
eBook - ePub
Handbook of Cardiac Electrophysiology
Second Edition
Andrea Natale, Oussama M. Wazni, Kalyanam Shivkumar, Francis E. Marchlinski, Andrea Natale, Oussama M. Wazni, Kalyanam Shivkumar, Francis E. Marchlinski
This is a test
Compartir libro
- 440 páginas
- English
- ePUB (apto para móviles)
- Disponible en iOS y Android
eBook - ePub
Handbook of Cardiac Electrophysiology
Second Edition
Andrea Natale, Oussama M. Wazni, Kalyanam Shivkumar, Francis E. Marchlinski, Andrea Natale, Oussama M. Wazni, Kalyanam Shivkumar, Francis E. Marchlinski
Detalles del libro
Vista previa del libro
Índice
Citas
Información del libro
The second edition of this bestseller provides a practical, user-friendly manual guiding the theory and practice of cardiac electrophysiology. The handbook provides the specialist in training with a thorough grounding procedures, and clinical findings for clinicians. It provides a review of the main kinds of arrhythmia with illustrations of typical ECG findings supported where appropriate by correlative imaging. It also details the principal diagnostic and therapeutic procedures include implantation of pacemakers, resynchronization therapy, and ablation techniques.
Key Features
-
- Provides concise, user friendly guide to the equipment, procedures and clinical findings with which EPs need to be familiar
-
- Delivers alternatives resource to the flagship titles available in this field - idea for those beginning training or seeking an update
-
- Presents extensively updated material to enhance comprehension
-
- Includes new treatments and devices for electrophysiologists trained to perform interventional cardiac electrophysiology studies (EPS) as well as surgical device implantations
Preguntas frecuentes
¿Cómo cancelo mi suscripción?
¿Cómo descargo los libros?
Por el momento, todos nuestros libros ePub adaptables a dispositivos móviles se pueden descargar a través de la aplicación. La mayor parte de nuestros PDF también se puede descargar y ya estamos trabajando para que el resto también sea descargable. Obtén más información aquí.
¿En qué se diferencian los planes de precios?
Ambos planes te permiten acceder por completo a la biblioteca y a todas las funciones de Perlego. Las únicas diferencias son el precio y el período de suscripción: con el plan anual ahorrarás en torno a un 30 % en comparación con 12 meses de un plan mensual.
¿Qué es Perlego?
Somos un servicio de suscripción de libros de texto en línea que te permite acceder a toda una biblioteca en línea por menos de lo que cuesta un libro al mes. Con más de un millón de libros sobre más de 1000 categorías, ¡tenemos todo lo que necesitas! Obtén más información aquí.
¿Perlego ofrece la función de texto a voz?
Busca el símbolo de lectura en voz alta en tu próximo libro para ver si puedes escucharlo. La herramienta de lectura en voz alta lee el texto en voz alta por ti, resaltando el texto a medida que se lee. Puedes pausarla, acelerarla y ralentizarla. Obtén más información aquí.
¿Es Handbook of Cardiac Electrophysiology un PDF/ePUB en línea?
Sí, puedes acceder a Handbook of Cardiac Electrophysiology de Andrea Natale, Oussama M. Wazni, Kalyanam Shivkumar, Francis E. Marchlinski, Andrea Natale, Oussama M. Wazni, Kalyanam Shivkumar, Francis E. Marchlinski en formato PDF o ePUB, así como a otros libros populares de Medicina y Teoria, pratica e riferimenti medici. Tenemos más de un millón de libros disponibles en nuestro catálogo para que explores.
Información
Section VIII
CATHETER ABLATION TECHNIQUES
20
ABLATION OF SVT (AVNRT AND AVRT)
Kushwin Rajamani and Patrick Tchou
CONTENTS
Catheter Ablation of AVNRT
Catheter Ablation of AVRT
References
CATHETER ABLATION OF AVNRT
In the common form of typical AtrioVentricular Nodal Reentrant Tachycardia (AVNRT), anterograde conduction occurs through the slow AV nodal pathway, typically localized along the tricuspid annulus just anterior to the coronary sinus (CS) os, while retrograde conduction occurs through the fast pathway localized more superiorly along the mid to anterior part of the septum. Earlier attempts at ablation targeted the fast AV nodal pathway,1,2 proved to be effective in 80%–90% of patients. However, the risk of complete AV block ranged up to 22% due to its close proximity to the compact AV node. Therefore fast pathway ablation is rarely performed now, especially in the context of the safer approach of slow pathway ablation. There are rare and unusual circumstances when fast pathway ablation may be necessary. Those would be described later in the chapter.
SLOW PATHWAY ABLATION
There are two approaches to slow AV nodal pathway ablation. One is called an anatomic approach while the other uses electrogram characteristics to guide ablation. In reality, both approaches use electrogram guidance as well as anatomic landmarks.
ANATOMIC APPROACH
This was first proposed by Jazayery et al.3 and ablation is performed using only anatomic landmarks (Figure 20.1). Ablation has been primarily performed using 4-mm non-irrigated catheters. Contact force ablation catheter with slow flow irrigation is an appealing alternative, which provides good feedback on adequate tissue. The triangle of Koch from the CS os to the His bundle is divided into three regions called the posterior, mid, and anterior regions. Since the tricuspid valve, one of the borders of the triangle, is almost vertically oriented, these three zones can also be anatomically considered inferior, mid, and superior segments along the septal portion of the tricuspid valve. The ablation catheter is placed along the septal edge of the tricuspid annulus just anterior to the CS os (posterior zone) to obtain an AV ratio of 0.1–0.5. The need for fluoroscopy is significantly reduced with the advent of electro-anatomic mapping systems. Furthermore, the inferior boundary of the His could be tagged (His cloud) which serves as a visual marker if encroached during ablation. If AVNRT is still inducible, further RF ablation is applied adjacent to the previous site with a higher AV ratio. This slightly higher ratio moves the catheter slightly away from the tricuspid annulus so as to transect the tail of the AVN—the slow pathway. If unsuccessful, the catheter is moved toward the mid and superior positions again targeting a small AV ratio. initially, this approach achieves a success rate of 95%–99% with an extremely low risk of AV block of 0.6%–0.9%. In rare cases, the slow pathway has left-sided extensions and interrogation of either the proximal coronary sinus or the septal mitral annulus via a transeptal access may be required.
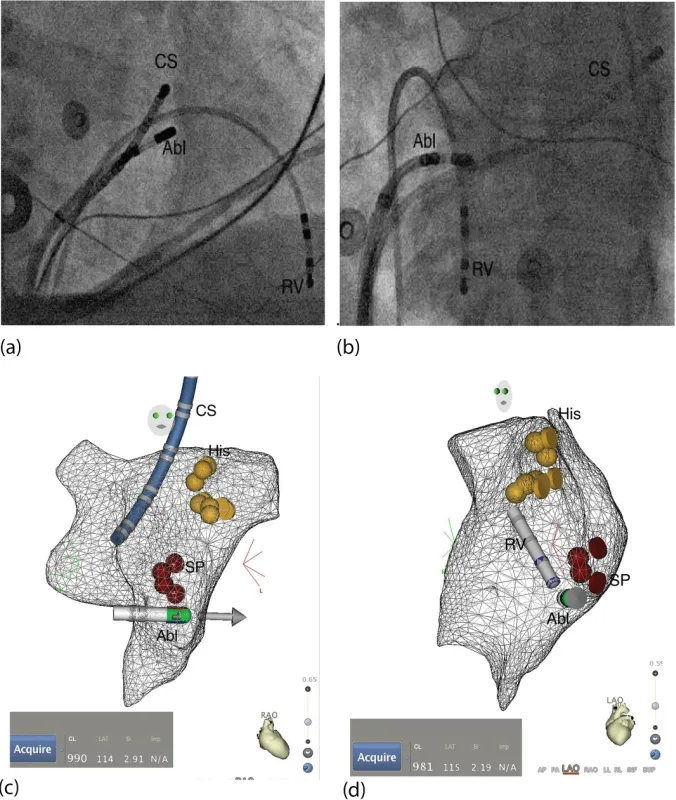
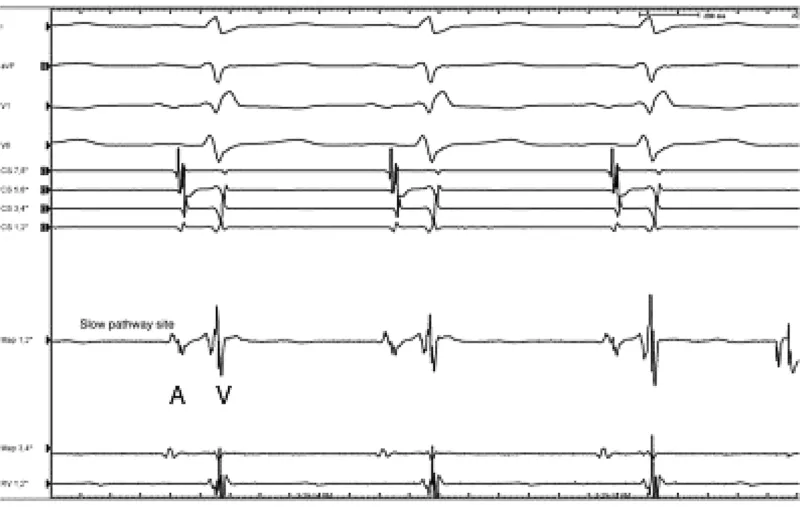
ELECTRO-ANATOMIC APPROACH
This electro-anatomic approach utilizes both endocardial potentials and anatomic markers to guide RF ablation (Figure 20.1). Sun4 described sharp atrial electrograms following a low amplitude atrial electrogram during sinus rhythm. This is recorded around the CS os, usually just anterior to it. Jais5 described the potential recorded at the mid or posterior septum, anterior to the CS. The potential is variable, from sharp to slow with a common AV ratio of 0.5–0.7. Both of these potentials can be recorded simultaneously in the same patient: the sharp potential more inferiorly and the slow potential more superiorly (Figure 20.2). Occasionally, an overlapping zone near the CS os where both potentials can be recorded is present.
In unusual cases, the slow pathway may be located along the mitral annulus or the AV node may have slow pathway extensions along both the tricuspid and mitral annuli. The mitral annular extensions can sometimes be targeted via the anterior wall of the proximal coronary sinus. When ablation along the tricuspid annulus and the proximal coronary sinus fails, the slow pathway may be located along the mitral annulus. Ablating this pathway may require access to the left atrium via a transeptal approach. Locating the site of ablation is similar to the right side approach. The annulus is mapped anatomically. The sites of ablation typically have a smaller A than V electrogram. The compact node near the His bundle should be avoided. The inferior end of the septal mitral annulus should be targeted first with gradual migration of the ablation site superiorly as needed to achieve slow pathway ablation. Junctional rhythm should be monitored during RF application to assure persistence of retrograde conduction, just as during ablation on the right side.
FAST PATHWAY ABLATION
When the slow pathway ablation is not properly targeted, one may generate a situation where typical AVNRT is so readily initiated that it becomes incessant. This scenario occurs when the antegrade fast pathway becomes injured and blocks readily with any premature beat or even during sinus rhythm in a Wenkebach pattern. Alternatively, the antegrade fast pathway may be non-conducting at all. In such circumstances, the retrograde conduction via the fast pathway may still be robust enough to maintain AVNRT. When this occurs, exclusive conduction via the slow pathway can readily initiate AVNRT. The PR Interval in sinus rhythm may well be prolonged already, consistent with slow pathway conduction. Under these circumstances, ablation of the AVNRT would necessitate targeting the fast pathway as eliminating slow pathway conduction would very likely result in high degree AV block if not complete AV block. Mapping of the earliest atrial activation during tachycardia would identify the retrograde fast pathway connection to the...