![]()
CATARACTS
| Q | Question 1.1 Viva Stem: How will you Perform Cataract Surgery? |
The most common cataract surgery performed in my center is phacoemulsification. I will perform it under informed consent in the operating theater under peribular anesthesia in sterile conditions. Clean and drape and retract the lids with a Liberman speculum. Create an anterior chamber paracentesis and the clear corneal incision 90 degrees apart, continuous curvilinear capsulorrhexis, hydrodissection, disassembly of the nucleus using stop and chop technique, irrigation and aspiration of soft lens material. Insert intraocular lens into a viscoelastic inflated bag, remove the viscoelastic, and hydrate the wound with subsequent cefazolin gentamicin dexamethasone spray.
| Q | Question 1.2 How would you Define Surge, How do you Reduce Surge, and What are the Phaco Settings that you Use? |
Surge is a result of loss of occlusion under high pressure giving rise to a rapid rate of fluid exit from the anterior chamber resulting in a rise in the posterior capsule.
It can be controlled by reducing the compliance of the tubing as well as allowing for venting. For sculpting, I would use a power of 30 mW and 30 mmHg vacuum at a bottle height of 100 cm. For fragmentation and removal of the nucleus, I will use a power of 20–30 mW with 300 mmHg vacuum at a bottle height of 120 cm. For the last fragment, I will use a power of 15–20 mW with 180 mmHg vaccum at a bottle height of 120 cm. For irrigation and aspiration of soft lens material, I will use 550 mmHg vacuum at a bottle height 100 cm.
| Q | Question 2 Viva Stem: What are the Considerations in Performing Cataract Surgery in a Patient with APAC Two Days Ago? |
Considerations can be divided into preoperative, perioperative, intraoperative and postoperative. Preoperatively, I will control the intraocular pressure medically in the absence of contraindications, check the endothelial cell counts and perform an ultrasound biomicroscopy to assess the degree of zonular laxity, standby anterior vitrectomy, and obtain anterior chamber intraocular lens biometry. If required, I will perform a laser peripheral iridotomy during the acute attack. Perioperatively, I will start the patient on intravenous mannitol (0.5–2 g/kg) if the pressure remains high. I will perform the surgery under peribulbar anesthesia, scrap the epithelium if the view is poor, create a longer more anteriorly placed corneal tunnel, using soft shell technique with dispersive viscoelastic to protect the endothelium and cohesive viscoelastic to maintain anterior chamber depth, refill frequently but avoiding overfill, performing an in situ chop with a sharp second instrument to reduce zonular stress, ensuring complete removal of viscoelastic at the end of surgery. Postoperatively, I will monitor the intraocular pressure and start the patient on topical antibiotics and steroids.
| Q | Question 3.1 Viva Stem: What are the Complications of Cataract Surgery? |
Complications of cataract surgery can be divided into intraoperative, early and late postoperative complications. Intraoperative complications include Descemet membrane detachment, corneal wound burn, iris trauma, capsulorrhexis runout, posterior capsular rupture, dropped nucleus or zonulysis, and suprachoroidal or retrobulbar hemorrhage. Early postoperative complications include hypotony from wound leak, hypertony from inadequate viscoelastic removal, corneal edema, infective endophthalmitis, retained lens fragment, and toxic anterior segment syndrome. Late postoperative complications include retained lens fragment, corneal decompensation, raised intraocular pressure from steroid response, corneal epitheliopathy from antibiotic toxicity, persistent inflammation, posterior capsular opacification, capsular block syndrome, decentered or subluxed intraocular lens, refractive surprise, capsular phimosis, cystoid macular edema, retinal tears or detachment, and chronic endophthalmitis.
| Q | Question 3.2 Intraoperatively, if you note Shallowing of the Anterior Chamber, what are your Differentials? If there is Sudden Deepening, what are your Differentials? |
When shallowing of the anterior chamber occurs, possible causes include suprachoroidal hemorrhage, unstable anterior chamber secondary to leaking wound, machine malfunction/irrigation failure or aqueous misdirection. Sudden deepening can result from lens iris diaphragm retropulsion syndrome, unstable anterior chamber, posterior capsular rupture or hydrorupture, zonulysis with lens tilt, and increased infusion bottle height.
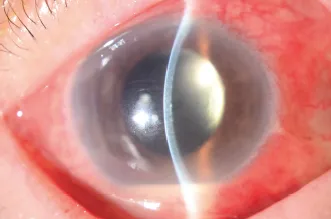
| Q | Question 4.1 Viva Stem: Describe the Photo Shown in Figure 1.1. |
Figure 1.1 This patient has postoperative exogenous endophthalmitis with features of conjunctival injection, hazy cornea, and hypopyon.
This is an anterior segment photograph of the patient’s left eye with a slit beam showing a diffusely injected eye with hazy edematous cornea but no obvious infiltrates. There is presence of hypopyon inferiorly and the patient is pseudophakic. The anterior chamber is deep and there are no obvious lens fragments present. The pupil is regular with no obvious vitreous in the anterior chamber seen. Lid margins appear otherwise normal. This patient likely has a postoperative exogenous endophthalmitis. Other differentials include retained lens fragment and reactivation of underlying uveitis. (TASS is unlikely in this case as there is no limbal-to-limbal corneal edema.) I will check the visual acuity and light projection and relative afferent papillary defect, assess for nasolacrimal duct obstruction (as a risk factor for infection) and intraocular pressures, check the wound for slow leak (less likely if pressure is high and anterior chamber is deep) and vitreous incarceration, look for posterior capsular rupture under the slit lamp and vitreous in the anterior chamber, and examine the fundus for vitritis and retinal detachment. If there is no view, I will perform a B scan and finally examine the fellow eye for risk factors for operative complications. I will examine the patient’s history for the date of surgery, duration and progression of symptoms, compliance to medication and any injury, whether the surgery was complicated and prolonged, and any immunocompromised state.
| Q | Question 4.2 A Patient had Cataract Surgery Four Days Ago and now has Vision with only Light Perception. How would you Manage the Patient? |
The patient likely has postoperative exogenous endophthalmitis until proven otherwise. This is an ocular emergency. Management is dependent on presenting visual acuity and presence of retinal complications such as detachment. In such a patient with presenting vision of light perception, based on the Endophthalmitis Vitrectomy Study, I will refer the patient urgently to the vitreoretinal surgeon and organize an urgent vitrectomy. If the surgery timing is too far away, I will perform immediate vitreous tap and jab in the meantime, sending for gram stain and cultures and injecting intravitreal vancomycin 1 mg in 0.1 mL and ceftazidime 2.25 mg in 0.1 mL in the absence of contraindications, start patient on systemic antibiotics, and admit the patient for monitoring of the progress.
| Q | Question 4.3 What are the Risk Factors for Postoperative Endophthalmitis? |
The risks of postoperative endophthalmitis can be split into patient factors, ocular factors, and operative factors. Patient factors include patients who are immunocompromised such as diabetics, patients who have retroviral infections, patients on immunosuppressive medications, and patients who are non-compliant to eye drops and follow-up visits. Ocular factors include lagophthalmos, exposure, distichiatic lashes, meibomitis, and nasolacrimal duct obstruction. Operative factors include prolonged surgery, wound leak, posterior capsular rupture, dropped nucleus, vitreous adhesion to the wound, or use of silicone lenses.
| Q | Question 4.4 What are the Causes of Chronic Endophthalmitis? |
Causes include propionibacterium acnes, fungal w...