- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
ABC of Prostate Cancer
About this book
Prostate cancer is the most common cancer in men in the UK and US and the second most common worldwide.
The ABC of Prostate Cancer provides fully illustrated guidance on the treatment and management of prostate cancer. It covers the biology, anatomy, and pathology of prostate cancer, screening, and active surveillance and monitoring. It presents an assessment of treatment options including prostatectomy, bracytherapy, chemotherapy and immunotherapy, along with modern diagnostic tests and an overview of new approaches to prostate cancer.
With an international author team, the ABC of Prostate Cancer is ideal for general practitioners, family physicians, specialist nurses, junior doctors, medical students and others working with prostate cancer patients and their families.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access ABC of Prostate Cancer by Prokar Dasgupta,Roger S. Kirby,Prokar Dasgupta in PDF and/or ePUB format, as well as other popular books in Medicina & Urologia. We have over one million books available in our catalogue for you to explore.
Information
Chapter 1
Applied Anatomy of the Prostate
Overview
- The prostate is composed of four zones: transitional, central, peripheral, and anterior fibromuscular stroma
- The ejaculatory ducts open into the prostatic urethra on either side of the verumontanum
- The external urethral sphincter (both voluntary and involuntary elements) lies immediately distal to the verumontanum while the internal urethral sphincter (involuntary) lies at the bladder neck
- The prostate lies in a hammock of nerves which can be divided into three zones: proximal neurovascular plate, predominant neurovascular bundles, and accessory distal neural pathways Cavernous nerves exceed the posterolateral track and distribute in a more widespread range from anterolateral to posterior of the gland
- The prostate is surrounded by prostatic fascia andendopelvic fascia, with Denonvillier's fascia separating it from the fascia propria of the rectum
The basic anatomy
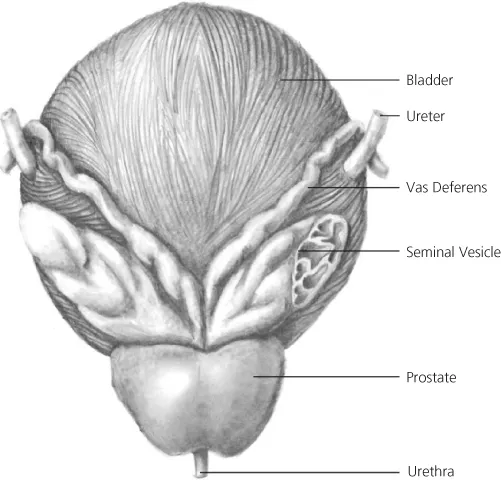
The prostate gland develops after puberty as a result of the testosterone surge. It reaches a size of 20cc in the normal adult, measuring 3 cm in length, 4 cm in width, and 2 cm in depth. Its size and shape can be approximated to that of a walnut. It is located at the base of the bladder, where it surrounds the proximal urethra. In this position, it lies above the urogenital diaphragm between the rectum and the symphysis pubis (Figure 1.1). It is described as having anterior, posterior, and lateral surfaces. Its base is contiguous with the bladder and its apex narrows inferiorly. There is no ‘true’ capsule to the prostate, but rather a ‘false’ capsule of fibromuscular stroma which disappears towards the apex of the gland. The prostate is surrounded by fascial structures (Figure 1.2) anteriorly and anterolaterally by the prostatic fascia, and posteriorly by Denonvillier's fascia which separates it from the fascia propria of the rectum. Laterally, the prostatic fascia merges with the endopelvic fascia (also called the lateral pelvic or levator fascia). The prostatic base is covered with a posterior layer of detrusor apron from the bladder muscle. Abutting the prostate posteriorly are the seminal vesicles and vasa (ducti) deferentia (Figure 1.3).
Figure 1.1 Sagittal section of the male pelvis.
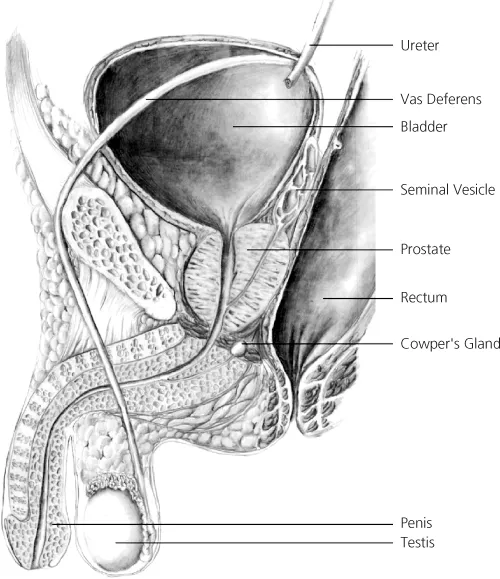
Figure 1.2 Fascial relations of the prostate.
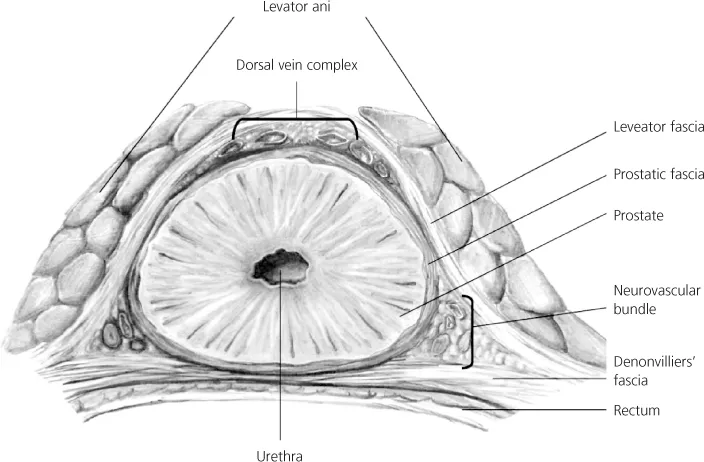
Figure 1.3 The posterior relations of the prostate.
The prostate gland itself is composed of ducts and alveoli that are lined by tall columnar epithelium (70%) within a stroma of fibromuscular tissue (30%). The urethra does not run straight through the middle of the gland as is the common medical student misconception, but rather takes a curved course, running anteriorly as it proceeds from proximal to distal, such that it ends up close to the prostate's anterior surface. It is lined by transitional epithelium throughout most of its length, and squamous epithelium at its distal end, hence, cancer of the urethra is either transitional cell or squamous cell carcinoma, and not adenocarcinoma as for the prostate. Those urothelial cancers are highly aggressive. A urethral crest runs the length of the prostate and disappears in the striated external urethral sphincter (rhabdosphincter). The prostatic sinuses run alongside the crest and all the prostatic glands discharge into this. The small slit of the prostatic utricle is found on the verumontanum (colliculus). The ejaculatory ducts open just lateral to the verumontanum and this is where the seminal vesicle contents are discharged (via the vasa) during emission (Figure 1.4). This allows the seminal fluid to mix with the prostatic secretions such that the final ejaculate is a mixture of these two components.
Figure 1.4 Cross-sectional anatomy of the male lower urinary tract.
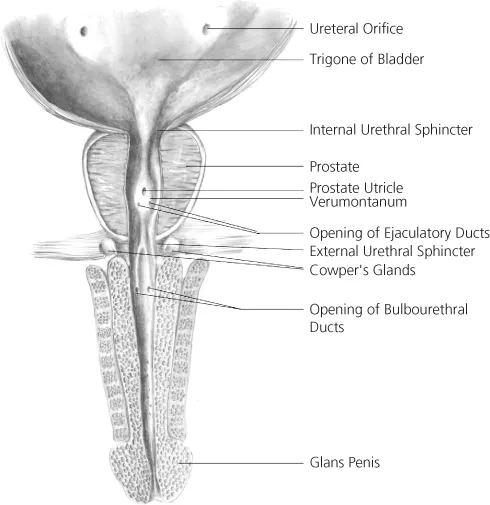
Just proximal to the verumontanum is the external urethral sphincter (EUS) which is a horseshoe-shaped structure which surrounds the prostatic apex craniodorsolaterally, is deficient posteriorly, and has both striated (voluntary) and smooth muscle (involuntary) components. Hence, during a transurethral resection of the prostate (TURP) for benign prostatic enlargement (BPE), the verumontanum serves as the limit for proximal resection so that the EUS is not damaged. The internal urethral sphincter is located at the bladder neck where the prostato-vesical junction is, and is purely under involuntary control (hence, it is composed of smooth muscle). It not only completes the continence mechanism but also makes antegrade ejaculation possible. The internal urethral sphincter is invariably damaged during a TURP so that, were the EUS to also be damaged, then urinary incontinence would be inevitable. This is why the verumontanum (or ‘veru’ to those that know it well) is such an important landmark during TURP.
Lymphovascular supply
The arterial supply to the prostate arises from the inferior vesical artery (itself a branch of the internal iliac artery). As the inferior vesical artery approaches the prostate gland, it becomes the prostatic artery. This then divides into two main groups of arteries: the urethral group and the capsular group. The urethral arteries penetrate the prostato-vesical junction posterolaterally and travel inward, perpendicular to the urethra. They approach the bladder neck in the 1- to-5 o'clock and 7- to-11 o'clock positions, with the largest branches located posteriorly. The capsular artery gives off a few small branches to the false capsule of the prostate, but, in the main, runs posterolaterally to the prostate along with the cavernous nerves (to form the so-called neurovascular bundle), before ending at the urogenital diaphragm.
The venous drainage of the prostate is via the periprostatic plexus of veins to both the dorsal venous complex (of Santorini) superiorly and the inferior vesical vein to the hypogastric vein. These then both drain into the internal iliac vein. The dorsal venous complex (DVC) lies over the anterior aspect of the prostate and is the commonest source of bleeding during a radical prostatectomy. Just lateral to the DVC are the puboprostatic ligaments (PPL) which are condensations of the endopelvic fascia and attach the prostate to the pubic symphysis. The PPL may be important in maintaining continence, and are thus often spared during radical prostatectomy.
As is true of much human anatomy, the lymphatic drainage of the prostate follows that of the veins. Hence, for the prostate, this is to the obturator and hypogastric nodes, and then on to the internal iliac and aortic nodes. It is important to note, however, that prostatic lymphatic drainage is not always predictable in a stepwise manner, and 25% of cases of prostate cancer drain directly to nodes outside the pelvis (internal iliac or higher), making the extent of pelvic lymphadenectomy in high-risk prostate cancer a subject of much debate.
Zonal anatomy
Throughout the nineteenth century, the prostate was described as having two lobes, with each lobe having its own ducts. In 1906, Howe described a middle (or median) lobe. In 1912, Lowsley described five lobes: two lateral lobes, a posterior lobe, the middle lobe, and an atrophied embryological anterior lobe. However, these lobes were visible only in BPE and not the normal prostate. This lobar concept thus left much to be desired, and in 1968, McNeal replaced it with his concentric zones concept (Figure 1.5).
Figure 1.5 McNeal's zones of the prostate.

The transition zone consists of 5–10% of the glandular tissue of the prostate and is responsible for most of the BPE that affects the prostates of older men. The prostatic ducts lead into the junction of the pre-prostatic and prostatic urethra, and travel on the posterolateral aspects of the EUS.
The ducts of the central zone arise circumferentially around the openings of the ejaculatory ducts. These glands are histologically distinct and appear to be Wolffian (mesonephric) in embryological origin. Only 1–2% of prostate cancers arise from this zone.
The peripheral zone makes up 60% of the prostatic volume. Its ducts drain into the prostatic sinus along the entire length. Some 70% of carcinomas arise from this zone which is also commonly affected by prostatitis (hence, prostatitis and cancer can co-exist in men).
The anterior fibromuscular stroma makes up approximately 30% of the gland, and extends from the bladder neck to the EUS anteriorly. It is compressed in BPE and rarely involved in prostate cancer, though anterior cancers should be suspected when repeat conventional prostatic biopsies which do not sample the anterior aspects well come back negative; hence, the use of saturation or template biopsies to sample these anterior aspects.
Neuroanatomy
Using dissections of male fetuses and newborn cadavers, Walsh and Donker first demonstrated the course of the cavernous nerve (the main nerve responsible for erectile function). This led to the concept of the macroscopic neurovascular bundle (NVB) that is located between the endopelvic and prostatic fasciae and runs along the posterolateral aspect of the prostate until it enters the urogenital diaphragm. However, recently, there have been observations that refute the dogma that the cavernous nerve is always within the NVB. Using intraoperative electrical stimulation with simultaneous measurement of intracavernosal pressure, our group, as well as others, discovered that the distribution of cavernous nerves was wider than that of the neurovascular bundle. Our group described the distribution of these nerves and they can be thought of as forming three broad zones: the trizonal concept.
The first zone is the proximal neurovascular plate (PNP) which is...
Table of contents
- Cover
- Series Page
- Title Page
- Copyright
- Contributors
- Foreword
- Chapter 1: Applied Anatomy of the Prostate
- Chapter 2: Pathology of Prostate Cancer
- Chapter 3: Biology of Prostate Cancer
- Chapter 4: Prostate Cancer Diagnosis
- Chapter 5: Imaging of Prostate Cancer
- Chapter 6: Screening for Prostate Cancer
- Chapter 7: Active Surveillance
- Chapter 8: Open Radical Prostatectomy
- Chapter 9: Laparoscopic Radical Prostatectomy
- Chapter 10: Robotic Radical Prostatectomy
- Chapter 11: Prostate Brachytherapy
- Chapter 12: HIFU
- Chapter 13: Cryotherapy for Prostate Cancer
- Chapter 14: Advances in External Beam Radiotherapy
- Chapter 15: Recent Advances in Hormonal Therapy
- Chapter 16: Management of Castration-Resistant Prostate Cancer
- Chapter 17: Immunology of Prostate Cancer
- Chapter 18: New Approaches to Prostate Cancer
- Index
- Advertisement