managing undernutrition in a range of clinical areas.
Frequently asked questions
How do I cancel my subscription?
Can/how do I download books?
At the moment all of our mobile-responsive ePub books are available to download via the app. Most of our PDFs are also available to download and we're working on making the final remaining ones downloadable now. Learn more here.
What is the difference between the pricing plans?
Both plans give you full access to the library and all of Perlego’s features. The only differences are the price and subscription period: With the annual plan you’ll save around 30% compared to 12 months on the monthly plan.
What is Perlego?
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Do you support text-to-speech?
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Is Advanced Nutrition and Dietetics in Nutrition Support an online PDF/ePUB?
Yes, you can access Advanced Nutrition and Dietetics in Nutrition Support by Mary Hickson, Sara Smith, Mary Hickson, Sara Smith in PDF and/or ePUB format, as well as other popular books in Medicina & Nutrición, dietética y bariatría. We have over one million books available in our catalogue for you to explore.
Information
SECTION 1
Background to undernutrition
Chapter 1.1
Definitions and prevalence of undernutrition
Mary Hickson1 and Sara Smith2
1 Plymouth University Institute of Health and Community, Peninsula Alllied Health Centre, Plymouth, UK
2 Department of Dietetics, Nutrition and Biological Sciences, Queen Margaret University, Edinburgh, UK
1.1.1 Undernutrition: definition and diagnostic criteria
A universal definition for undernutrition is lacking, but it is generally accepted that malnutrition is defined as ‘a state of nutrition in which a deficiency or excess (or imbalance) of energy, protein and other nutrients causes measurable adverse effects on tissue and body form (body shape, size and composition) and function and clinical outcome’ [1]. Such a definition refers to both undernutrition and overnutrition; in this book, the term ‘undernutrition’ is used rather than ‘malnutrition’, to distinguish between the issues of undernutrition and overnutrition.
Global consensus work to develop universal diagnostic criteria and documentation for undernutrition is in progress and is led by the world’s four largest parenteral and enteral nutrition societies [2]. The ongoing work recognises the value of unified terminology, which reflects contemporary understanding and practices, to allow global comparisons and improve clinical care [3] and ultimately aims to seek the adoption of consensus criteria by the World Health Organization and the International Classification of Disease. Early discussions have identified that consensus criteria will need to take account of differences in global practices, such as financial reimbursement and the sometimes limited availability of assessment methods in clinical practice to assess body composition, for example fat‐free mass [2].
Diagnostic criteria have generally focused on dietary intake and clinically relevant changes in body mass (e.g. body mass index (BMI) and involuntary percentage weight loss) [1]. However, it is increasingly recognised that criteria should consider additional factors, such as the presence of acute or chronic inflammation and changes in muscle function [2–5]. This more aetiological approach to diagnosis would allow the recognition of important differences in the pathophysiology of undernutrition and potential response to intervention [5]. The assessment of muscle function and inflammatory markers could therefore result in earlier recognition of risk and the implementation of more effective targeted interventions [4].
The European Society of Enteral and Parenteral Nutrition [3] has proposed a more aetiological approach to the diagnosis of different categories of undernutrition (Figure 1.1.1). These categories are disease‐related undernutrition with inflammation, disease‐related undernutrition without inflammation and undernutrition without disease. However, further work is required to agree specific diagnostic indices for each of these categories. Furthermore, it is acknowledged that some patients may present with mixed aetiologies (e.g. disease‐related undernutrition together with economic‐related undernutrition). This book addresses the causes, consequences and management of undernutrition in the categories outlined in Figure 1.1.1, but the focus is on issues arising primarily in economically developed countries. The book does not attempt to explore the wide‐ranging and complex issues surrounding hunger‐related undernutrition in famine or conflict situations found more frequently in developing countries, particularly affecting children.
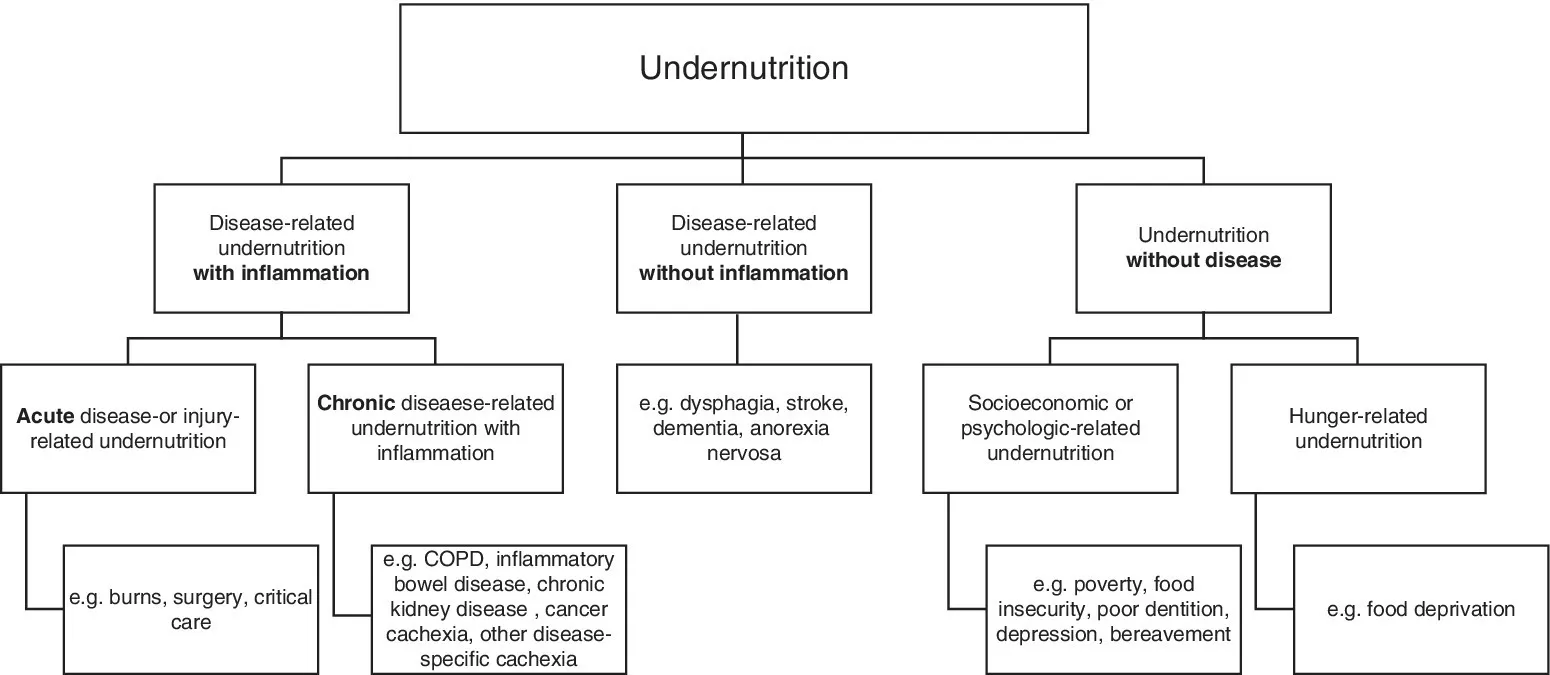
Figure 1.1.1 Diagnosis tree for undernutrition. COPD, chronic obstructive pulmonary disease.
Source: Adapted with permission of Elsevier from Cederholm et al. [3].
1.1.2 Prevalence of undernutrition
The reported prevalence of undernutrition in hospitals varies widely due to differences in study populations, assessment tools and settings. Interpretation of the data is also complicated by small and unrepresentative sample sizes, single‐centre studies, geographical variations, the use of tools without validation and failure to screen the total population. In Europe, several large studies indicate rates in the range of 20–30%, with a higher prevalence in older adults (32–58%) and in cancer (31–39%). Asian studies show a prevalence of 27–39%, again increasing with age (88%), and higher rates in critically ill (87%), surgical (56%) and gastrointestinal malignancy (48%) populations. Similar prevalence is found North America (37–45%) and Australia (23–42%). Prevalence of undernutrition in Latin American hospitals appears to be slightly higher with most studies indicating rates of 40–60%. Consistent with other countries, rates were higher in gastrointestinal surgery patients (55–66%) and older adults (44–71%) [6].
Over 20 years of data are available in the UK since the seminal paper by McWhirter and Pennington [7] was published, and include a national survey called ‘Nutritional Screening Week’ carried out by the British Association of Parenteral and Enteral Nutrition (BAPEN) over a 4‐year period, controlling for the time of the year [8]. This group of datasets shows similar patterns to those described above and also suggests that there has been little change in prevalence during this time [8]. Data on hospital incidence are completely lacking but are extremely challenging to collect and are unlikely to be available unless routine screening and storing in electronic records become the norm.
One obvious factor that will affect undernutrition is food intake during hospital stay. This has been examined by the ‘Nutrition Day’ survey, which is an annual 1‐day survey of hospital patients’ food intake. These important data show that almost half of all hospital patients (n = 91 245) did not eat a full meal. The factors associated with this lower intake are eating less the week before, physical immobility, female sex, old or young age, and a very low BMI [9]. This suggests that interventions to address poor food intake, targeted at those at risk, will be crucial to reduce prevalence of undernutrition in the future.
The prevalence of undernutrition in other settings has also been examined but far fewer data exist. Nursing and residential homes have reported rates of 17–71% for defined undernutrition and up to 97% for those at risk of undernutrition [10]. The UK Nutrition Screening Week data show rates of 41% with little variation across geographical regions or types of care home [11].
Overall, it is clear that undernutrition commonly occurs concurrently with disease and at particular life stages. It is important to note that the methods used to detect undernutrition in prevalence studies are designed to identify protein and energy undernutrition. The identification of micronutrient deficiencies requires different tools and tests.
Despite decades of identifying undernutrition as a prevalent and problematic condition, it remains an elusive challenge in institutional and community settings. Understanding the causes and consequences of undernutrition is essential to subsequently designing multicomponent approaches to reducing its burden.
References
- 1. Todorovic V, Russell CA, Elia M. The ‘MUST’ Explanatory Booklet. A Guide to the Malnutrition Universal Screening Tool (MUST) for Adults. Redditch: BAPEN, 2011.
- 2. Cederholm T, Jensen GL. To create a consensus on malnutrition diagnostic criteria: a report from the Global Leadership Initiative on Malnutrition (GLIM) meeting at the ESPEN Congress 2016. Clin Nutr 2017; 36(1): 7–10.
- 3. Cederholm T, Barazzoni R, Austin P, Ballmer P, Biolo G, Bischoff SC, Compher C, Correia I, Higashiguchi T, Holst M, et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr 2017; 36(1): 49–64.
- 4. Smith S, Madden AM. Body composition and functional assessment of nutritional status in adults: a narrative review of imaging, impedance, strength and functional techniques. J Hum Nutr Diet 2016; 29(6): 714–732.
- 5. White JV, Guenter P, Jensen G, Malone A, Schofield M, Academy of Nu...