![]()
The Jacob I. Fabrikant Memorial Address
McDermott MW (ed): Radiosurgery. Basel, Karger, 2010, vol 7, pp 1–17
...........................
Raising Questions and Answering Them: A Personal Approach to Radiosurgery. The 2007 Jacob I. Fabrikant Award Lecture
The 2007 Jacob I. Fabrikant Award Lecture
Douglas Kondziolka
Departments of Neurological Surgery and Radiation Oncology, University of Pittsburgh, and the Center for Image-Guided Neurosurgery, UPMC Presbyterian, Pittsburgh, Pa., USA
An academic career provides the opportunity for a physician to have a leadership role in the advance of a specialty. Investigation and publication are the cornerstones of this effort. What is learned must be shared. Over the past two decades, I have had the opportunity to see a specialty develop from its earliest forms, and to participate in that progress with many hard-working and talented colleagues. Since my first introduction to radiosurgery at the Harvard Cyclotron Unit with Dr. Raymond Kjellberg in 1984, and after my arrival at the University of Pittsburgh in 1989 to learn from Drs. Lunsford, Coffey and Flickinger, I have been influenced by investigators who asked questions. Asking a question and working to come up with a reasonable answer is the foundation of what we do as academic physicians. Dr. Jack Fabrikant worked in such a way, and instilled enthusiasm for research in his trainees. It is an honor to receive this award named for him.
Radiosurgery is perhaps the most ‘minimally invasive’ technique currently applied for the surgical treatment of brain disease and the first widely adopted form of ‘biologic neurosurgery’ [37, 38, 40, 45]. Radiosurgery allows the surgeon to operate at a macromolecular level, via ‘cutting’ of nucleic acids strands, or affecting protein biosynthesis [91]. Because radiosurgery causes differential cellular effects, it has wide application to a variety of cerebral disorders (table 1) [69].
If we are to be biologic surgeons..
What are the effects of a single radiation dose to the brain?
What are the effects of different doses, over time, and in different brain locations?
Our understanding of how radiosurgery should be used will determine how techniques will evolve. Multiple isocenters using narrow radiation beams, or multiple delivery angles, are used to create a three-dimensional radiation volume that matches the imaging-defined tumor margin (i.e. conformality) [18]. Over the last two decades and despite the efforts of many, we have not learned that much about brain and cranial nerve tolerance. We have much work to do. There remains ‘dogma’ about appropriate doses for different cranial nerves or the brainstem. We should remember that many of these concepts were founded on very little data, and should be questioned. Because many targets are adjacent to critical brain and cranial nerve structures, conformal radiosurgery remains crucial to maintain low morbidity rates with high tumor control rates. In 2008, we should work to keep our radiation localized to the target disease, and keep it out of surrounding normal tissue. Devices such as the Perfexion model of the Gamma Knife® use elegant robotics to perform efficient work (fig. 1). Some argue that fractionated stereotactic irradiation is of value [4, 7], and we agree if the planned treatment volume encompasses normal cranial nerves or brain tissue. It should not be a replacement for conformal radiosurgery which provides effective and efficient treatment to the tumor or vascular malformation. Pharmacologic radio-protection with drugs that help mediate radiation injury will be important in the future [21, 50].
What about tumor or AVM doses, in models closer to humans, over longer periods of time?
Radiobiological studies in a sub-human primate model (baboon) were performed at the University of Pittsburgh using an 8-mm collimator and maximum doses of 20, 50, or 150 Gy. The longest-term studies were conducted in animals that received 20 Gy and were followed for 2 years. In these animals, no histologic effects were seen in normal brain, indicating the tolerance of the brain to such a dose commonly delivered to the margin of tumors in humans. Such a study provided evidence for the safety profile of human tumor and AVM radiosurgery.
Table 1. Gamma Knife® radiosurgery at the University of Pittsburgh, 1987-2007 (n = 8,200)
Clinical indication | Procedures n |
Arteriovenous malformation | 1,132 |
Cavernous malformation | 126 |
Arteriovenous fistula | 31 |
Vestibular schwannoma | 1,252 |
Trigeminal schwannoma | 36 |
Other schwannoma | 43 |
Meningioma | 1,126 |
Pituitary tumor | 255 |
Craniopharyngioma | 63 |
Hemangioblastoma | 41 |
Hemangiopericytoma | 32 |
Glomus tumor | 19 |
Pineocytoma | 16 |
Malignant pineal tumor | 13 |
Chordoma | 27 |
Chondrosarcoma | 19 |
Choroid plexus papilloma | 10 |
Hemangioma | 8 |
Glioblastoma multiforme | 305 |
Anaplastic astrocytoma | 122 |
Astrocytoma | 39 |
Oligodendroglioma | 19 |
Pilocytic astrocytoma | 71 |
Ependymoma | 62 |
Medulloblastoma | 21 |
CNS lymphoma | 11 |
Hypothalamic hamartoma | 4 |
Brain metastasis | 2,382 |
Malignant skull base tumor | 44 |
Other tumor | 20 |
Trigeminal neuralgia | 721 |
Sphenopalatine neuralgia | 7 |
Cluster headache | 5 |
Thalamotomy for tremor | 78 |
Mesial temporal lobe epilepsy | 3 |
Obsessive compulsive disorder | 3 |
Cancer pain | 2 |
Fig. 1. The Perfexion model of the Leksell Gamma Knife®, University of Pittsburgh Medical Center.
Skull Base Tumors
Stereotactic radiosurgery has changed the role of the neurosurgeon in the management of cranial base tumors such as meningiomas, schwannomas, pituitary adenomas, craniopharyngiomas, and other lesions [9, 25, 30, 32, 66, 83]. Rather than simply recommending a resection (complete or partial), observation (with an unclear natural history), or fractionated radiation therapy (with limited long-term data except for pituitary tumors)), the surgeon can now provide radiosurgery as primary or in some cases as adjuvant care [90]. Initially, radiosurgery was attractive to patients who were elderly or medically infirm, but later was offered to patients of all ages [2-5] eligible for stereotactic frame fixation. We have found that results have been consistent in both children and adults [16, 17].
How do we maintain cranial nerve function inpatients with acoustic neuromas?
To date we have managed over 1,200 patients with vestibular schwannomas using Gamma Knife® radiosurgery. Initially, patients had radiosurgery as an alternative to microsurgical resection due to one or more of the following criteria: advanced patient age, poor medical condition for surgery, recurrent or residual tumor after prior surgery, neurofibromatosis type II, or patient preference [16, 18, 42, 87]. Symptoms before radiosurgery included hearing loss (92%), balance symptoms or ataxia (51%), tinnitus (43%), or other neurologic deficit (19.5%). 34% had useful hearing (253 total), Gardner-Robertson grade I (speech discrimination score ≥70%; pure tone average ≤30 dB) or grade II (speech discrimination score ≥50%; pure tone average ≤50 dB). Over the last 15 years, the average dose to the tumor margin was 13 Gy.
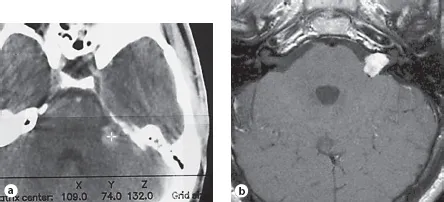
Fig. 2. Axial CT image of a left vestibular schwannoma in a 36-year-old man at radio-surgery (a), and at 20 years (b), showing long-term tumor regression.
In two separate outcomes evaluations, we found that the clinical tumor control rate (no requirement for surgical intervention) was 98% at 5-10 years [16, 42]. The key to good outcomes included magnetic resonance imaging (MRI)-based planning, use of multiple isocenters with smaller radiation beams, and a tumor margin dose in the range of 12-13 Gy [18]. We think that an evaluation of middle ear structures will be important to improve outcomes further. Our typical margin dos...