eBook - ePub
2021 Endocrine Case Management
Meet the Professor
Bulent O. Yildiz
This is a test
Condividi libro
- English
- ePUB (disponibile sull'app)
- Disponibile su iOS e Android
eBook - ePub
2021 Endocrine Case Management
Meet the Professor
Bulent O. Yildiz
Dettagli del libro
Anteprima del libro
Indice dei contenuti
Citazioni
Informazioni sul libro
2021 Endocrine Case Management: Meet the Professor (MTP) Reference Edition is your source for the latest updates in the diagnosis and management of a wide range of endocrine disorders. This valuable resource allows you to evaluate your endocrine knowledge and gain insight into the strategies used by clinical experts. MTP is updated annually with new cases. Features include:
• Significance of the Clinical Problem
• Key Learning Objectives
• Strategies for Diagnosis and Management
• Clinical Pearls and Pertinent References
• Cases and Questions
Domande frequenti
Come faccio ad annullare l'abbonamento?
È semplicissimo: basta accedere alla sezione Account nelle Impostazioni e cliccare su "Annulla abbonamento". Dopo la cancellazione, l'abbonamento rimarrà attivo per il periodo rimanente già pagato. Per maggiori informazioni, clicca qui
È possibile scaricare libri? Se sì, come?
Al momento è possibile scaricare tramite l'app tutti i nostri libri ePub mobile-friendly. Anche la maggior parte dei nostri PDF è scaricabile e stiamo lavorando per rendere disponibile quanto prima il download di tutti gli altri file. Per maggiori informazioni, clicca qui
Che differenza c'è tra i piani?
Entrambi i piani ti danno accesso illimitato alla libreria e a tutte le funzionalità di Perlego. Le uniche differenze sono il prezzo e il periodo di abbonamento: con il piano annuale risparmierai circa il 30% rispetto a 12 rate con quello mensile.
Cos'è Perlego?
Perlego è un servizio di abbonamento a testi accademici, che ti permette di accedere a un'intera libreria online a un prezzo inferiore rispetto a quello che pagheresti per acquistare un singolo libro al mese. Con oltre 1 milione di testi suddivisi in più di 1.000 categorie, troverai sicuramente ciò che fa per te! Per maggiori informazioni, clicca qui.
Perlego supporta la sintesi vocale?
Cerca l'icona Sintesi vocale nel prossimo libro che leggerai per verificare se è possibile riprodurre l'audio. Questo strumento permette di leggere il testo a voce alta, evidenziandolo man mano che la lettura procede. Puoi aumentare o diminuire la velocità della sintesi vocale, oppure sospendere la riproduzione. Per maggiori informazioni, clicca qui.
2021 Endocrine Case Management è disponibile online in formato PDF/ePub?
Sì, puoi accedere a 2021 Endocrine Case Management di Bulent O. Yildiz in formato PDF e/o ePub, così come ad altri libri molto apprezzati nelle sezioni relative a Medicine e Endocrinology & Metabolism. Scopri oltre 1 milione di libri disponibili nel nostro catalogo.
Informazioni

BONE AND MINERAL METABOLISM
Evaluation of the Patient With Hypophosphatemia
Peter J. Tebben, MD. Division of Endocrinology, Diabetes, Metabolism, and Nutrition, Department of Internal Medicine and Department of Pediatrics and Adolescent Medicine, Mayo Clinic, Rochester, MN; E-mail: [email protected]
Learning Objectives
As a result of participating in this session, learners should be able to:
- Identify clinical manifestations of acute and chronic hypophosphatemia.
- Explain phosphate homeostasis and identify an approach for evaluation of patients with hypophosphatemia.
- Describe therapeutic options for the management of various causes of hypophosphatemia.
Main Conclusions
- Measure serum phosphate and apply the age-appropriate reference range when evaluating patients with unexplained musculoskeletal complaints.
- History and limited laboratory evaluation can establish the underlying etiology of hypophosphatemia.
- Treatment for hypophosphatemia due to poor intake or malabsorption includes phosphate supplementation, dietary changes, and/or treatment of underlying malabsorption disorders.
- Treatment options for hypophosphatemia due to renal phosphate wasting includes active vitamin D and phosphorus replacement or anti-fibroblast growth factor 23 antibody therapy for those with X-linked hypophosphatemic rickets.
- Patients treated with active vitamin D and phosphorus require close monitoring to avoid complications of therapy including secondary/tertiary hyperparathyroidism and nephrocalcinosis/nephrolithiasis.
Significance of the Clinical Problem
Hypophosphatemia is a common clinical abnormality identified in hospitalized patients and has been associated with poor outcomes.1 Chronic hypophosphatemia is less common and requires a systematic approach to determine the underlying etiology and formulate an effective treatment plan. The biological role of phosphorus is diverse, and it is essential for the proper function of a multitude of systems, including having a critical role in skeletal mineralization.2 Disorders that lead to chronic hypophosphatemia are associated with abnormal mineralization and manifest as rickets in children or osteomalacia in adults.3,4
Symptoms of acute hypophosphatemia can be nonspecific and generally reflect the severity and acuity of the decline of the serum phosphate concentration.5 Muscle weakness and fatigue are common symptoms, particularly in those with acquired hypophosphatemia. Cardiac and respiratory dysfunction, as well as rhabdomyolysis and hemolysis, may occur with severe, acute hypophosphatemia.5 However, patients with chronic hypophosphatemia due to heritable causes such as X-linked hypophosphatemic rickets (XLH) generally do not experience these severe symptoms and typically present with skeletal manifestations of rickets and osteomalacia. Serum phosphorus is an important mineral that is frequently overlooked in the evaluation of patients with musculoskeletal complaints, which can lead to significant delays in diagnosis and treatment.6,7
Barriers to Optimal Practice
- Symptoms of hypophosphatemia can be nonspecific and serum phosphate concentrations are not part of routine chemistry panels. Therefore, the diagnosis of hypophosphatemic conditions may go unrecognized or delayed.
- Serum phosphate concentrations are significantly higher in infants and younger children than in adults. As a result, hypophosphatemia may be overlooked if the adult reference range is applied to the pediatric population.
- Understanding the goals and potential adverse effects of therapy for chronic hypophosphatemia are not always appreciated and can lead to adverse outcomes.
Strategies for Diagnosis, Therapy, and/or Management
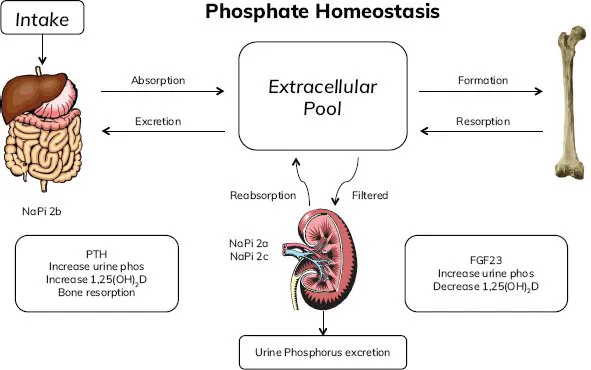
The majority of total body phosphate is found in the skeleton, with the remainder distributed in other tissues and the extracellular space. Many factors affect intestinal absorption and renal reabsorption of phosphorus that influence concentrations measured in the in the blood (Figure 1). The major hormones involved in phosphate homeostasis include 1α-25(OH)2D3 and PTH. However, phosphaturic peptides such as fibroblast growth factor 23 (FGF-23) also have an important role in disorders of phosphate metabolism and this has provided a target for therapeutic intervention in patients with excess FGF-23 due to XLH.8-12
Figure 1. Major Factors in Phosphate Homeostasis
Hypophosphatemia is defined as a serum phosphate concentration below the lower end of normal and is dependent on age. The normal range of serum phosphate in adults is approximately 2.5 to 4.5 mg/dL (0.8-1.5 mmol/L). Infants and children have significantly higher serum phosphate concentrations than adults. It is imperative to use the appropriate reference range in this younger population or the diagnosis of hypophosphatemia may be overlooked.
Hypophosphatemia can be divided into 3 main categories (Table):
- Decreased intake and/or malabsorption
- Redistribution within the body
- Renal phosphate wasting
- FGF-23 mediated
- Non–FGF-23 mediated □ Hyperparathyroidism□ Other
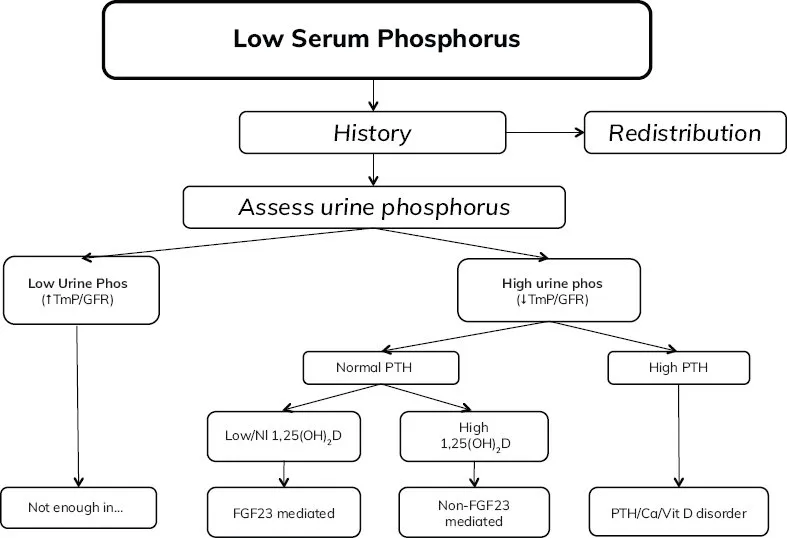
These 3 categories provide a useful framework for evaluation and management of patients with hypophosphatemia (Figure 2).
Decreased Intake and/or Malabsorption
Intestinal absorption of phosphorus is largely dependent on the amount of phosphorus consumed. Absorption takes place primarily in the proximal small bowel with both active and passive mechanisms.13 Decreased intake or malabsorption should be considered in patients with primary malabsorption disorders such as inflammatory bowel disease or short gut syndrome. In addition, patients receiving phosphate binders such as calcium, sevelamer, or lanthanum carbonate can develop hypophosphatemia due to reduced intestinal phosphate availability. Metabolic bone disease (fractures and/or rickets) has been identified in some children receiving an elemental-based infant and child formula thought to be related to low phosphate bioavailability.14,15
Table. Conditions Associated with Hypophosphatemia
| Low Intake or Impaired Absorption | Redistribution | Renal Phosphate Wasting |
| Low phosphate intake Vitamin D deficiency
Malabsorption
Phosphate binders
|
| PTH mediated
FGF-23 mediated
Non–FGF-23 mediated
|
Laboratory Assessment
Figure 2 outlines an approach to the clinical investigation of patients with hypophosphatemia. Most patients can be categorized based on widely available tests, including measurement of serum calcium, phosphate, PTH, creatinine, and vitamin D metabolites. Urinary calcium, phosphate, and creatinine should also be measured. Low urine phosphate with a low fractional excretion of phosphate (less than 5%) is a hallmark of hypophosphatemia caused by inadequate intake or malabsorption. Elevated 1α,25(OH)2D3 concentration is also expected in this category of patients.
Treatment
Treatment for this group of patients is primarily directed at identification and correction of the underlying pathology. If dietary restriction or phosphate binders are the culprit, adjusting the diet or reducing/discontinuing phosphate binders will resolve the hypophosphatemia. Patients with malabsorption due to severe inflammatory bowel disease or short bowel syndrome may require phosphate supplementation if the underlying gastrointestinal pathology cannot be fully corrected. Caution must be exercised in this group, and a low initial dose of phosphorus should be used to avoid worsening gastrointestinal symptoms. Stomach upset and diarrhea are the most common adverse effects of phosphate supplementation.
Redistribution
Hypophosphatemia due to redistribution is typically apparent based on history alone and generally does not require extensive evaluation to establish the etiology. Diabetic ketoacidosis (DKA) and severe malnutrition are states of whole-body phosphate depletion. Serum phosphate is often normal before initiation of treatment for these conditions. However, when insulin is administered to patients with DKA or when feeding is introduced in malnourished patients, cellular uptake of phosphorus ensues, causing hypophosphatemia that is sometimes severe.
Figure 2. Algorithm for Evaluation of Patients With Hypophosphatemia
Hungry bone syndrome is a consequence of calcium and phosphate uptake into bone following surgery for primary hyperparathyroidism. Although most patients do not experience hungry bone syndrome following parathyroidectomy, larger parathyroid adenoma volume, higher alkaline phosphatase, and older age are risk factors for this condition.16
Acute respiratory alkalosis can cause transient hypophosphatemia due to transcellular shifts, is self-limited, and does not require phosphate replacement therapy.
Laboratory Assessment
Limited laboratory testing is needed to establish the cause of hypophosphatemia due to redistribution. However, management of these patients may require more extensive laboratory monitoring. In addition to hypophosphatemia, refeeding syndrome and treatment of DKA are associated with other electrolyte abnormalities that require monitoring and replacement. Vitamin D status should be evaluated in all malnourished patients. Patients with hungry bone syndrome require close monitoring of serum calcium, phosphate, and magnesium, as well as assessment for vitamin D deficiency.
Treatment
Patients with severe malnutrit...