![]()
Section 1
Atrial Fibrillation: Background, Evaluation, and Management
![]()
CHAPTER 1
Classification and Epidemiology of Atrial Fibrillation
Faisal Rahman, BMBCh, MA, and Emelia J. Benjamin, MD, ScM
INTRODUCTION
Atrial fibrillation (AF) is the most important clinical arrhythmia globally and affects an estimated 33 million people worldwide.1,2 Our understanding and management of AF have been evolving significantly since the first electrocardiographic AF recordings made by Einthoven3 and Lewis4 over 100 years ago. At the time, the only successful treatment was digitalis, demonstrated by Mackenzie.5 The shifting epidemiology and the increasing morbidity, mortality, social, and healthcare costs have increased the public health importance of AF in low-, middle-, and high-income countries. Providing high-quality management of AF is facilitated by an integrated approach by different members of the healthcare team. To name a few roles, team members may include an internist to assist with rate control, a primary care nurse practitioner for regular follow-up, a pharmacist for anticoagulation, and a visiting nurse to help with adherence and monitoring.
AF is a supraventricular tachycardia defined by uncoordinated electrical and mechanical activity of the atria. Electrocardiographically, AF is distinguished by “irregularly irregular” RR intervals, and therefore ventricular rate, and absence of defined P waves reflecting a lack of synchronized atrial activity. The atrial electrical activity may produce fluctuations of the baseline called fibrillatory or f waves at rates over 300 beats per minute (bpm). The delay in the atrioventricular node ensures that the ventricular rate is usually significantly slower than the atrial rate in the absence of accessory atrioventricular pathways.
CLASSIFICATION
The American College of Cardiology (ACC)/American Heart Association (AHA)/Heart Rhythm Society (HRS)6 and European Society of Cardiology (ESC)2,7 have recommended a clinical classification system according to the duration and method of conversion of AF episodes:
• Paroxysmal: AF that spontaneously terminates within 7 days, majority usually terminate within 48 hours
• Persistent: AF that is present for more than 7 days
• Longstanding persistent: AF present for 1 year or greater
• Permanent: AF present for 1 year or greater when rhythm control is no longer planned or has failed
The first-time AF is recognized regardless of symptoms, duration, or stability, it is known as the first diagnosed or detected AF. If individuals have two or more episodes, then AF is deemed as recurrent. It is not uncommon for individuals to have both paroxysmal and persistent episodes of AF, in which case the ACC/AHA/HRS and ESC guidelines recommend that the most common presentation should be used for classification.6,7
The ACC/AHA/HRS and ESC also distinguish secondary AF when an underlying acute pathology, such as myocardial infarction, myocarditis, and hyperthyroidism, accounts for the AF. Treatment of the primary process is expected to restore sinus rhythm without relapse. However, recent publications have suggested AF occurring in the context of intercurrent illnesses8 or surgery9 may be associated with long-term AF recurrence and other complications.
Lone AF is sometimes used to describe AF in young individuals without secondary causes such as acute illness, hypertension, diabetes mellitus, or cardiopulmonary disease.6 The term is sometimes used to identify patients who do not need anticoagulation and are eligible for treatment with class IC antiarrhythmic agents such as flecainide. However, the use of the term has been inconsistent, and it is increasingly clear that many cases of lone AF may be associated with undiagnosed cardiopulmonary disease. Thus, current guidelines and experts discourage the use of the term “lone AF.”6,10
The ACC/AHA/HRS and ESC classification has superseded the use of the term chronic AF to describe more sustained AF.2,6 Although there are several weaknesses to the ACC/AHA/HRS and ESC schema, because of the simplicity and adoption by major cardiovascular societies, it has become widely accepted.
EPIDEMIOLOGY
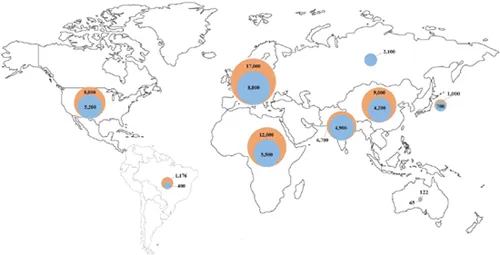
The estimated prevalence of AF in the adult population in the United States, western Europe, and Australia is 1% to 4%,11–16 affecting an estimated 5.2 million in the United States17 and 8.8 million in the European Union18 (Figure 1.1). Over 70% of individuals with AF are over 65 years of age.11,18–20 For example, in large cross-sectional studies in the United States, the prevalence of AF was 0.1% in participants younger than 55 years,14 and over 13% in those over 80 years of age.21 However, screening studies demonstrate that AF often is unrecognized, and thus current reports likely underestimate the actual prevalence of AF.22-24
Figure 1.1
Current estimated prevalence of AF (blue), and 2050 projections worldwide.1,15,17-20,25
There is a dearth of data from low- and middle-income countries, but the available estimates report a lower prevalence (0.3% to 0.9%) in Africa and Asia compared with western Europe and the United States.19,25–29 The 2010 Global Burden of Disease study estimated the worldwide age-adjusted prevalence of AF as 596 per 100,000 men and 373 per 100,000 women, affecting approximately 33 million people.1 In 2010, the incidence rates of AF were 78 per 100,000 person-years in men and 60 per 100,000 person-years in women, increased from 61 in men and 44 in women in 1990.1 AF-associated mortality was higher in women and increased by 2-fold and 1.9-fold in men and women, respectively, from 1990 to 2010.1 There was evidence of significant regional heterogeneity in AF estimations and availability of population-based data.1 With the increasing life expectancy of the population worldwide, the burden of AF has risen in the past two decades1 and is expected to continue to rise. Projections expect the prevalence to approximately double by 2050 in many nations.11,17,18,20,30
The Framingham Heart31 and Rotterdam studies32 evaluated the lifetime risk of AF in individuals of European ancestry. In the Rotterdam Study,32 the lifetime risk of AF at 55 years of age was 22% to 24%, and in the Framingham cohort31 the lifetime risk at 40 years of age was 23% to 26%. Because of the increase in the prevalence of AF with age, the lifetime risk at 70 years of age remains high at 21% to 24%.31
Risk Factors
Aside from advancing age, there is a wide variety of other risk factors associated with AF. The most prevalent risk factors are hypertension and elevated body mass index. In the Atherosclerosis Risk in Communities (ARIC) study, the population-attributable risk for AF was 21.6% for elevated blood pressure and 17.9% for overweight or obesity.33 Other important predictors of AF in both males and females include diabetes mellitus, smoking, myocardial infarction, valvular heart disease,34 heart failure,34,35 hyperthyroidism,36 and atrial structural abnormalities.37
Before wide...