
eBook - ePub
Introduction to Neural Engineering for Motor Rehabilitation
Dario Farina, Winnie Jensen, Metin Akay, Dario Farina, Winnie Jensen, Metin Akay
This is a test
Compartir libro
- English
- ePUB (apto para móviles)
- Disponible en iOS y Android
eBook - ePub
Introduction to Neural Engineering for Motor Rehabilitation
Dario Farina, Winnie Jensen, Metin Akay, Dario Farina, Winnie Jensen, Metin Akay
Detalles del libro
Vista previa del libro
Índice
Citas
Información del libro
Neural engineering is a discipline that uses engineering techniques to understand, repair, replace, enhance, or treat diseases of neural systems. Currently, no book other than this one covers this broad range of topics within motor rehabilitation technology. With a focus on cutting edge technology, it describes state-of-the-art methods within this field, from brain-computer interfaces to spinal and cortical plasticity. Touching on electrode design, signal processing, the neurophysiology of movement, robotics, and much more, this innovative volume collects the latest information for a wide range of readers working in biomedical engineering.
Preguntas frecuentes
¿Cómo cancelo mi suscripción?
¿Cómo descargo los libros?
Por el momento, todos nuestros libros ePub adaptables a dispositivos móviles se pueden descargar a través de la aplicación. La mayor parte de nuestros PDF también se puede descargar y ya estamos trabajando para que el resto también sea descargable. Obtén más información aquí.
¿En qué se diferencian los planes de precios?
Ambos planes te permiten acceder por completo a la biblioteca y a todas las funciones de Perlego. Las únicas diferencias son el precio y el período de suscripción: con el plan anual ahorrarás en torno a un 30 % en comparación con 12 meses de un plan mensual.
¿Qué es Perlego?
Somos un servicio de suscripción de libros de texto en línea que te permite acceder a toda una biblioteca en línea por menos de lo que cuesta un libro al mes. Con más de un millón de libros sobre más de 1000 categorías, ¡tenemos todo lo que necesitas! Obtén más información aquí.
¿Perlego ofrece la función de texto a voz?
Busca el símbolo de lectura en voz alta en tu próximo libro para ver si puedes escucharlo. La herramienta de lectura en voz alta lee el texto en voz alta por ti, resaltando el texto a medida que se lee. Puedes pausarla, acelerarla y ralentizarla. Obtén más información aquí.
¿Es Introduction to Neural Engineering for Motor Rehabilitation un PDF/ePUB en línea?
Sí, puedes acceder a Introduction to Neural Engineering for Motor Rehabilitation de Dario Farina, Winnie Jensen, Metin Akay, Dario Farina, Winnie Jensen, Metin Akay en formato PDF o ePUB, así como a otros libros populares de Scienze biologiche y Biotecnologia. Tenemos más de un millón de libros disponibles en nuestro catálogo para que explores.
Información
PART I
Injuries of the Nervous System
Part I contains three chapters that examine the type of neural injuries that may lead to sensory–motor impairment, as well as aspects of plasticity, as a relatively novel conceptual theme in the field of neural rehabilitation. Damage to the nervous system is typically associated with the loss of motor drive and of afferent input to the central nervous system. The severity of the neural damage depends on the location of the injury, which may lead to adaptation of the movement pattern, paresis, or complete paralysis. Plasticity has been defined as changes in the strength, number, and location of synaptic connections in response to either an environmental stimulus or an alteration in synaptic activity in a network; our fundamental understanding of what underlies neural plasticity is believed to be one of the key elements in devising strategies for rehabilitation or repair of injuries.
Chapter 1, by Popović and Sinkjær, provides a review of the incidence and the pathology of major diseases and injuries within the central nervous system that lead to impairment of the sensory–motor system, such as stroke and spinal cord injury. The chapter also briefly introduces the types of injuries that lead to loss of sensory–motor functions at the peripheral level.
Chapter 2, by Navarro, more specifically examines injuries at the peripheral level that may result in partial or total loss of motor, sensory, and autonomic functions. Functional deficits may be compensated by reinnervation of denervated targets by regenerating the injured axons, by collateral branching of undamaged axons, or by remodeling of nervous system circuitries. Plasticity of central connections may compensate functionally for the lack of adequate target reinnervation; however, plasticity has limited effects on disturbed sensory localization or fine motor control after injuries, and it may even result in maladaptive changes, such as neuropathic pain and hyperreflexia.
Obtaining evidence for spinal or cortical plasticity in the human is very difficult without using invasive recording techniques. Chapter 3, by Ivanenko and collaborators, reports on motor primitives to provide a novel perspective on how the neural control system operates under locomotion in healthy subjects and in patients. They find that building blocks with which the central nervous system constructs motor patterns can be preserved in patients with various motor disorders despite the fact that they often modify their muscle activity and adopt motor equivalent solutions. Our understanding of these motor primitives may be useful in driving neuroprostheses or entraining locomotor circuits in disabled people in the future.
Review Chapter
1
Diseases and Injuries of the Central Nervous System Leading to Sensory–Motor Impairment
Summary
Damage to the central and peripheral nervous systems is associated with a loss of motor drive and a defective afferent input to the central nervous system (CNS). Depending on the location and severity of the neural damage this leads to anything from a complete paralysis to a paresis and a maladaptation of the movement pattern. This chapter starts with a presentation of neuron injury. Such injuries are categorized based on the extent and type of damage to the nerve and the surrounding connective tissue. This chapter addresses sensory–motor deficits that are caused by neuron injury or disease: (a) cerebrovascular accident (CVA), or stroke, which causes impairments due to changes in blood supply to the brain; (b) spinal cord injuries (SCIs), which result in total or partial obstruction of flow of both sensory and motor information between the peripheral and central nervous systems; (c) nontraumatic disorders of the CNS (amyotrophic lateral sclerosis and multiple sclerosis); and (d) cerebral palsy. At the end of the chapter we present the incidence of CNS diseases.
Neuron Injury
A neuron injury is categorized based on the extent and type of damage to the nerve and the surrounding connective tissue (Fig. 1.1): neuropraxia, a nerve injury in which the nerve remains intact but with its signaling ability damaged; axonotmesis, in which the nerve remains intact but there with an interruption in conduction of the impulse along the nerve fiber; and neurotmesis, which follows a severe contusion, stretch, laceration, or similar damage. In this case both the axon and the encapsulating connective tissue lose their continuity.
Figure 1.1. Sketch of nerve injury.
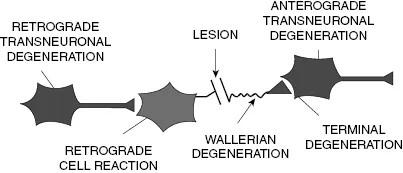
In some injuries, the presynaptic neurons that synapse on the damaged cells are also affected. Transneuronal changes of various kinds are important in explaining why a lesion at one site in the central nervous system (CNS) can have effects on sites distant to the lesion, sites that are distributed according to the connections that the lesion interrupts.
The zone of trauma is a place where a bundle of axons is cut, either by sectioning of a tract within the CNS or by sectioning a peripheral nerve. The part of the axon still connected to the cell body is the proximal segment, and the part isolated from the rest of the cell is the distal segment.
At a zone of trauma in the CNS, the axon and myelin sheath undergo rapid local degeneration. Because a lesion usually interrupts blood vessels, macrophages from the general circulation can enter the area and phagocytose axonal debris. Astrocytes and microglia proliferate and act as phagocytes. In the CNS, however, the proliferation of fibrous astrocytes leads to the formation of a glial scar around the zone of trauma. Scarring can block the course taken by regenerating axons and establish an effective barrier against the reformation of central connections.
The degeneration spreads in both directions along the axon from the zone of trauma, but only for a short distance in the proximal segment, usually up to the point of origin of the first axon collateral. After few days, a retrograde reaction is seen in the cell body. If the entire cell body dies, then degeneration spreads from the axon hillock down along the remainder of the proximal segment. In the distal segment, outside the zone of trauma, the degeneration first appears in the axon terminal about one day after the occurrence of the lesion. In approximately two weeks, the synapses formed by the distal segment degenerate completely. The process is called terminal degeneration. Degeneration of the distal axon, termed Wallerian degeneration, takes place over a period of about two months. Sometime cells that are prior postsynaptic to the injured neuron may also be affected.
The term motor unit refers to the motor neuron in the spinal cord and the population of muscle fibers that it innervates. The motor unit has four functional components: (1) the cell body of the motor neuron, (2) the axon of the motor neuron that runs in the peripheral nerve, (3) the neuromuscular junctions, and (4) the muscle fibers innervated by that neuron.
Most diseases of the motor unit cause weakness and wasting of skeletal muscles. These diseases may differ in other features, however, depending upon which of the four components of the motor unit is primarily affected. A disease can be functionally selective by affecting only the sensory systems or only the motor systems. Motor diseases are regionally selective. They affect only one component of the neuron (e.g., the axon, rather than the cell body).
The clinical consequences of neurogenic disease are most obvious when a peripheral nerve is cut. The muscles innervated by that nerve are immediately paralyzed and then waste progressively. Tendon reflexes are lost immediately, as is the sensation in the area innervated by the nerve because the nerve carries sensory as well as motor fibers. In neurogenic diseases, similar effects of denervation appear more slowly, and the muscles gradually become weak and wasted.
Cerebrovascular Accident
There is a large population of humans that suffer from impairment caused by changes in blood supply of the brain. Blood flow to the brain is highly protected, yet the brain remains highly susceptible to disturbances of the blood supply, as reflected in the high incidence of symptomatic cerebral vascular disease. The term stroke, or cerebrovascular accident (CVA), refers to the neurological symptoms and signs, usually focal and acute, which result from diseases involving blood vessels.
Strokes are either occlusive (due to closure of a blood vessel) or hemorraghic (due to bleeding from a vessel), as sketched in Figure 1.2. Insufficiency of blood supply is termed ischemia; if it is temporary, symptoms and signs may clear with little or no pathological evidence of tissue damage. Ischemia reduces blood supply, thereby depriving tissue of oxygen and glucose, and prevents the removal of potentially toxic metabolites such as lactic acid. When ischemia is sufficiently severe and prolonged, neurons and other cellular elements die; this condition is called infarction.
Figure 1.2. Sketch of the hemorrhagic (left) and ischemic (right) cerebrovascular accident. The right panel shows a magnetic resonance imaging (MRI) scan of a brain after an ischemic stroke.
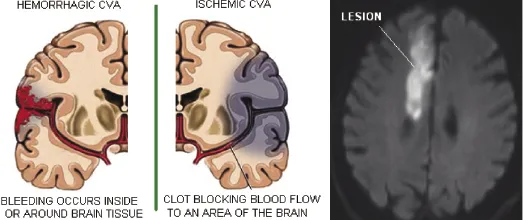
Hemorrhage may occur at the brain surface (extraparenchymal). Alternatively, hemorrhage may be intraparenchymal (e.g., from rupture of vessels damaged by long-standing hypertension), causing a blood clot or hematoma within the cerebral hemispheres, in the brainstem, or in the cerebellum. Ischemia or infarction may accompany hemorrhage. The mass effect of an intracerebral hematoma may compromise the blood supply of adjacent brain tissue; subarachnoid hemorrhage may, by unclear mechanisms, cause reactive vasospasm of cerebral surface vessels, leading to further ischemic brain damage. Infarcted tissue may also become secondarily hemorrhagic.
Each cerebral hemisphere is supplied by an internal carotid artery, which arises from a common carotid artery beneath the angle of the jaw, enters the cranium through the carotid foramen, traverses the cavernous sinus (giving off the ophthalmic artery), penetrates the dura, and divides into the anterior and middle cerebral arteries (Fig. 1.2 and Fig. 1.3).
Figure 1.3. Blood supply of the brain. The large surface branches of the anterior cerebral artery supply the cortex and white matter of the inferior frontal lobe, the medial surface of the frontal and parietal lobes, and the anterior corpus callosum. Smaller penetrating branches supply the deeper cerebrum and diencephalon, including limbic structures, the head of the caudate, and the anterior limb of the internal capsule. The large surface branches of the middle cerebral artery supply most of the cortex and white matter of the hemisphere's convexity, including the frontal, parietal, temporal, and occipital lobes, and the insula. Smaller penetrating branches supply the deep white matter and diencephalic structures such as the posterior limb of the internal capsule, the putamen, the outer globus pallidus, and the body of the caudate. After the internal carotid artery emerges from the cavernous sinus, it also gives off the anterior choroidal artery, which supplies the anterior hippocampus and, at a caudal level, the posterior limb of the internal capsule.
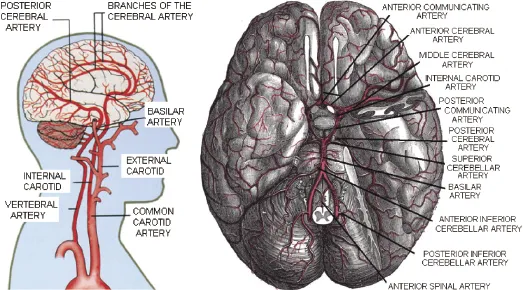
Interconnections between blood vessels (anastomoses) protect the brain when part of its vascular supply is compromised. The anterior communicating artery connects the two anterior cerebral arteries; the posterior cerebral arteries are connected to the internal carotid arteries by the posterior communicating arteries.
Middle Cerebral Artery Territory Infarction
Infarction in the territory of the midd...