![]()
Management of Concussion
Niranjan A, Lunsford LD (eds): Concussion. Prog Neurol Surg. Basel, Karger, 2014, vol 28, pp 112-127 DOI: 10.1159/000358769
______________________
Evidence-Based Management of Sport-Related Concussion
Michael McCreaa-c · Kevin Guskiewiczd
Departments of aNeurosurgery and bNeurology, Medical College of Wisconsin, and cClement Zablocki VA Medical Center, Milwaukee, Wis., and dDepartment of Exercise and Sport Science, University of North Carolina at Chapel Hill, Chapel Hill, N.C., USA
______________________
Abstract
Concussion is not only one of the most common injuries encountered by athletes participating in contact and collision sports, but also among the most complex injuries to manage in a sports medicine setting. Over the past two decades, we have made great progress in advancing the basic and clinical science of concussion. These advances have had enormous clinical translational value for developing evidence-based guidelines for management of concussion in sports. Applied clinical research has clarified the defining characteristics of sport-related concussion (SRC) that support new diagnostic criteria. At the same time, major advancements have been realized in the development and validation of clinical tools that allow a more objective and accurate assessment of concussion and performance-based measures of recovery. These tools provide clinicians with a more informed basis for determining an athlete's cognitive and physical fitness to return to competition after concussion. Standardized injury management protocols that systematically prescribe rest, graded activity, and return to play have been adopted in nearly all clinical settings. Herein, we briefly summarize the findings and recommendations from several national and international consensus guidelines and position statements on best practice in the evaluation and management of SRC.
© 2014 S. Karger AG, Basel
It is now widely recognized that concussion is not only one of the most common injuries encountered by athletes participating in contact and collision sports, but also among the most complex injuries to manage in a sports medicine setting [1, 2]. A combination of factors often presents the clinician with a unique set of challenges in the diagnoses, evaluation, and management of sport-related concussion (SRC). First, we know that athletes commonly do not report concussive events, either because they do not recognize the signs of injury, they do not consider the injury serious enough to warrant medical attention, or they purposefully mask their injury in order to avoid any lost time from participation [3]. Second, even when reported by the athlete, the clinical effects of concussion are often subtle and difficult to detect on common assessment tools. Third, athletes commonly underreport their postinjury symptoms, falsely inflating their level of recovery in hopes of being more rapidly cleared for return to competition. Fourth, to complicate matters further, ‘signal detection’ on clinical measures (e.g. cognitive and balance testing) often diminishes rapidly in the acute setting of early recovery, making it difficult to precisely determine the athlete’s level of recovery and fitness to resume participation after concussion [4]. Finally, there is now recognition that our clinical assessment of concussion merely represents a surrogate index of recovery, but not a direct measure of the integrity of brain structure and function after concussion. Historically, this set of challenges has hampered the front-line clinician responsible for evaluating athletes with suspected concussion on the sports sideline and objectively determining when the athlete is fit to resume participation.
Over the past two decades, we have made enormous strides toward advancing the basic and clinical science of concussion. In doing so, a new evidence base now informs us on the magnitude of this problem, including large-scale epidemiologic studies indicating the frequency of concussion in contact and collision sports at all competitive levels, including youth sports. We now have a new understanding of the defining characteristics of concussion, on which current definitions of injury and diagnostic criteria are based [5]. Several large prospective studies have described the true natural history of acute clinical effects and recovery, including detailed evidence on the time course in recovery of symptoms, cognitive functioning, balance, and other functional capacities in athletes affected by SRC [4, 6-8]. From the basic science arena, major scientific breakthroughs have shed light on the underlying pathophysiology of concussion, which in turn has implications on our understanding of the time course of physiological effects and recovery after injury [9].
In the spirit of true clinical translation, these research advances have directly impacted the development of evidence-based best practice guidelines for the diagnosis, assessment, and management of SRC, including protocols that drive the decision-making process on an athlete’s fitness to return to participation after concussion. In essence, translational research over the past 20 years has delivered several key findings that to a large extent take the guess work out of concussion management and provide the clinician with parameters for best practice. Several professional organizations have conducted extensive reviews of the existing literature relevant to SRC and developed consensus guidelines based on the available evidence [1, 2, 5, 10]. As would be expected based on their empirical foundation, there is a great deal of consistency and overlap among the current consensus guidelines and position statements.
While the published consensus guidelines and position statements provide a lengthy and detailed set of evidence-based recommendations, our chapter is intended as a brief, high-level summary of the state of the evidence and international consensus on best practice in management of SRC. The publications principally relied on for the purpose of this brief review include those from the American Academy of Neurology (AAN) [5], American Medical Society for Sports Medicine (AMSSM) [2], National Athletic Trainers Association (NATA) [10], and 4th International Consensus Conference on Concussion in Sport [1]. We recommend that clinicians caring for athletes affected by SRC become directly familiar with these specific guidelines statements. Similarly, several accompanying papers in this special issue provide a more detailed and substantive review of the existing literature within specific topic areas (e.g. diagnosis, pathophysiology, neurocognitive testing, special populations, postconcussion syndrome, rehabilitation, etc.), extending beyond the scope of this more global review on evidence-based injury management of SRC.
Evidence-Based Concussion Evaluation and Management
Defining and Recognizing Concussion
One of the major challenges associated with SRC over the years has been the degree of heterogeneity in the clinical presentation of this injury. There has been a fair amount of variability in various concussion definitions developed over the past 30 years, but thankfully with a movement toward greater consensus based on the latest evidence. The Zurich 2012 statement defines concussion as a brain injury characterized by a complex pathophysiological process affecting the brain, induced by biomechanical forces [1]. In a similar vein, the AMSSM defines concussion as a traumatically induced transient disturbance of brain function involving a complex pathophysiological process [2]. In basic terms, all definitions of concussion reference a central tenet of injury to the brain that results in temporary loss of normal brain function. Current guidelines indicate that concussion may be caused either by a direct blow to the head or by forces elsewhere to the body that transmit force to the head.
Central to the concussion definition is the rapid onset of short-lived impairment of neurologic function, which most often and typically resolves spontaneously over a short time frame. What is most evident from research over the past two decades is that unconsciousness, once considered a defining characteristic of concussion, is a relatively infrequent occurrence in a sports settings, with only approximately 10% of athletes having any period of witnessed unconsciousness associated with their injury [4]. Similarly, posttraumatic amnesia is observed in less than 50% of all SRCs. Retrograde amnesia is relatively less common, occurring in less than 25% of athletes [4].
Current guidelines stipulate that concussion is a clinical diagnosis based on the combination of injury mechanism and acute symptoms and signs [1, 2, 5]. In other words, the clinical diagnosis of concussion is based largely on what happened to the athlete at the time of the injury event. The mechanism of injury is an important consideration in ruling out other causes of nonspecific signs or symptoms. Once the mechanism is better delineated, then the astute clinician surveys for a constellations of common signs and symptoms indicative of concussion. Ideally, the diagnosis is formulated by a healthcare provider with expertise and knowledge in the recognition and evaluation of concussion.
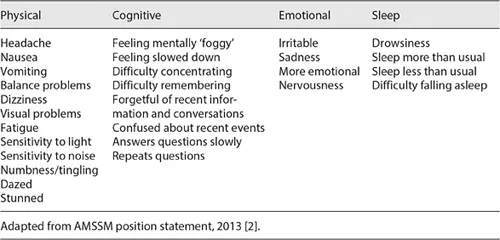
Table 1. Common signs and symptoms of concussion
Concussion often produces a common set of physical, cognitive, behavioral, and other symptoms. Table 1 lists common signs and symptoms observed in the setting of SRC [11]. Along with the established mechanism of injury, these signs and symptoms essentially represent the clinical criteria used to diagnose concussion. It should be noted that several symptoms of concussion are considered nonspecific, meaning that they commonly occur in the context of health conditions other than concussion that are commonly encountered by athletes. Further, certain symptoms may also be common in other comorbid conditions, such as mood disorders, learning disabilities, or other developmental cognitive disorders other than concussion. Therefore, it is essential for the clinician to link the onset of suspected concussion signs and symptoms with an apparent mechanism of injury in order to more precisely isolate concussion as the probable cause of those signs and symptoms. Infrequently, there may be delayed onset of symptoms after concussion, but most often these abnormalities manifest immediately after the head impact in question.
Concussion symptom checklists can provide the clinician with a systematic way to document the presence and severity of concussion symptoms, as well as a method for tracking changes in symptom levels on serial assessment over the course of the athl...