Chapter 1: Psychiatric illnesses
Chapter 2: Models of mental disorder
Chapter 3: Communication in the clinical mental health setting
Chapter 4: The multidisciplinary team approach to group practice
Chapter 5: Community care and working with carers
Chapter 6: Practical guidelines for service evaluation
Publisher Summary
This chapter discusses the psychiatric illness and different types of symptom clusters. Individual psychiatric illnesses consist of particular clusters of symptoms that recur in different people at different times and places. These symptoms typically consist of a combination of abnormal thoughts and bodily sensations, usually called cognitive and somatic symptoms. In the psychiatric illness of depression, the cognitive symptoms include thoughts of guilt, worthlessness, and hopelessness, whereas the somatic symptoms include loss of energy, sleep, and appetite disturbance, and tiredness. Similarly, in the illness of anxiety state the cognitive symptoms include fearful thoughts of dying, suffocating, collapsing, or making a fool of oneself, while the somatic symptoms may include palpitations, breathlessness, and sweating. In any one individual, a psychiatric illness and personality disorder may coexist, making the treatment for the psychiatric illness less favorable. Likewise, personality disorder and physical illness or disability may coexist and result in difficulties during the rehabilitation phase of the illness. More commonly, dominant personality traits may influence the clinical picture. These traits are of insufficient severity to cause the level of dysfunction associated with personality disorder, but may present clinical management difficulties, particularly in the diagnosis and care of physical illness.
Introduction
One person in four will suffer from a psychiatric illness at some point in their lives, and the risk is particularly high for those who have chronic physical disability or illness. As a physiotherapist, therefore, you are very likely to be working with patients who have psychiatric illness, although since psychiatric symptoms often go undetected you may not always recognize this.
In physically ill people it is sometimes difficult to distinguish between normal emotional responses to stress, and psychiatric illness. Yet this is important, since psychiatric illnesses are generally treatable, thus making it much easier to help with the underlying physical problem. Correspondingly, failure to recognize and help a patient’s psychiatric problem is likely to slow down their physical recovery, particularly where active participation in therapy is needed.
This chapter will explain what is meant by the term ‘psychiatric illness’, and describe the main types you are likely to encounter as a physiotherapist. It will then highlight the reasons why particular individuals become ill, and how common this is. Finally the recognition of psychiatric illnesses, the awareness of particular risk factors, the importance of personality and ways in which people can be helped are described.
What are psychiatric illnesses?
Individual psychiatric illnesses consist of particular clusters of symptoms that recur in different people at different times and places. These symptoms typically consist of a combination of abnormal thoughts and bodily sensations, usually called cognitive and somatic symptoms. For example, in the psychiatric illness of depression the cognitive symptoms include thoughts of guilt, worthlessness and hopelessness, whereas the somatic symptoms include loss of energy, sleep and appetite disturbance, and tiredness. Similarly in the illness of anxiety state the cognitive symptoms include fearful thoughts of dying, suffocating, collapsing or making a fool of oneself, while the somatic symptoms may include palpitations, breathlessness and sweating.
To recognize a psychiatric illness one must detect the cluster or pattern of symptoms. Unlike physical medicine there is rarely a laboratory test to confirm the diagnosis. This is because with most psychiatric illnesses we have yet to find any single underlying physical cause such as a virus. Thus, diagnosis of psychiatric illness is usually determined by whether sufficient key symptoms of a recognized cluster are present.
When does a symptom cluster become an illness?
In psychiatry, there is often a continuum between normality and illness. For example, after major loss or trauma it is natural to develop symptoms of sleep and appetite disturbance, features that are also found in depression. How then can one distinguish between the two?
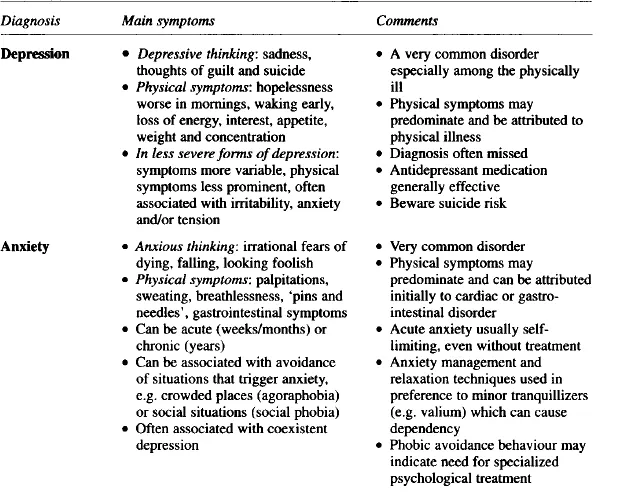
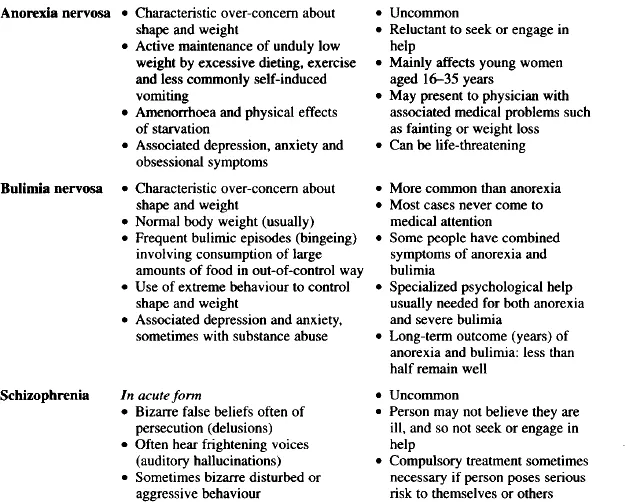
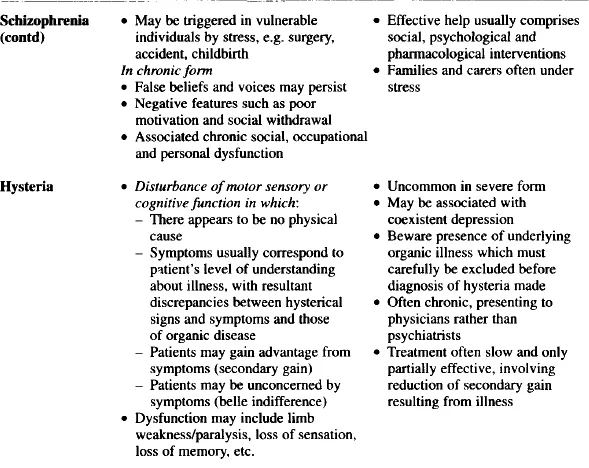
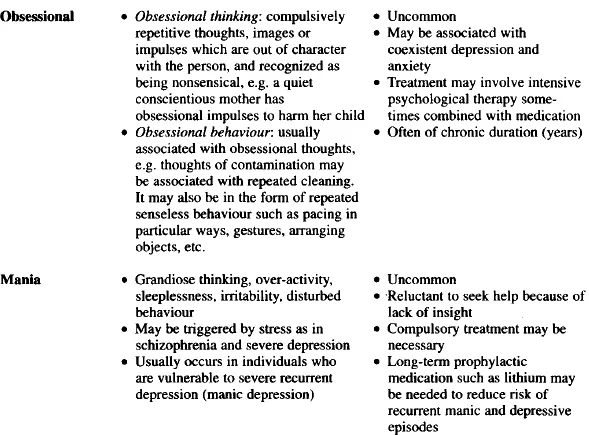
Three things tend to point towards a diagnosis of illness. First, the presence of a full cluster of symptoms. Therefore, in someone coping with a major loss, a diagnosis of depression would need the presence of symptoms of guilt or hopelessness, together with a number of the somatic symptoms summarized in Table 1.1. Secondly, symptoms would normally be persistent, often over a period of weeks if not months. Thirdly, the intensity of symptoms is likely to impair daily living to some degree.
Table 1.1
Diagnosis of psychiatric illness
Thus, where an individual is experiencing psychiatric symptoms, the diagnosis of mental illness depends on whether there is a sufficient clustering of individual symptoms, and on the duration and intensity of these symptoms. If a psychiatric illness is thought to be present this is likely to have specific treatment implications.
What different types of symptom clusters are there?
Broadly speaking there are two groups of psychiatric illnesses. The first comprises those with symptoms which represent a gross exaggeration of experiences that many of us are familiar with; examples include depression, anxiety and obsessional illness. These are sometimes called neuroses. The second comprises those with symptoms totally different from normal experience; examples include schizophrenia and bipolar affective disorder (manic depression). These are sometimes called psychoses.
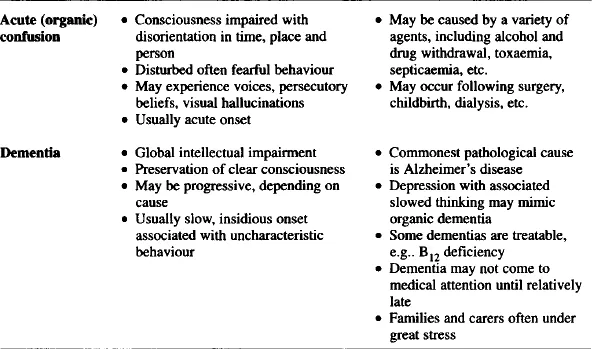
Less frequently, psychiatric illness can be caused by physical factors such as in drug or alcohol withdrawal, endocrine disorders or steroid use. These are usually called organic psychiatric disorders.
In addition to psychiatric illnesses some people suffer from abnormalities of behaviour and personality. If these abnormalities are enough to cause serious persistent disruption in relationships and in employment, then a personality disorder may be present. People with personality disorders are often distressed and needy, are more likely to seek medical attention, and may pose particular difficulties during treatment.
In any one individual, a psychiatric illness and personality disorder may coexist, making the treatment, for the psychiatric illness less favourable. Likewise, personality disorder and physical illness or disability may coexist and result in difficulties during the rehabilitation phase of the illness.
More commonly, dominant personality traits may influence the clinical picture. These traits are of insufficient severity to cause the level of dysfunction associated with personality disorder, but may nevertheless present clinical management difficulties, particularly in the diagnosis and care of physical illness.
Thus, influential personality characteristics may vary across a spectrum from mild (personality trait) to severe (personality disorder). Some of the more commonly encountered personality characteristics likely to be encountered in physical medicine are described later in this chapter.
What are the characteristics of psychiatric illnesses?
Eight important characteristics of psychiatric illnesses are described below.
Common
Psychiatric illnesses are particularly common among general hospital inpatients and general practice and hospital outpatient clinic attenders. Up to a third of attenders have significant psychiatric symptoms, while up to a fifth have a specific psychiatric illness, most commonly depression or anxiety. This is 10 times what one would expect from a general population sample, and in part reflects the stressful nature of physical illness.
Those at particularly high risk of developing psychiatric disorders include people with chronic physical disability or pain, people who have life-threatening illnesses, and people who have lost a significant part of their bodily functioning, for example after a stroke, an amputation or a mastectomy. (In contrast, women undergoing hysterectomy appear to have a particularly low risk of developing psychiatric disorder after surgery.)
Recurrence
Once a person has suffered from a psychiatric illness the risk of recurrence is greater than if they had never had that illness. For example, the risk of a psychotic illness after childbirth increases from 1 in 500 to 1 in 5 if the mother has had a previous psychotic illness. Likewise, a man who has had a history of depression during his life is at particular risk of developing depression following a major health problem such as a heart attack.
Hidden
The presence of a psychiatric illness is often missed, even by experienced clinicians. At least a half of depressive illnesses are missed in hospital and GP clinics, for example. Alcohol dependence and eating disorders, particularly bulimia, are also likely to be missed.
The reasons why certain common psychiatric disorders are so readily missed are various: Depressed patients may fail to recognize their illness, may feel unworthy of asking for help, or may attribute symptoms to physical illness; bulimic patients may be too ashamed to seek help; patients abusing alcohol may deny the problem not only to others but to themselves.
Varied presentation
Psychiatric illness can present in different ways. This is partly because individuals may attac...