Jonathan is not alone. Many people know a lot more about the anatomy of technology than they do about their own bodies—the most precious “machine” they have. Your knee is your body’s most complex joint, a crucial component of what makes you mobile, yet you might be hard-pressed to name parts of your knee beyond kneecap or tendon. There are other key components that you need to know about so you can maintain your knees in optimum health. Do you know how ligaments provide stability to your knees? Can you identify the two types of lubrication and cushioning that protect your knees? Would you be able to identify what is wrong if your knee pain is on the outside or inside of your knee, or in front? In order to prevent or treat any kind of knee pain, you need to know what makes your knees tick, literally and figuratively.
Your knees are built to carry your weight and hold up to a lifetime of walking, running, jumping, dancing, and all that you do in an upright or bent position. There is tremendous variability in the knee’s response to activity, and this can be influenced by age, weight, gender, and genetics. Knees are vulnerable to damage from falls or sudden twisting motions, and are injured, on average, more frequently than other joints. Because your knee is such a complex joint, this chapter will help you understand the structure of your knees and what makes them prone to injury.
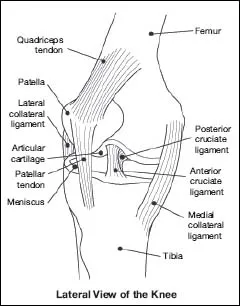
The motion of your knee is complex. It is somewhat like the hinge of a door, moving backward and forward, and like the elbow, it is capable of limited rotation. The knee is made of three bones held together by ligaments and works in coordination with muscles, tendons, cartilage, bursae, synovial fluid, and nerves. Your femur, the bone in your thigh, makes up the top part of the knee, and your tibia, the bone in your shin, the lower part. The third bone is the kneecap, also called the patella, which slides in a groove on the lower end of your thighbone. A fourth bone, the fibula, is a long narrow bone adjacent to your tibia that is connected by a variety of soft tissue structures. The ends of the femur, tibia, and fibula and the back of the patella are lined with articular cartilage, which provides a smooth gliding surface for motion.
FIGURE 1. This side view of the knee shows how the ligaments and tendons connect and support the femur, tibia, and patella. (Courtesy of National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health.)
THE PATELLA: KNEECAP
Your patella is the small triangular bone in the front of your knee. The back of the patella is lined with articular cartilage so that it can glide smoothly in the groove located at the end of your femur. This is the trochlear groove. When you bend and straighten your knee, the patella moves up and down in this groove. Ideally, the patella remains centered in the groove as the knee bends and extends.
Your quadriceps muscles in the front of the thigh, via the quadriceps tendon, attach directly to the upper edge of the kneecap and help to keep it in its groove by exerting a balanced pull on the patella. Any imbalance in these structures, such as muscle weakness or tightness, has the potential to cause patellofemoral problems, including pain or maltracking. The patella is also stabilized by the retinaculum, which are medial and lateral bands of connective tissue that span from the patella to the distal femur, the part farthest from the patella (see below).
If the patella glides laterally toward the outside of the knee in this groove, this is known as patellofemoral maltracking. If the patella transiently comes out of the groove, this is a patellar subluxation and reflects that the patella is not tracking properly. When the patella is completely dislodged from the groove, this means that your kneecap is dislocated. There is an additional structure called the medial patellofemoral ligament (MPFL), a discrete thickening of the medial retinaculum. The strong band of connective tissue is important for patellar stability and can be torn in a patellar dislocation.
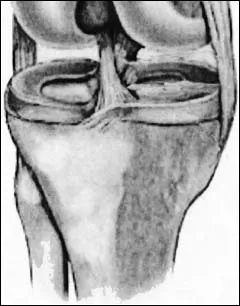
FIGURE 2. This frontal view of the knee with the muscles and tendons peeled back shows the bony alignment. (© Olga Spiegel, 2007.)
LIGAMENTS: THE FOUR STABILIZERS
The four ligaments that stabilize your knee are strong ropelike bands of collagen and elastin that link bone ends together to give mechanical stability to your knee, guide its normal motion, and help prevent abnormal motion. When ligaments are too lax, or loose, they don’t hold your knee bones as firmly. Most laxity results from trauma and may require ligament reconstruction to restore stability. However, there are some people who are “loose jointed.” They have many lax ligaments throughout the body, even without trauma.
The collateral ligaments run along the inner and outer sides of your knee. These are the medial collateral ligament (MCL) and lateral collateral ligament (LCL), respectively. The cruciate ligaments cross diagonally from the back of the femur to the front of the tibia (anterior cruciate ligament, or ACL) and from the front of the femur to the back of the tibia (posterior cruciate ligament, or PCL). The ACL and MCL are the most frequently injured ligaments, but damage can occur to any or all of them. These injuries can be serious and painful because ligaments are slow to heal.
If bones are pulled too far apart, ligament fibers overstretch, resulting in a sprain or tear. Ligament injuries are graded on a scale of 1 to 3, from a mild sprain to a complete tear. This is explained in chapter 7 about diagnosis. It’s important to know these terms because your physician may use them when describing your condition. ACL injuries are common in contact sports, such as two players colliding on a football field, as well as noncontact situations, such as when you plant your foot and pivot suddenly to change direction. If you completely tear your ACL, you will know it immediately. You may feel intense pain, feel or hear a pop in your knee, and experience its giving way or instability. Your knee may swell within the first few hours following the injury even if you have applied ice to it. PCL tears are less common and occur when a force applied to the tibia drives the tibia backward. This can occur with a fall on a bent knee, a dashboard injury during a car accident, or contact with another athlete. The MCL is usually injured by a blow to the outside of the knee while the foot is planted. This force exerts pressure on the inside ligament, forcing the knee into a “knock-kneed” position. With this injury, you may feel a ripping sensation and the sense that your knee is buckling. The LCL is rarely injured by itself, but it can be injured in combination with an injury to the outer aspect of the knee.
Top Sports for Contact ACL Injuries
Basketball
Football
Soccer
Lacrosse
Rugby
Top Sports for Noncontact ACL Injuries
Soccer
Basketball
Skiing
Lacrosse
Field hockey
Pain from sprained ligaments generally gets worse over the first twenty-four hours and is accompanied by knee swelling. The pain from a ligament injury usually gets worse when you walk or bend your knee.
TENDONS:
THE CONNECTION FROM MUSCLE TO BONE
Tendons connect muscle to bone and are among the strongest of any soft tissue in your body. They make it possible to use your muscles to bend and straighten your leg by changing the position of your knee joint. The quadriceps tendon connects the quadriceps muscle on the front of your thigh to the top of your kneecap. The patellar tendon connects your kneecap to the top of your tibia. The hamstring tendons connect the hamstring muscle on the back of your thigh to the tibia and fibula. The medial hamstring tendons attach to the tibia, and the lateral hamstring tendons attach to the fibula. So, essentially, the quadriceps tendon helps you straighten your knee, and the hamstring tendons help you bend it.
Like ligaments, the tendons are bands of tissue. However, they have more densely packed collagen than ligaments and can handle the high tensile loads required during activities such as rowing, running, cycling, jumping, and dancing. Most tendon injuries are caused by overuse, which can result in inflammation (tendinitis) or tendon degeneration (tendinosis), but some tendon injuries are caused by trauma. (See chapter 9 about treatment of tendinitis.)
ARTICULAR AND MENISCAL CARTILAGE:
THE SHOCK ABSORBERS
There are two types of cartilage in your knee that are critically important to its normal function. They act as cushions, or shock absorbers, and help stabilize the knee joint.
Articular Cartilage
Articular cartilage is the smooth, shiny material that covers bone surfaces where they touch so they can glide easily: the ends of the femur, the trochlear groove, the top of the tibia, and the underside of the kneecap. Articular cartilage cannot regenerate, so when it is injured, it can be difficult to treat because time alone will not heal it. Instead, there are ways to resurface areas of traumatic cartilage loss, but these procedures result in formation of a fibrocartilage that is less desirable than articular cartilage. Loss of articular cartilage from aging or trauma results in osteoarthritis and pain. People with cartilage injury often ask if they have arthritis, which they view as a problem of the elderly. By definition, any damage to articular cartilage is a component of arthritis. It can be mild, moderate, or severe, and can affect a limited area of your articular cartilage or all of your cartilage surfaces.
Meniscal Cartilage (The Meniscus)
The cartilage known as the meniscus is made of two C-shaped, padlike structures of fibro-elastic cartilage that separate the surfaces of the femur and tibia. There is a meniscus on the medial and lateral sides of the knee joint. Menisci is the plural for the two crescents that are found in each knee. They have a firm, springy structure and are made of collagen fibers interwoven with a gel-like material (proteoglycans) that, unlike the articular cartilage, can heal in specific regions.
FIGURE 3. This close-up of the top of the tibia shows how the meniscus acts as a cushion between it and the femur. The menisci are two C-shaped pads, one on the inner side of the knee and one on the outer side. (© Olga Spiegel, 2007.)
Tears to the meniscus, commonly known as “torn cartilage,” are a common cause of knee pain in people of all ages. Meniscus tears can cause swelling, stiffness, pain, limitation of motion, and mechanical symptoms such as catching or locking, where the knee feels like it is stuck in an unnatural position. In people under the age of thirty, torn cartilage is generally caused by trauma and related to an event such as a twisting injury. With increasing age, the meniscus begins to degenerate, becoming less springy and more fragile, so a tear can occur with something as simple as bending down to pick up something or playing a routine game of golf or tennis.
You may not notice small tears to the meniscus, but larger tears will usually cause pain and mild to moderate swelling. A displaced flap of torn meniscal cartilage can interfere with knee movement and can cause the knee to lock. Locking can also be caused by a piece of articular cartilage that has broken off and is floating in the joint cavity. This is known as a “loose body.” You may not even notice it is a problem until it interferes with knee movement, like a pencil caught in a door. Locking from a meniscal or flap tear generally causes recurrent symptoms at the same site, while locking from a loose body can occur at different sites or in different knee positions as the fragment floats in the knee.
Cartilage loss—both articular and meniscal—can also be caused by inflammatory conditions such as rheumatoid arthritis and psoriatic arthritis. It is uncommon, but sometimes people are born with a discoid meniscus—that is, a circular pad rather than a crescent-shaped pad, which can predispose a person to meniscus injury (see chapter 4).
SYNOVIUM: THE SOURCE OF LUBRICANT
The synovium is a thin membrane that lines the knee joint and creates synovial fluid. Think of synovial fluid—an excellent natural lubricant—as motor oil for your knee. Just as motor oil keeps a car’s gears from grinding against each other, so the synovial fluid keeps the parts of your knees well lubricated. There is a small amount of synovial fluid produced in a normal joint to provide lubrication for the articula...