- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
ABC of Medically Unexplained Symptoms
About this book
This brand new title addresses the complex issues faced by primary health care practitioners in treating and managing patients with 'medically unexplained symptoms'. It aims to develop guidelines and principles to help identify patients with medically unexplained symptoms, as they are typically underdiagnosed, and to manage symptoms more effectively with active patient involvement.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access ABC of Medically Unexplained Symptoms by Christopher Burton in PDF and/or ePUB format, as well as other popular books in Medicina & Medicina interna e diagnosi. We have over one million books available in our catalogue for you to explore.
Information
Chapter 1
Introduction
OVERVIEW
- Medically unexplained symptoms (MUS) are characterised by disturbances of function—including physiological, neurological and cognitive processes
- Using what is currently known about disturbed function, it is possible to develop coherent and plausible models of conditions in order to explain what is going on to patients
- Sharing explanations and understanding concerns allows the doctor and patient to work together. Describing symptoms as disorders of function is an acceptable way of doing this
Aim
This book aims to help general practitioners (GPs) and other generalists to understand and treat conditions associated with symptoms that appear not to be caused by physical disease. This lack of explanation due to visible pathology means they are often called medically unexplained symptoms (MUS). This book takes the view that MUS are disorders of function, rather than structure, and so the book will refer to them as functional symptoms. Although we do not fully understand the nature of the disturbed function, research is making this clearer and several mechanisms, including physiological, neurological and cognitive processes play a part in symptoms. This book also takes the view that by using what is currently known about functional symptoms, it is possible to develop coherent and plausible models to explain what is going on. This book aims to help doctors explain the medically unexplained—both to themselves and to their patients.
Symptoms that appear not to be caused by physical disease are a challenge to doctors and patients. Both have to simultaneously consider the possibility of serious illness (either physical or mental) while seeking to contain and reduce the symptoms and the threat they represent. This is not easy. In order to deal with MUS, and the patients who present with them, doctors need to apply a range of clinical skills: from empathic history taking and focused examination, through careful assessment of probabilities, to communication, explanation and—sometimes—support. This book assumes you already have those skills to some extent; it aims to show ways of using, and developing, them in order to deal with these common problems.
An approach to MUS
The ABC of Medically Unexplained Symptoms is not a book about the somatisation of mental distress from a psychoanalytic perspective. It does not take the view that unexplained symptoms are a way of communicating need in people who cannot otherwise do so. Rather it takes a mechanistic view of symptoms as the result of interacting processes—some physiological, some neuropsychological—that lead to persistent unpleasant feelings and distress. This approach is similar to that used in pain medicine, with which it has much in common; indeed many unexplained symptoms and syndromes include pain.
This introductory chapter addresses three questions: what do we mean by medically unexplained symptoms; what causes medically unexplained symptoms; and what should we call medically unexplained symptoms?
What do we mean by medically unexplained symptoms?
The simple answer to this question is ‘physical symptoms that cannot be explained by disease’, but it has several problems. First, this book is written largely from a primary care perspective and although it may be that every possible disease has been ruled out in tertiary care, this is not often the case in primary care. Furthermore, not all ‘diseases’ have consistent pathology—migraine is an excellent example of a syndrome that we have kept on the ‘explained’ side of the dividing line between explained and medically unexplained symptoms but where the problem is one of disturbed function rather than structure. Even persistent back pain, which initially seems an obvious ‘explained’ symptom, shows almost no correlation between symptom severity and structural abnormality.
Instead of this simple ‘absence of disease’ answer, it can be helpful to think of three different meanings: symptoms with low probability of disease; functional somatic syndromes; and experiencing multiple physical symptoms. This book will use the adjective ‘functional’ in relation to symptoms or syndromes (i.e. MUS) to mean simply that we can best understand them in terms of disturbed function without altered structure. In general it will use the term ‘organic’ to refer to conditions associated with pathological change.
Symptoms with low probability of disease
This term has recently been introduced in an attempt to capture the uncertainty that is inherent in this field. Around 10% of patients in primary care with persistent so-called MUS eventually turn out to have an alternative diagnosis. The proportion is rather lower in some forms of secondary care but nonetheless all doctors will have seen a patient whom they originally thought had a functional symptom but turned out to have a disease. We believe that the concept of symptoms with low probability of disease is useful though, as it can be applied to a patient with positive pointers to a functional disorder and with no red flags for serious illness to indicate a ‘working diagnosis’. Chapters 3 and 4 describe the recognition of physical illness and emotional disorders in patients with MUS.
Functional somatic syndromes
The common functional physical symptoms—fatigue, headache, light-headedness, headache, palpitations, chest pain, nausea, bloating, abdominal pain, musculoskeletal pain and weakness often occur together. Some of these clusters—particularly when they present to a given clinical specialty—are commonly grouped together as a syndrome. So gastroenterology has the irritable bowel syndrome (IBS), rheumatology has chronic widespread pain and fibromyalgia, and gynaecologists have chronic pelvic pain. As Figure 1.1 shows, and as described further in Chapter 2, all these symptoms overlap; to the extent that some experts argue that all the syndromes represent facets of a single disorder.
Figure 1.1 Overlap of medically unexplained symptoms.
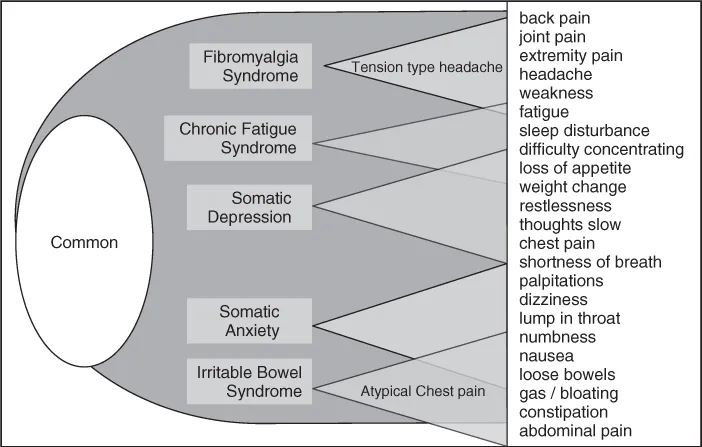
In practical terms, however, the syndrome labels are here to stay and they often represent useful diagnostic labels or categories. The common syndromes are covered in this book, and when we use the term ‘MUS’, it includes these defined syndromes as well as less clearly categorised symptoms.
Experiencing multiple physical symptoms
As Chapter 2 describes, everyone has some functional symptoms at some point in their life. What matters is that some patients have multiple physical symptoms that cause distress and that have an impact in terms of restricting behaviour or seeking medical attention. This triad of multiple symptoms, distress and impact has received various names including somatisation (but it then gets confused with the psychoanalytic concept) and most recently a proposed new term ‘bodily distress disorder’. At the moment there is no widely acceptable name for this phenomenon, but the triad of multiple symptoms (Box 1.1), distress and impact seems to describe an important group of patients well.
Box 1.1 The triad of experiencing multiple symptoms
- Experiencing multiple symptoms
- Distress because of symptoms
- Impact on activities or healthcare seeking because of symptoms
What causes MUS?
The simple answer is ‘we don,'t know’—because otherwise they wouldn't be medically unexplained symptoms. But actually we know quite a bit about the factors that predispose patients to MUS, the mechanisms that give rise to symptoms; the cognitive processes by which they are appraised and the processes that perpetuate them.
Predisposing factors
If you have the good fortune to have been born with the right genes, brought up in an emotionally secure family, protected from poverty, illness and abuse, and have a fulfilling role in life then your chances of problems with MUS (and most other conditions) are reduced. However for most people it is difficult to argue that one factor is more important than another. Depression and anxiety undoubtedly predispose to future MUS, and conversely MUS predispose to future depression and anxiety.
Biological mechanisms
Given that there is no obvious disorder of structure, it is reasonable—and acceptable—to talk of MUS as disorders of function and you will find this sort of language in several of the chapters. As well as more obvious changes of function such as gut motility or heart rate, subtle changes in autonomic function are common in patients with MUS. Some form of hypothalamic–pituitary axis dysfunction appears to be present in many patients with fatigue and chronic pain and there is mounting evidence for the effect of stress on immune regulation.
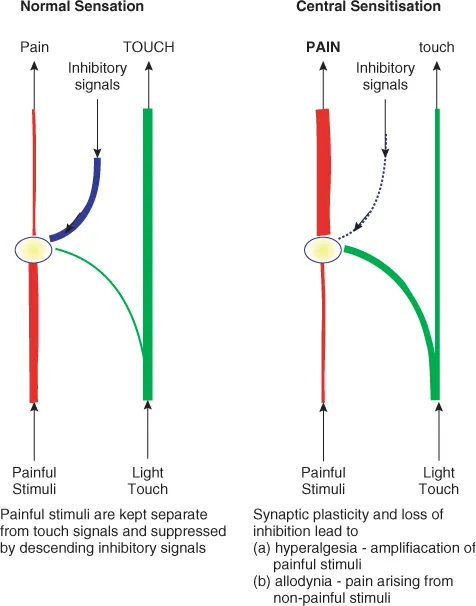
Central sensitisation to pain is an increasingly recognised and understood process in all forms of chronic pain (whether ‘explained’ or not). It is characterised by heightened perception of, and distress from, a range of sensory inputs and includes the two components hyperalgesia (heightened perception of painful stimuli) and allodynia (pain arising from non-painful stimuli) illustrated in Figure 1.2. Neuroimaging is beginning to highlight characteristic areas of under- and overactivity as symptoms are processed in the brain. This is an active field of research and it seems inevitable that new physical mechanisms will be uncovered with time.
Figure 1.2 Sensory pathways in normal sensation and central sensitisation.
Symptom awareness and appraisal
It is important to recognise that symptoms feel the same to the patient, whether they are ‘explained’ or ‘medically unexplained’. This is important to convey to patients who sometimes think that if no physical cause can be found then the doctor thinks they are imagining it—and that, somehow, functional symptoms would feel different.
The same centres in the brain are activated regardless of the origin of pain and detailed studies of the experience of symptoms show that distress from and response to symptoms follow similar patterns, regardless of cause. The experience of symptoms ...
Table of contents
- Cover
- Series Page
- Title Page
- Copyright
- Contributors
- Acknowledgements
- Chapter 1: Introduction
- Chapter 2: Epidemiology and Impact in Primary and Secondary Care
- Chapter 3: Considering Organic Disease
- Chapter 4: Considering Depression and Anxiety
- Chapter 5: Medically Unexplained Symptoms and the General Practitioner
- Chapter 6: Principles of Assessment and Treatment
- Chapter 7: Palpitations, Chest Pain and Breathlessness
- Chapter 8: Headache
- Chapter 9: Gastrointestinal Symptoms: Functional Dyspepsia and Irritable Bowel Syndrome
- Chapter 10: Pelvic and Reproductive System Symptoms
- Chapter 11: Widespread Musculoskeletal Pain
- Chapter 12: Fatigue
- Chapter 13: Neurological Symptoms: Weakness, Blackouts and Dizziness
- Chapter 14: Managing Medically Unexplained Symptoms in The Consultation
- Chapter 15: Cognitive Approaches to Treatment
- Chapter 16: Behavioural Approaches to Treatment
- Chapter 17: Pharmacological Treatment
- Chapter 18: Conclusion
- Appendix: Suggestions for Reflection and Audit
- Index