
eBook - ePub
Diabetes Management
A Manual for Patient-Centred Care
Janet Titchener
This is a test
Condividi libro
- 110 pagine
- English
- ePUB (disponibile sull'app)
- Disponibile su iOS e Android
eBook - ePub
Diabetes Management
A Manual for Patient-Centred Care
Janet Titchener
Dettagli del libro
Anteprima del libro
Indice dei contenuti
Citazioni
Informazioni sul libro
Diabetes is a chronic disease involving self-management by the patients. This book teaches providers the skills to translate and transfer complex medical information to empower patients to participate in making well-informed decisions about their own care on a daily basis, as directed by the American Diabetes Association. It provides the basic knowledge around the pathophysiology of diabetes, different management options including insulin management and calculations, information on how foods affect blood sugars and how to address cardiovascular risk factors. This book aims to change clinical outcomes through its unique presentation of information and its approach to awareness.
Key Features
- Follows a unique approach in imparting techniques that bring long-term patient behaviour changes, making the provision of chronic disease management more efficient and satisfying
-
- Serves to help professionals in their day-to-day patient management to achieve better outcomes
-
- Addresses the area of need for primary care and helps to make well-informed decisions by understanding the essential cost of care
-
Domande frequenti
Come faccio ad annullare l'abbonamento?
È semplicissimo: basta accedere alla sezione Account nelle Impostazioni e cliccare su "Annulla abbonamento". Dopo la cancellazione, l'abbonamento rimarrà attivo per il periodo rimanente già pagato. Per maggiori informazioni, clicca qui
È possibile scaricare libri? Se sì, come?
Al momento è possibile scaricare tramite l'app tutti i nostri libri ePub mobile-friendly. Anche la maggior parte dei nostri PDF è scaricabile e stiamo lavorando per rendere disponibile quanto prima il download di tutti gli altri file. Per maggiori informazioni, clicca qui
Che differenza c'è tra i piani?
Entrambi i piani ti danno accesso illimitato alla libreria e a tutte le funzionalità di Perlego. Le uniche differenze sono il prezzo e il periodo di abbonamento: con il piano annuale risparmierai circa il 30% rispetto a 12 rate con quello mensile.
Cos'è Perlego?
Perlego è un servizio di abbonamento a testi accademici, che ti permette di accedere a un'intera libreria online a un prezzo inferiore rispetto a quello che pagheresti per acquistare un singolo libro al mese. Con oltre 1 milione di testi suddivisi in più di 1.000 categorie, troverai sicuramente ciò che fa per te! Per maggiori informazioni, clicca qui.
Perlego supporta la sintesi vocale?
Cerca l'icona Sintesi vocale nel prossimo libro che leggerai per verificare se è possibile riprodurre l'audio. Questo strumento permette di leggere il testo a voce alta, evidenziandolo man mano che la lettura procede. Puoi aumentare o diminuire la velocità della sintesi vocale, oppure sospendere la riproduzione. Per maggiori informazioni, clicca qui.
Diabetes Management è disponibile online in formato PDF/ePub?
Sì, puoi accedere a Diabetes Management di Janet Titchener in formato PDF e/o ePub, così come ad altri libri molto apprezzati nelle sezioni relative a Medicina e Medicina de familia y práctica general. Scopri oltre 1 milione di libri disponibili nel nostro catalogo.
Informazioni
1
The physiology of glucose metabolism
The body is made up of millions of cells. Each cell can be thought of as an engine with a specific job to do – brain cells think, kidney cells make urine, cells in the eye are for seeing, and so on. Like any engine, these cells require fuel to run on. The main fuel that the cells in our body run on is glucose (a simple sugar).
Glucose is transported within the blood and delivered to the cells via blood vessels. The glucose enters each cell through glucose-specific channels or “gates”. For most cells in the body, cellular uptake of glucose can only occur in the presence of insulin, as insulin is needed for opening the gates. In muscle cells, glucose-specific channels can also be opened by exercise (Figure 1.1). Brain cells are the only cells that can receive glucose without assistance from insulin or any other mechanism.
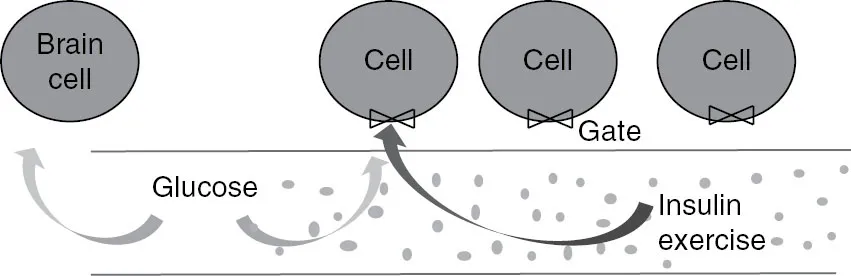
Figure 1.1Glucose enters cells through a glucose-specific ‘gate’, but can only do so if insulin or exercise is also present.
There are two sources of glucose
Our body has two major sources of glucose:
•a continual supply from the liver, and
•a sporadic supply from intestinal absorption of ingested food.
To ensure that there is always a constant supply of glucose available for cells, the body has several places where glucose can be stored and/or generated. The largest and most important of these is the liver. The liver stores glycogen (a storage form of glucose). During fasting, glycogen is broken down into glucose and released into the blood – a process called glycogenolysis. The liver is also capable of making glucose, a process called gluconeogenesis. Through glycogenolysis and gluconeogenesis, the liver constantly releases glucose into the blood, ensuring that fuel is available for the body’s cells 24 hours a day (Figure 1.2).
The second source of glucose is from food. When food is digested, it is broken down into the basic metabolic components of carbohydrates, proteins and fats. These are either used immediately or stored as energy for future use. Ingested carbohydrates (along with a small percentage of ingested protein) are directly converted into glucose in the gut and absorbed into the blood. This blood glucose is taken up immediately by the body’s cells to support bodily functions (e.g. walking, thinking, pumping of the heart), cellular repair and growth. Some of the glucose is transported to the liver to replenish stores and, if we eat more than is needed for current cellular function, the glucose is converted into long-term energy stores – i.e. the person gains weight.
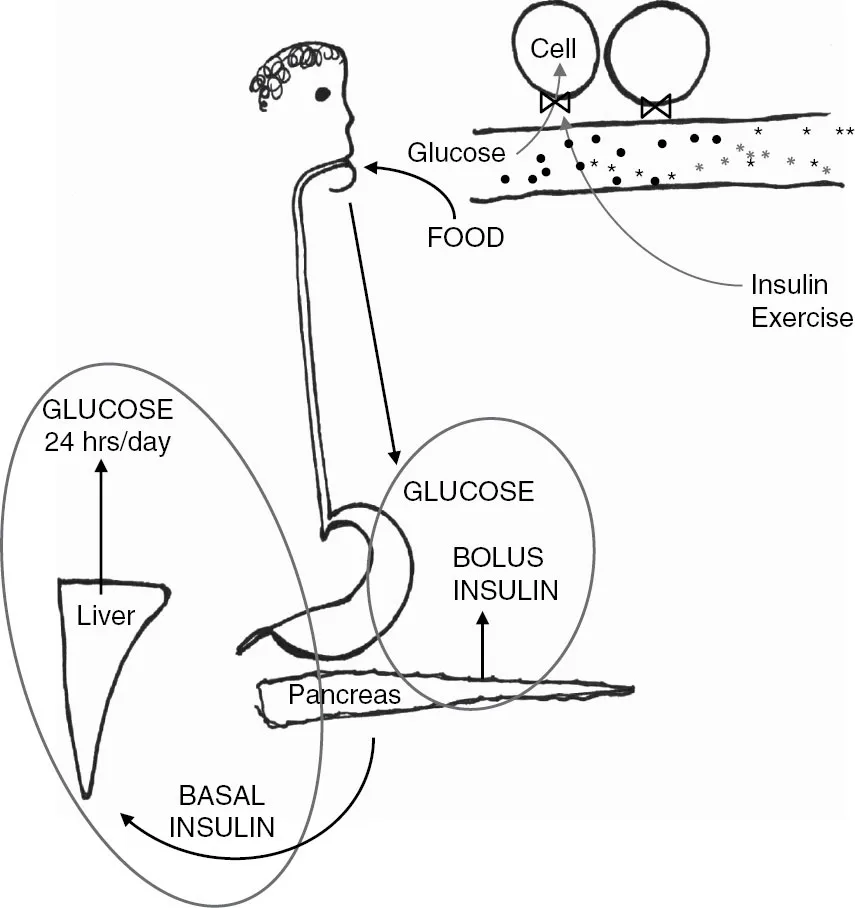
Figure 1.2Two sources of glucose (hepatic and ingestion of foods) are matched by a basal and bolus secretion of insulin from the pancreas.
There are two ‘kinds’ of insulin – basal and bolus
As noted above, except in the brain and in exercising muscle, cellular uptake of glucose can only occur in the presence of insulin. Insulin is a hormone secreted from the pancreatic β-cells. When released into the blood, the insulin binds to specific receptors on the surface of the cells causing the glucose-specific ‘gate’ on the cell membrane wall to open so glucose can enter the cell (Figure 1.2).
Just as glucose is supplied in two different ways, the pancreas provides insulin in two different ways. To match the constant glucose secretion from the liver, the pancreas produces a constant ‘drip’ of insulin, known as the basal insulin (Figure 1.2). The production of pancreatic basal insulin and hepatic glucose are beautifully matched with each other by hormonal feedback loop systems (counter-regulatory systems). This ensures that there is no under- or oversupply of glucose from the liver, and that any glucose released from the liver is appropriately taken up by the cells. Thus, in a person who does not have diabetes, blood sugar levels remain within a narrow range – between 3.5 and 7.8 mmol/L (65–140 mg/dL).
In response to the rapid influx of glucose following a meal, the pancreas immediately releases ‘pre-packaged’ insulin – referred to as a bolus of insulin (Figure 1.2). Depending on the content of the meal, this is then followed by increased insulin synthesis and release, again carefully regulated to match circulating glucose concentrations. This prompt pancreatic action ensures that the cellular glucose uptake can occur instantly and efficiently, which is why the postprandial blood glucose of a person without diabetes does not rise above 7.8 mmol/L (140 mg/dL) regardless of meal volume or content.
Other hormones assist with glucose homeostasis
As our understanding of glucose metabolism has grown, we now know that this representation of insulin as the sole regulator of glucose metabolism is too simplistic. Glucose homeostasis (i.e. keeping blood glucose within normal range) involves multiple pancreatic (insulin, glucagon, amylin) and incretin (gut) hormones (GIP, GLP-1; see below), and there may well be more yet to be discovered (Figure 1.3).
Glucagon This hormone is secreted from the pancreatic α-cells which sit next to the insulin-producing β-cells. Glucagon’s major role is to stimulate hepatic glucose production during the fasting state or when blood sugars go low. During and immediately following a meal, glucagon secretion is suppressed to ensure hepatic glucose output is reduced, as the body does not need two simultaneous sources of glucose.
Amylin This is another pancreatic hormone. It is co-secreted with insulin from the pancreatic β-cells following the ingestion of food. Amylin suppresses postprandial glucagon secretion, thereby decreasing glucagon-stimulated hepatic glucose output (as described above). Amylin also slows the rate of gastric emptying. This reduces the rate at which glucose is delivered to the small intestine for absorption, thereby playing an important role in the control of postprandial blood sugars. By slowing gastric emptying, it is also possible that amylin reduces food intake and body weight – i.e. amylin has similar actions to the incretin hormones (see below).
Incretin (gut) hormones Simplistically, the incretin system can be viewed as an overall coordinator of glucose homeostasis following a meal. Several incretin hormones have now been characterised. The two most significant are GIP (gastric inhibitory polypeptide) and GLP-1 (glucagon-like peptide 1), with GLP-1 considered more physiologically relevant in humans. Both are secreted from cells in the gut (the ‘K’ and ‘L’ cells) following the ingestion of food. The K cells are primarily located in the proximal part of the small intestine (duodenum and jejunum), while the L cells are located more distally in the ileum.
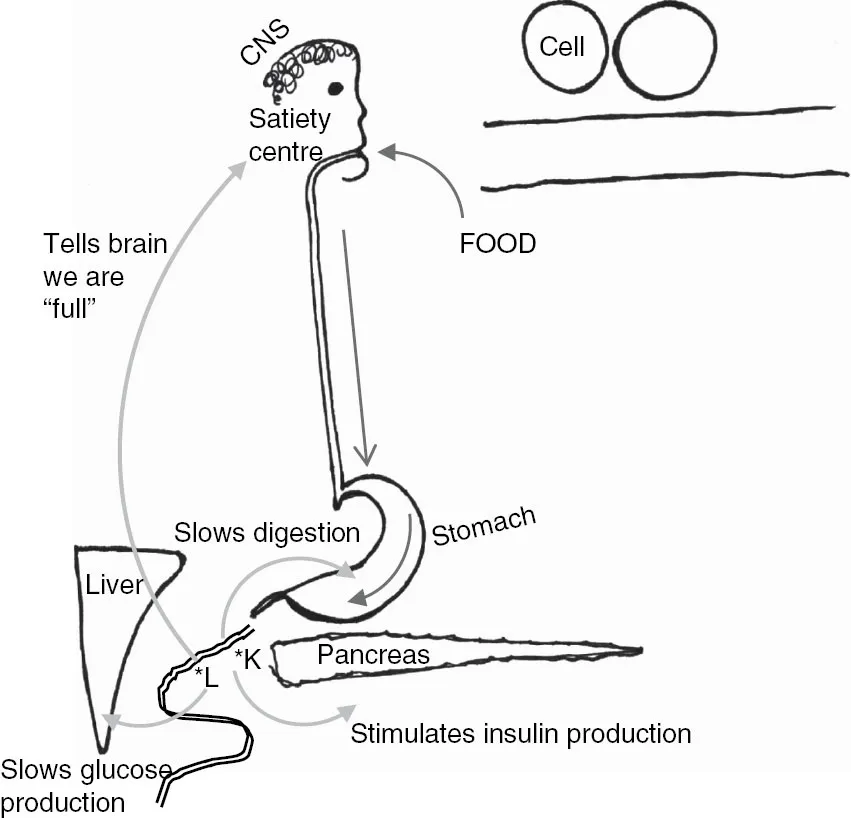
Figure 1.3The incretin system has four targets – the central nervous system (CNS), the stomach, the pancreas and the liver.
The incretin hormones have four actions (Figure 1.3). They
•Stimulate insulin secretion from the pancreatic β-cells (to match incoming food).
•Inhibit glucagon secretion from the pancreatic α-cells (thereby reducing hepatic glucose production).
•Slow gastric emptying (thereby reducing postprandial glucose excursion).
•Stimulate the satiety centre in the central nervous system, i.e. help control appetite.
The kidneys also play a crucial role
The kidneys, like the liver, have glucose stores and contribute to the supply of glucose during periods of fasting. However, the kidneys’ main contribution to glucose homeostasis is through their ability to reabsorb blood glucose that has been filtered through the glomeruli.

Figure 1.4Blood is filtered by the kidneys. In the glomeruli, glucose passes from the blood into renal tubules. The sodium-dependent glucose transporter (SGLT) transports the glucose back into the bloodstream.
The kidneys act as the body’s filter system (Figure 1.4), playing an important role in maintaining the constitution of our blood. Each time the blood circulates around the body, it passes through the glomeruli within the kidneys. The glomeruli act like a filter: large proteins in the blood (e.g. red blood cells, platelets, immunoglobulins) do not pass through the filter and remain in the blood vessel, while the smaller components (e.g. electrolytes, water, glucose) do pass through the filter and into the renal tubules. The tubules are then responsible for determining whether these smaller components should be transported back into the blood or whether they should be excreted.
In a healthy kidney, 100% of the glucose in the blood passes through the glomeruli and into the tubules. But, as glucose is our fuel, the tubules transport 100% of the glucose back into the blood and no sugar appears in the urine. The transporting is done by the sodium-dependent glucose transporter (SGLT) cells located in the proximal renal tubules. Of note, there is a threshold to how much glucose the SGLT cells can transport, so that if they are presented with too much glucose – such as in a person...