
eBook - ePub
Managed Mental Health Care
Major Diagnostic And Treatment Approaches
S. Richard Sauber, S. Richard Sauber
This is a test
Condividi libro
- 272 pagine
- English
- ePUB (disponibile sull'app)
- Disponibile su iOS e Android
eBook - ePub
Managed Mental Health Care
Major Diagnostic And Treatment Approaches
S. Richard Sauber, S. Richard Sauber
Dettagli del libro
Anteprima del libro
Indice dei contenuti
Citazioni
Informazioni sul libro
Published in 1997, Managed Mental health Care is a valuable contribution to the field of Psychiatry/Clinical Psychology.
Domande frequenti
Come faccio ad annullare l'abbonamento?
È semplicissimo: basta accedere alla sezione Account nelle Impostazioni e cliccare su "Annulla abbonamento". Dopo la cancellazione, l'abbonamento rimarrà attivo per il periodo rimanente già pagato. Per maggiori informazioni, clicca qui
È possibile scaricare libri? Se sì, come?
Al momento è possibile scaricare tramite l'app tutti i nostri libri ePub mobile-friendly. Anche la maggior parte dei nostri PDF è scaricabile e stiamo lavorando per rendere disponibile quanto prima il download di tutti gli altri file. Per maggiori informazioni, clicca qui
Che differenza c'è tra i piani?
Entrambi i piani ti danno accesso illimitato alla libreria e a tutte le funzionalità di Perlego. Le uniche differenze sono il prezzo e il periodo di abbonamento: con il piano annuale risparmierai circa il 30% rispetto a 12 rate con quello mensile.
Cos'è Perlego?
Perlego è un servizio di abbonamento a testi accademici, che ti permette di accedere a un'intera libreria online a un prezzo inferiore rispetto a quello che pagheresti per acquistare un singolo libro al mese. Con oltre 1 milione di testi suddivisi in più di 1.000 categorie, troverai sicuramente ciò che fa per te! Per maggiori informazioni, clicca qui.
Perlego supporta la sintesi vocale?
Cerca l'icona Sintesi vocale nel prossimo libro che leggerai per verificare se è possibile riprodurre l'audio. Questo strumento permette di leggere il testo a voce alta, evidenziandolo man mano che la lettura procede. Puoi aumentare o diminuire la velocità della sintesi vocale, oppure sospendere la riproduzione. Per maggiori informazioni, clicca qui.
Managed Mental Health Care è disponibile online in formato PDF/ePub?
Sì, puoi accedere a Managed Mental Health Care di S. Richard Sauber, S. Richard Sauber in formato PDF e/o ePub, così come ad altri libri molto apprezzati nelle sezioni relative a Psychologie e Santé mentale en psychologie. Scopri oltre 1 milione di libri disponibili nel nostro catalogo.
Informazioni
1
Introduction to Managed Mental Health Care: Provider Survival
Viewed by many as the solution to America's health care crisis, managed health care is spawning a revolution in the delivery of mental health services. Whether managing care or managing costs, providers must learn how to manage themselves and their professional skills in order to survive. There is increased employer interest in how health care dollars are spent. New financial arrangements between insurers and providers have reshaped clinical practice to focus on the goals of efficacy and efficiency in behavioral health care.
Practitioners now have to comply with rigorous cost-containment measures and third-party treatment decisions. As a means of controlling costs, short-term treatment and group therapy have replaced traditional long-term analysis. Alarmingly, the dictates of managed care may lead to increased liability for practitioners. Economic survival almost compels single practitioners to join group practices and multidisciplinary groups.
Managed health care is dramatically changing the dynamics of psychological treatment. This handbook examines the complexities of managed care and its ramifications for the mental health field. This introductory chapter focuses on the following topics: the history of managed care; the impact of managed care; the therapist's role in cost containment; accepting change; detriments of managed care; recommendations for improvement; and survival tactics.
Subsequent chapters have been organized to guide providers struggling to understand managed care. They provide the practical tools needed to survive in this new world of big business and organized health care delivery systems. This book helps the clinical provider understand how to meet the needs of both the patient and the managed care company when it comes to the most common basic diagnostic categories: anxiety, depression, adjustment disorders, and marital and family problems. In order to survive, the therapist has to master brief therapeutic interventions, especially group therapy, which will be the primary treatment mode of the future.
It also is essential for the clinician to understand employer assistance programs and how these services are now being organized under the control of managed-care companies. After all, it is the employers of these patients who are paying the bills. It is necessary to teach these employers that mental health benefits are cost-effective. Studies show that depression and other mental disorders cost society billions of dollars annually. A large percentage of that cost is attributable to absenteeism and lost productivity in the workplace. It is important to convince employers that effective psychological treatment can improve health, increase well-being, and actually lower medical expenditures. (See Appendix I, “Mental Health is Cost-Effective,” and Appendix II, “The Economics and Effectiveness of Inpatient and Outpatient Mental Health Treatment” at the end of this chapter.)
In the past, a small number of specialized, nonmainstream mental health caregivers provided personal injury and worker's compensation services. The two services differed in terms of the amount of regulation and fee caps, with worker's compensation being much more rigid. These specialized services are now coming into the mainstream under managed care control. Thus, there are new opportunities for the mental health therapist to become acquainted with these kinds of patients and to provide mental health services that fit with the managed care requirements.
HISTORY OF MANAGED CARE
To understand managed care, it is necessary to understand the history of health care in the United States. Prior to World War II, health care was relatively inexpensive. Most Americans did not have health insurance; they simply paid the family doctor or the hospital when they needed treatment. After the war, medical treatments and the quality of new procedures began to improve greatly, but progress did not come cheap. People realized that they needed some sort of coverage for medical bills, and many employers began to offer health coverage. This worked well for awhile.
Back in the old days, people had a family doctor who knew them and understood their health care needs. But as families grew and moved about, many people found themselves on their own in a confusing world of specialists and ever-changing diagnostic procedures. Many people received care they may not have needed. Costs skyrocketed. Managed care was devised to attack these problems.
The first companies to offer managed mental health care were founded in the 1970s, although attempts to allocate and coordinate the use of resources for mental health services can be traced back to the 1960s in both the public and private sectors. The landmark Community Mental Health Act of 1963, which established a system of community mental health centers (CMHCs), primarily served the needs of America's newly deinstitutionalized chronically mentally ill population. The CMHCs sought to develop a continuum of services for their consumers, focusing on adequate, if not optimal, care with emphasis on outpatient community-based services. A new group of specialists emerged. These community psychiatrists, community psychologists, and community mental health workers, who were employed in community settings, became accustomed to managing minimal public resources to benefit clients most in need of mental health care—a preventive and public health population-based approach.
In the 1960s and 1970s, employers became increasingly aware of the negative impact of alcohol abuse and other personal problems on the productivity of their employers. Some responded by implementing employee assistance programs (EAPs), which originated in earlier employer-sponsored worker-assistance programs for alcoholism. These early programs identified employees in need of mental health or substance abuse services, ensuring appropriate referral to treatment resources. Employers benefited from the cost savings associated with maintaining a healthier work force.
During the late 1970s and 1980s, indemnity insurance coverage for mental health disorders expanded as society became more accepting of psychotherapy and substance abuse rehabilitation. Employers relied on retrospective reviews or, more effectively, on concurrent review processes to validate the need for clinical services for their employees. These processes were often ineffective because neither the providers nor the reviewers of care had the opportunities or incentives to implement treatment plans cooperatively. Employers and benefit consultants believed that providers based treatment planning on benefit maximums rather than on clinical necessity. For example, if the benefit plan allowed for 30 days of inpatient substance abuse care per year, providers often requested 28, 29, or 30 days of inpatient treatment. Some employers responded by restricting or reducing benefits or implementing excessive deductibles for mental health care. An inevitable outcome of this dynamic is that employers might unintentionally deny access to care for employees with clinically significant disorders. To overcome this problem, employers began exploring other approaches to “insuring” care as the costs of mental health care, especially that portion associated with inpatient psychiatric or substance abuse services, skyrocketed in the 1980s.
Many employers turned to health maintenance organizations (HMOs), which have grown steadily in the past decade. Through a gatekeeping system of primary care physicians, management strategies and protocols, management information systems, and capitated financing arrangements, these complex, highly regulated entities served as a partial solution to providing health care to employees. Companies involved with managed mental health care grew as the HMO industry expanded, providing specialized benefit management and clinical services to HMO enrollees. These companies funded their operations through a capitation arrangement with their HMO customers, assuming risk for all mental health care. The capitation form of prospective payment means that a single payment is made for each individual enrolled, regardless of whether that patient requires considerable treatment, a minimal treatment, or no treatment at all.
Several managed mental health care (MMHC) organizations established clinic systems throughout the nation to serve HMO populations (see Figure 1.1, Winegar, 1992).
The latest generation of MMHC systems is the employer-sponsored mental health care provider network (Winegar, 1992). This new benefit
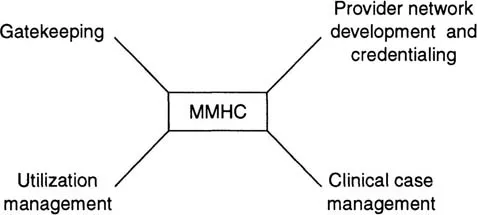
FIGURE 1.1
Model for MMHC organizations.
Model for MMHC organizations.
design is called a network-based product. Consumers are given incentives to use network providers and facilities through reduced out-of-pocket expenses or richer benefit levels. These coverage plans may still provide limited benefits for non-network-delivered services. Benefit designs are sometimes called point-of-service (POS) products, because the consumer determines whether to make use of a network-affiliated professional or facility.
In contrast to traditional indemnity insurance plans, MMHC systems customarily provide utilization review of inpatient care costs to both in-and out-of-network facilities. Reluctant to offer HMO plans (with their reduced choice of providers) alone, these network-based benefit plans provide easy entry into managed-care systems for a growing number of employers who seek increased accountability and cost containment while preserving employee choice of service providers.
By eliminating HMO or indemnity insurance involvement in the mental health care benefit area, employers may also carve out the mental health/substance abuse benefit and contract directly with the MMHC firm through either a capitated arrangem...