
eBook - ePub
Ocular Surface Disease: Cornea, Conjunctiva and Tear Film E-Book
Expert Consult - Online and Print
Edward J. Holland, Mark J. Mannis, W. Barry Lee
This is a test
Condividi libro
- 472 pagine
- English
- ePUB (disponibile sull'app)
- Disponibile su iOS e Android
eBook - ePub
Ocular Surface Disease: Cornea, Conjunctiva and Tear Film E-Book
Expert Consult - Online and Print
Edward J. Holland, Mark J. Mannis, W. Barry Lee
Dettagli del libro
Anteprima del libro
Indice dei contenuti
Citazioni
Informazioni sul libro
Ocular Surface Disease: Cornea, Conjunctiva and Tear Film incorporates current research and the latest management strategies as well as classification systems and treatment paradigms for all forms of ocular surface disease. This is the first comprehensive resource that helps you to meet ocular surface disease challenges effectively using today's best medical and surgical approaches.
- Get the complete, evidence-based guidance you need to provide optimal care for your patients with ocular surface disease.
- Implement the latest drug treatments and surgical interventions to provide better outcomes with fewer complications.
- Hone and expand your surgical skills by watching videos of leading experts performing advanced procedures including ocular surface transplantation techniques; amniotic membrane transplantation; pterygium surgery; lamellar keratoplasty (DALK) in ocular surface disease; and keratoprosthesis surgery.
- Visualize how to proceed by reviewing detailed, full-color images and consulting new classification systems and treatment paradigms for mild to severe forms of ocular surface disease.
- Take it with you anywhere! Access the full text, downloadable image library, video clips, and more online at expertconsult.com.
Domande frequenti
Come faccio ad annullare l'abbonamento?
È semplicissimo: basta accedere alla sezione Account nelle Impostazioni e cliccare su "Annulla abbonamento". Dopo la cancellazione, l'abbonamento rimarrà attivo per il periodo rimanente già pagato. Per maggiori informazioni, clicca qui
È possibile scaricare libri? Se sì, come?
Al momento è possibile scaricare tramite l'app tutti i nostri libri ePub mobile-friendly. Anche la maggior parte dei nostri PDF è scaricabile e stiamo lavorando per rendere disponibile quanto prima il download di tutti gli altri file. Per maggiori informazioni, clicca qui
Che differenza c'è tra i piani?
Entrambi i piani ti danno accesso illimitato alla libreria e a tutte le funzionalità di Perlego. Le uniche differenze sono il prezzo e il periodo di abbonamento: con il piano annuale risparmierai circa il 30% rispetto a 12 rate con quello mensile.
Cos'è Perlego?
Perlego è un servizio di abbonamento a testi accademici, che ti permette di accedere a un'intera libreria online a un prezzo inferiore rispetto a quello che pagheresti per acquistare un singolo libro al mese. Con oltre 1 milione di testi suddivisi in più di 1.000 categorie, troverai sicuramente ciò che fa per te! Per maggiori informazioni, clicca qui.
Perlego supporta la sintesi vocale?
Cerca l'icona Sintesi vocale nel prossimo libro che leggerai per verificare se è possibile riprodurre l'audio. Questo strumento permette di leggere il testo a voce alta, evidenziandolo man mano che la lettura procede. Puoi aumentare o diminuire la velocità della sintesi vocale, oppure sospendere la riproduzione. Per maggiori informazioni, clicca qui.
Ocular Surface Disease: Cornea, Conjunctiva and Tear Film E-Book è disponibile online in formato PDF/ePub?
Sì, puoi accedere a Ocular Surface Disease: Cornea, Conjunctiva and Tear Film E-Book di Edward J. Holland, Mark J. Mannis, W. Barry Lee in formato PDF e/o ePub, così come ad altri libri molto apprezzati nelle sezioni relative a Medicine e Opthalmology & Optometry. Scopri oltre 1 milione di libri disponibili nel nostro catalogo.
Informazioni
Argomento
MedicineCategoria
Opthalmology & OptometryPart 1
Fundamentals
1
Historical Concepts of Ocular Surface Disease
W. Barry Lee and Mark J. Mannis
Introduction
The ocular surface is the interface between the functioning eye and our environment. This surface provides anatomic, physiologic, and immunologic protection and comprises the palpebral and bulbar conjunctival epithelium, the corneoscleral limbus, the corneal epithelium, and the tear film. While these structures represent the anatomical ocular surface, adnexal structures including the anterior lamellae of the eyelids, eyelashes, meibomian glands, and the lacrimal system are essential for appropriate protection and function of the ocular surface.
The ocular surface functions to maintain optical clarity of the cornea, serves as a refractive surface for accurate projection of light through the ocular media, and provides protection of the structures of the eye against microbes, trauma, and toxins. Creation of an unstable ocular surface from trauma or disease can compromise the integrity of any one of these protective functions and can lead to various forms of corneal and conjunctival dysfunction, broadly ranging from a mild corneal abrasion to severe stem cell loss, decreased vision, and ultimate blindness in the most severe disease. While the health and function of all these structures is imperative for a stable ocular surface, the most important key to anatomic and functional ocular surface stability remains the corneal epithelial stem cells. Our understanding of ocular surface disorders and stem cell physiology has undergone substantial evolution over the last three decades, with remarkable advancements in both corneal epithelial stem cell research as well as medical and surgical techniques for support and restoration of the ocular surface.
Ocular Surface Disease: Advances in Diagnosis & Medical Management
Disorders of the ocular surface include a variety of conditions. Some of the more common conditions encountered in practice include dry eye disease, blepharitis, ocular allergies and pterygia. In addition, less common but more challenging conditions include limbal stem cell deficiency, and ocular surface disease (OSD) from systemic disease (Fig. 1.1). As our understanding of OSD has expanded, the availability of advanced diagnostic tools, medical and surgical therapeutic options, and treatment algorithms for various conditions has enhanced success with OSD. There are classic diagnostic tools for diagnosis of OSD, such as impression cytology, Schirmer testing, tear break-up time, and vital dye staining of the cornea and conjunctiva. These remain valuable tools, however, new diagnostic devices have emerged (Fig. 1.2). Devices, such as tear osmolarity analysis, matrix metalloproteinase-9 analysis, rapid antigen detection for various ocular infectious diseases, and comprehensive analysis of the tear film and lipid are just some of the new diagnostic devices available. Additional advanced diagnostic tools include confocal microscopy, optical coherence tomography (OCT) of the anterior segment, and Scheimpflug imaging of the cornea for advanced diagnosis of various OSD states.1,2 Confocal microscopy enables a detailed investigation of the tarsal and palpebral conjunctiva, central and peripheral cornea, tear film, and eyelids, while affording evaluation of the ocular surface at the cellular level. The device has been particularly useful as a diagnostic tool for cases of atypical keratitis and as a tool to detect phenotypic alterations of the conjunctival epithelium in dry eye disease.1–3
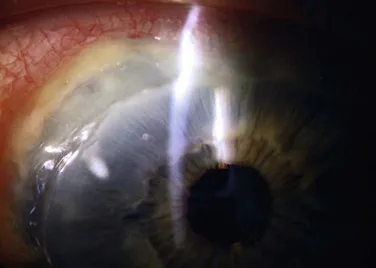
Figure 1.1 Slit lamp photograph of a patient with severe peripheral ulcerative keratitis from rheumatoid arthritis.

Figure 1.2 A slit lamp photograph demonstrating lissamine green staining of the interpalpebral bulbar conjunctiva in a patient with mild symptoms from dry eye disease.
Two of the most common OSD challenges remain dry eye disease and blepharitis. Our knowledge of both of these conditions has expanded over the last few decades with both clinical and basic science research to support the key role of inflammation as a major factor in the development of symptoms and clinical findings of these diseases. The combination of factors leading to dry eye states, often referred to as ‘dysfunctional tear syndrome,’ refers to the compilation of lid margin disease, altered tear film composition, decreased tear volume, diminished corneal sensation, and the presence of anti-inflammatory factors in the tear film.4 The International Dry Eye Workshop (DEWS) included a panel of international ocular surface disease experts challenged to update and review new concepts of dry eye disease. The group developed current concepts of dry eye disease including definition and classification, diagnosis, epidemiology, treatment and management, and research. A fundamental change in our understanding of dry eye is evident in its current definition: ‘Dry eye is a multifactorial disease of the tears and ocular surface that results in symptoms of discomfort, visual disturbance, and tear film instability with potential damage to the ocular surface. It is accompanied by increased osmolarity of the tear film and inflammation of the ocular surface.’4 DEWS provided levels of disease severity with regard to symptoms and signs of dry eye followed by evidence and consensus-based treatment recommendations for dry eye treatment based on new research linking dry eye disease to inflammation.4 Similarly, the Meibomian Gland Workshop involved a panel of international experts challenged to expand our understanding of meibomian gland disease (MGD) (Fig, 1.3). The group developed a contemporary definition and classification of MGD, reviewed methods of diagnosis and evaluation, developed recommendations for the management and therapy of MGD, and presented recommendations for study designs and future research in MGD.5 The treatment recommendations from these workshops have afforded a better understanding of the underlying pathology of dry eye disease, dysfunctional tear syndrome and blepharitis.
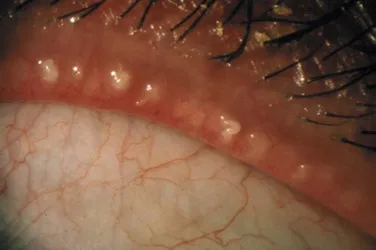
Figure 1.3 High-magnification slit lamp view of severe meibomian gland inspissation in advanced meibomian gland dysfunction.
With expanded diagnostic tools and a better understanding of the pathophysiology of various forms of OSD, we have seen an explosion of new therapeutic strategies from novel medication classes to new therapeutic devices. In the past, treatment options for various conditions, such as dry eye disease were limited to environmental modifications, artificial tears, and punctal plugs. Current medical treatment advances for OSD include new topical and oral therapies for allergic eye disease, limbal stem cell deficiency, and dysfunctional tear syndrome. Topical nonsteroidal anti-inflammatory agents, cyclosporine A, mast cell stabilizer/antihistamine agents, and various new formulations of corticosteroids can aid in difficult inflammatory eye conditions, such as severe atopic keratoconjunctivitis and dysfunctional tear syndrome. Medical management of limbal stem cell deficiency includes therapeutic agents from topical vitamin A formulations to autologous serum, various topical growth factors, oral omega 3 fatty acid supplementation, and topical vascular endothelial growth factor (VEGF) inhibitors to counteract corneal neovascularization. In addition, new therapeutic devices, such as meibomian gland probing, intense pulse light therapy, and LipiFlow® can be additive to topical and oral medication regimens for relief of signs and symptoms of various types of OSD.5
Origins of the Surgical Management of Severe Ocular Surface Disease
An early concept for the surgical treatment of ocular surface disease (OSD) appeared in 1940 with use of amniotic membrane for the repair of conjunctival defects and symblepharon by De Rotth.6 In 1951, Hartman suggested the use of a free conjunctival graft for correction of pterygium, pseudopterygium, and symblepharon.7 This report suggested the benefit of using conjunctiva for grafting procedures and introduced the notion of harvesting conjunctiva from the contralateral eye in selected cases for the surgical treatment...