eBook - ePub
Evidence-Based Emergency Care
Diagnostic Testing and Clinical Decision Rules
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Evidence-Based Emergency Care
Diagnostic Testing and Clinical Decision Rules
About this book
This book for emergency physicians and fellows training in emergency medicine provides evidence-based information on what diagnostic tests to ask for and when and how to use particular decision rules. The new edition builds on the success of the current book by modifying the presentation of the evidence, increasing the coverage, and updating the current information throughout.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Evidence-Based Emergency Care by Jesse M. Pines, Christopher R. Carpenter, Ali S. Raja, Jeremiah D. Schuur, Jesse M. Pines,Christopher R. Carpenter,Ali S. Raja,Jeremiah D. Schuur in PDF and/or ePUB format, as well as other popular books in Medicine & Medical Theory, Practice & Reference. We have over one million books available in our catalogue for you to explore.
Information
Section 1
The Science of Diagnostic Testing and Clinical Decision Rules
Chapter 1
Diagnostic Testing in Emergency Care
As emergency department (ED) physicians, we spend a good deal of our time ordering, interpreting, and waiting for the results of diagnostic tests. When it comes to determining who needs a test to rule out potentially life-threatening conditions, ED physicians are the experts. There are several reasons for this expertise. First and foremost, we see a lot of patients. Especially for those working in busy hospitals, the expectation is to see everyone in a timely way, provide quality care, and ensure patients have a good experience. If we order time-consuming tests on everyone, ED crowding and efficiency will worsen, costs of care will go up, and patients will experience even longer waits than they already do. In addition, the way ED physicians in the United States are paid may be changing over the coming years through mechanisms such as accountable care organizations and payment bundling. There may be more pressure to carefully choose who needs and who does not need tests in an evidence-based manner.
Differentiating which patients will benefit from further testing in the ED is a complex process. Over the past 30 to 40 years, science and research in diagnostic testing and clinical decision rules in emergency care have advanced considerably. Now, there is a greater understanding of test performance regarding the reliability, sensitivity, specificity, and overall accuracy of tests. Validated clinical decision rules exist to provide objective criteria to help distinguish who does and does not need a test. Serious, potentially life-threatening conditions such as intracranial bleeding and cervical spine (C-spine) fractures can be ruled out based on clinical grounds alone. There are also good risk stratification tools to determine a probability of disease for conditions like pulmonary embolism before any tests are even ordered.
How do we decide who to test and who not to test? There are some patients who obviously need tests, such as the head-injured patient who has altered mental status and who may have a head bleed where the outcome may be dependent upon how quickly the bleeding can be detected with a computed tomography (CT) scan. There are also patients who obviously do not need tests, such as patients with a simple toothache or a mild upper respiratory tract infection. Finally, there is a large group of patients in the middle for whom testing decisions can sometimes be challenging. This group of patients may leave you feeling “on the fence” about testing. In this large middle category, it may not be clear whether to order a test or even how to interpret a test once you have the results. And when we receive unexpected test results, it may not be clear how best to use those results to guide the care of an individual patient.
Let's give some examples of how diagnostic testing can be a challenge in the ED. You are starting your shift and are signed out a patient for whom your colleague has ordered a D-dimer assay (a test for pulmonary embolism). She is 83 years old and developed acute shortness of breath, chest pain, and hypoxia (room air oxygen saturation = 89%). She has a history of a prior pulmonary embolism and her physical examination is unremarkable, except for mild left anterior chest wall tenderness and notably clear lung sounds. The D-dimer comes back negative. Has pulmonary embolism been satisfactorily ruled out? Should you perform a pulmonary angiogram or a CT scan of the chest, or maybe even consider a ventilation–perfusion (V/Q) scan? Was D-dimer the right test for her to begin with?
Let's consider a different scenario. Consider a positive D-dimer assay in a 22-year-old male with atypical chest pain, no risk factors, and normal physical examination including a heart rate of 70 beats per minute and an oxygen saturation of 100% on room air. What do you do then? Should he be anticoagulated and admitted? Does he have a pulmonary embolism? Should you move forward with further confirmatory testing before initiating treatment? Or is he so low risk that he's probably fine anyway? Of course, you might wonder why, if he was so low risk, was the D-dimer ordered in the first place?
As a third example, you are evaluating a 77-year-old female who has fallen down, has acute hip pain, and is unable to ambulate. The hip radiograph is negative. Should you pursue it? Possibly get a CT or magnetic resonance imaging (MRI)? But even though the hip radiograph is negative, will she be able to go home?
These are examples of when test results do not confirm your clinical suspicion. What do you do in those cases? Should you believe the test result or believe your clinical judgment before ordering the test? Were these the optimal tests in the first place? Remember back to conversations with your teachers in emergency medicine on diagnostic testing. Didn't they always ask, “How will a test result change your management?” and “What will you do if it's positive, negative, or indeterminate?”
The purpose of diagnostic testing is to reach a state where we are adequately convinced of the presence or absence of a condition. Test results are interpreted in the context of the prevalence of the suspected disease state: your clinical suspicion of the presence or absence of disease in the individual patient. For example, coronary artery disease is common. However, if we look for coronary disease in 25 year olds, we are not likely to find it because it is very uncommon in that population. There are also times when your clinical suspicion is so high that you do not need objective testing. In certain patients, you can proceed with treatment. For example, some emergency physicians may choose to treat a dislocated shoulder based on the clinical examination rather than first obtaining a radiograph. However, testing is often needed to confirm a diagnosis or to rule out more severe, life-threatening diseases.
The choice over whether to test or not test in the ED also depends upon the resources of the hospital and of the patient. Some hospitals allow easy access to radiographic testing and laboratory testing. In other hospitals, obtaining a diagnostic test may not be as easy. Some hospitals don't have CT scanners. Others do not have the staff available for certain types of tests at night or on weekends (like MRIs and ultrasounds). Sometimes patients may not need a test if you believe that they are reliable to return if symptoms worsen. For others, you may believe that a patient's emergency presentation may be the only time he or she will have access to diagnostic testing. For example, saying to a patient, “Follow up with your doctor this week for a stress test” may be impractical if the patient does not have a primary doctor or does not have good access to medical care. Many providers practice in environments where they cannot order a lot of tests (like developing countries). You also may practice in an office environment that simply does not have easy access to testing. However, regardless of the reason why we order tests in the ED or other acute settings, what is certain is that the use of diagnostic testing in many cases can change how you manage a patient's care.
Sometimes, you may question your choice of whether to test, to not test, or to involve a specialist early. Should you get a CT scan first or just call a surgeon in for a young male with right lower quadrant pain, fever, nausea, and possible appendicitis? How many cases have you seen where the CT scan has changed your management? What if the patient is a young, nonpregnant female? Does that change your plan?
How about using clinical decision rules in practice? By determining if patients meet specific clinical criteria, we can choose not to test some patients if they are low risk. Do all patients with ankle sprains need X-rays? Can you use the Ottawa ankle rules in children? What are the limits of clinical decision rules? Is it possible to apply the Canadian C-spine rules to a 70-year-old female? What is sufficiently “low risk”? These questions come up daily in the practice of emergency medicine. In fact, a major source of variability among physicians is whether or not they order tests. Remember back to your training when you were getting ready to present a patient to the attending physician. Weren't you trying to think to yourself, “What would she do in this case? What tests would she order?”
Access to test results helps us decide whether to treat a disease, initiate even more testing, or no longer worry about a condition. The cognitive psychology of clinical decision making has evolved rapidly over the last several decades. As ED physicians, we gain confidence in this process with experience. Much of the empirical science and mathematics behind testing that are described in this book become instinctive and intuitive the longer you practice emergency medicine. Sometimes we may think a patient does not need to be tested because the last hundred patients who had similar presentations all had negative tests. Maybe you or your colleagues were “burned” once when a subtle clinical presentation of a life-threatening condition was missed (like a subarachnoid hemorrhage). The next patient who presents with those symptoms is probably more likely to get a head CT followed by a lumbar puncture. Is this evidence based? Recognizing our individual diagnostic biases is one way to decrease the likelihood of erroneous decision making while increasing efficiency and effectiveness.
Step back for a moment and think about what we do when ordering a test. After evaluating a patient, we come away with a differential diagnosis of both the most common and the most life-threatening possibilities. The following approach to medical decision making was derived by Pauker and Kassirer in 1980.1 Imagine diagnostic testing as two separate thresholds, each denoted as “I” (for indeterminate). The scale at the bottom of Figure 1.1 denotes pretest probability, which is the probability of the disease in question before any testing is employed. In practice, it is often a challenge to come up with a pretest probability, and frequently opinions on pretest probability differ considerably between experienced physicians. However, for the moment, assume that pretest probability is a known quantity.
Figure 1.1 Pretest probability of disease. (Source: Data from Pauker and Kassirer (1980)).
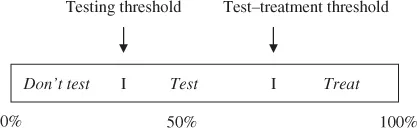
In Figure 1.1, the threshold between “don't test” and “test” is known as the testing threshold. The threshold between “test” and “treat” is known as the test–treatment threshold. In this schema, treatment should be withheld if the pretest probability of disease is smaller than the testing threshold, and no testing should be performed. Treatment should be given without testing if the pretest probability of disease is above the test–treatment threshold. And, when our pretest probability lies between the testing and test–treatment thresholds, the test should be performed and the patients treated according to the test results. That is the theory. But now let's make this more cl...
Table of contents
- Cover
- Website: Evidence-Based Medicine Series
- Title Page
- Copyright
- Dedication
- About the Authors
- Foreword
- Preface
- Acknowledgments
- Section 1: The Science of Diagnostic Testing and Clinical Decision Rules
- Section 2: Trauma
- Section 3: Cardiology
- Section 4: Infectious Disease
- Section 5: Surgical and Abdominal Complaints
- Section 6: Urology
- Section 7: Neurology
- Section 8: Miscellaneous: Hematology, Ophthalmology, Pulmonology, Rheumatology, and Geriatrics
- Index