![]()
1
Mechanics of the Cardiovascular System
B. Greaney & A.M. Kucia
Overview
The cardiovascular system consists of two primary components: the heart and blood vessels. The lymphatic system also has a cardiovascular exchange function but does not contain blood. This chapter will highlight the mechanics of the cardiovascular system and present an overview of the essential elements and structures involved in the flow of blood through the venous and arterial systems. It will also highlight how abnormalities in the mechanics of the cardiovascular system can result in degrees of cardiac disease states.
Learning objectives
After reading this chapter, you should be able to:
- Identify the anatomical location of the heart and its basic function.
- Identify the key structures within the heart, which are involved in the flow of blood through the heart and identify their specific function.
- Define the term ‘cardiac cycle’ and explain the key physiological changes that occur in the heart during this process.
- Define the terms ‘cardiac output’ (CO) and ‘stroke volume’ (SV), and explain their physiological significance in relation to the cardiac cycle.
- Define the terms ‘preload’, ‘afterload’ and ‘contractility’, and explain their physiological impact upon myocardial contraction.
Key concepts
Cardiac cycle; cardiac output; cardiac chambers; cardiac valves; layers of the heart
Basic heart anatomy
The human heart is essentially a muscular pump which delivers blood containing oxygen, nutrients and other vital elements to the body tissues and major organs. The structure and location of the heart was described by Henry Gray in 1918. It is conical in shape, about the size of a human fist and weighs between 230 and 340 g in an adult. The heart is located in the mediastinum, with one-third lying to the right of the sternum and two-thirds to the left. The top of the heart is known as the base, and this is located behind the sternum; the bottom of the heart, known as the apex, is located in the fifth intercostal space in the mid-clavicular line. The heart is a four-chambered structure – the upper chambers known as the right and left atria, the lower two chambers known as the right and left ventricles, with right and left-sided chambers divided by the septum.
The bulk of the heart’s wall is the myocardium, which is a thick contractile mass of cardiac muscle cells. It is the myocardium that provides the force of contraction to move blood out of the ventricles at the end of each cardiac cycle. The heart is surrounded by the pericardium, which is comprised of two principal layers that surround and protect the heart. The outer layer is known as the fibrous pericardium, which is made up of tough and fibrous connective tissue. This layer provides both protection and anchorage for the heart. The second layer, the serous pericardium, is a thinner, more delicate layer and forms two distinct layers around the heart. The outer parietal layer is adhered to the inner side of the fibrous pericardium, whilst the inner visceral layer, also known as the epicardium, is adhered tightly to the myocardium. Between these two layers there exists a potential space termed the pericardial cavity. Within this cavity is a very thin film of serous fluid known as pericardial fluid, which is normally between 15 and 35 mL in volume (Spodick 1997). The key function of this fluid is to reduce friction between the pericardial layers as the heart contracts. The inner layer lining the heart is a continuous sheet of squamous epithelium, continuing into the tunica intima of blood vessels, and is known as the endocardium.
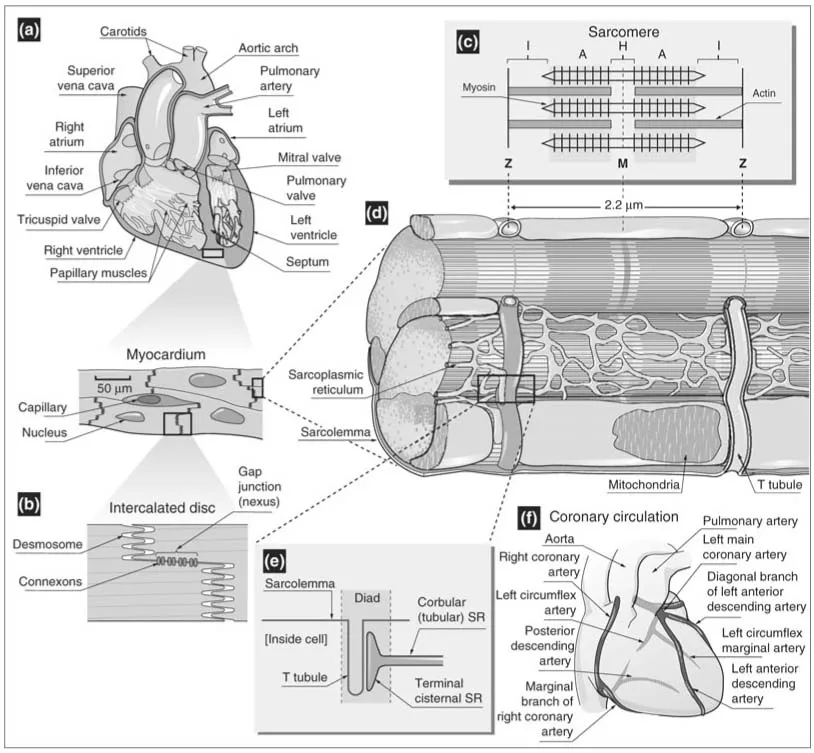
The heart is divided into four chambers: two upper atria and two lower ventricles. These chambers are separated by a set of heart valves termed the atrioventricular (AV) valves; the tri-cuspid valve separates the right atrium (RA) and right ventricle (RV) and the bicuspid valve or mitral valve separates the left atrium (LA) and left ventricle (LV) (Figure 1.1a). Attached to each AV valve are two structures: the chordae tendinae and the papillary muscles. These two structures are adhered to the walls of each ventricle (Figure 1.1a). Their function is to prevent the valve cusps inverting or swinging upward into the atria during ventricular systole. The key function of the heart valves is to permit the flow of blood in one direction only as it flows through the heart.
The heart can be viewed functionally as two pumps serving the pulmonary and systemic circulations. The pulmonary circulation refers to the flow of blood within the lungs that is involved in the exchange of gases between the blood and the alveoli. Deoxygenated blood returns to the RA via the inferior and superior vena cavae. It then passes through the tricuspid valve to the RV before entering the pulmonary circulation via the pulmonary artery, where gases are exchanged. The pulmonary artery has a pulmonary valve or semi-lunar valve which opens and closes during contraction and relaxation of the heart, again having a similar function to the AV valves, allowing the flow of blood in one direction only (Figure 1.1). The systemic circulation consists of all the blood vessels within and outside of all organs excluding the lungs. Once oxygenated, the blood returns to the LA via the pulmonary veins and then passes through the mitral valve into the thicker-walled left ventricle, which ejects the oxygenated blood through the aortic valve into the aorta and into the systemic circulation. The aorta also has a valve, the aortic valve, which prevents the back-flow of blood during myocardial contraction (Figure 1.1a).
The cardiac cycle
In simple terms, the heart is a pump that receives blood from the venous system at low pressure and generates pressure through contraction to eject the blood into the arterial system. The mechanical action of the heart is created by a synchronised contraction and relaxation of the cardiac muscle, referred to as systole and diastole. The actual mechanical function of the heart is influenced by pressure, volume and flow changes that occur within the heart during one single cardiac cycle.
When the heart muscle contracts (systole) and relaxes (diastole), sequential changes in pressure are produced in the heart chambers and blood vessels, which result in blood flowing from areas of high pressure to areas of lower pressure. The valves prevent backflow of blood. Under normal conditions, this cycle will take place in the human heart between 60 and 100 times per minute.
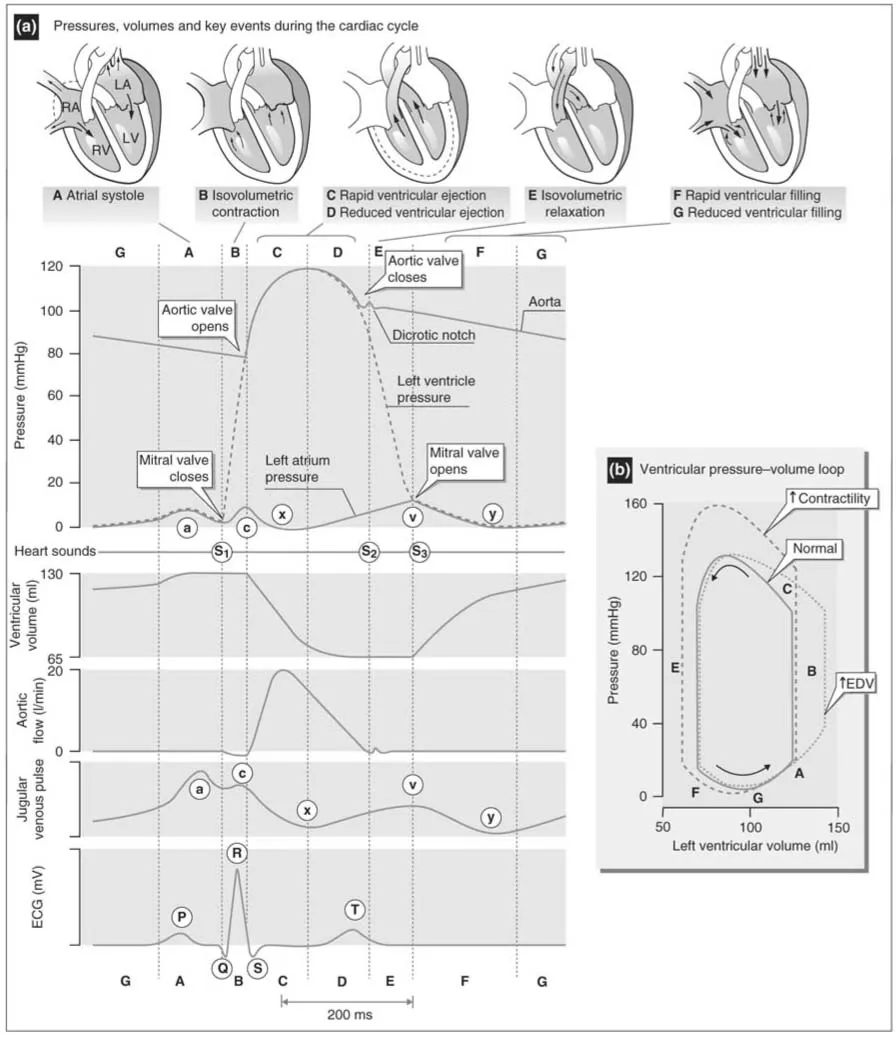
Figure 1.2a demonstrates the seven phases of the cardiac cycle.
Figure 1.1 Gross anatomy of the heart.
Source: From Aaronson and Ward (2007).
Phase 1: Atrial systole
Atrial systole begins after a wave of depolarisation passes over the atrial muscle. Atrial depolarisation is represented by the P wave on the electrocardiograph (ECG). As the atria contract, pressure builds up inside the atria forcing blood through the tricuspid and mitral valves into the ventricles. Atrial contraction causes a small increase in proximal venous pressure (in the pulmonary veins and vena cavae). This is represented by the ‘a’ wave of the jugular venous pulse, which is used to measure jugular venous pressure (JVP) (Klabunde 2005).
- Blood flows from the RA across the tricuspid valve into the RV.
- Blood flows from the LA through the mitral valve into the LV.
Pressure in the atria falls and the AV valves float upward. Ventricular volumes are now at their maximum (around 120mL) and this is known as end diastolic volume (EDV). Left ventricular end diastolic pressure (LVEDP) is approximately 8–12 mmHg; right ventricular end diastolic pressure (RVEDP) is usually around 3–6 mmHg. A fourth heart sound (S4) may be heard in this phase if ventricular compliance is reduced, such as happens with ventricular hypertrophy, ischae-mia or as a common finding in older individuals.
Figure 1.2 Cardiac cycle.
Source: From Aaronson and Ward (2007).
Key point
Ventricular filling occurs passively before the atria contract and depends upon venous return. Atrial contraction normally accounts for only around 10% of ventricular filling, when the body is at rest. However, at high heart rates (such as during exercise), there is a shortened period of diastole where passive filling normally occurs. Under these conditions, atrial contraction is more important and can contribute up to 40% of ventricular filling. Enhanced ventricular filling due to atrial contraction is sometimes referred to as the ‘atrial kick’ (Klabunde 2005).
Phase 2: Isovolumetric contraction
This phase is represented by the QRS complex on the ECG. The ventricle depolarises and initiates contraction of the myocytes, resulting in a rapid increase in ventricular pressure. This rise in pressure causes the AV valves to close. Closure of the AV valves generates the first heart sound (S1). A split S1 may be heard as mitral valve closure precedes tricuspid valve closure by around 0.04 of a second, although usually only one sound can be heard through a stethoscope. The time between closure of the AV valves and opening of the semilunar valves is known as isovolumetric contraction because there is no change in the volume of blood in the ventricle at this stage, although the ventricle contracts and becomes more spheroid in shape. The pressure in the LV becomes maximal at this stage and is termed dp/dt (maximal slope of the ventricular pressure tracing/time) (Klabunde 2005).
Phase 3: Rapid ventricular ejection
When the ventricular pressure exceeds that of the aorta (around 80 mmHg) and pulmonary arteries (around 10 mmHg) the aortic and pulmonary valves open and blood is ejected out of the ventricles. The LV has a thick muscular wall that allows it to generate high pressures during ventricular contraction. Maximal outflow velocity occurs early in the ejection phase, so the highest aortic and pulmonary artery pressures are reached at this time (Klabunde 2005).
- Blood is ejected from the RV across the pulmonic valve and into the pulmonary artery to the pulmonary circulation.
- Blood is ejected from the LV across the aortic valve and into the aorta to the systemic circulation.
Between 70 and 90 mL of blood is ejected with each stroke (stroke volume), but about 50 mL remains in each ventricle. The residual amount of blood left in the ventricle is known as the endsystolic volume (ESV). Stroke volume thus is the difference between EDV and ESV. Around 60% of the total volume of the ventricle is ejected in each cycle. To work out the ejection fraction of the ventricle, divide the stroke volume by the EDV. The normal left ventricular ejection fraction (LVEF) is above 55% (Klabunde 2005).
Key point
In the healthy heart, no heart sounds should be heard during the ejection phase of the cardiac cycle. The presence of sounds during ejection indicates valvular disease or intracardiac shunts (Klabunde 2005).
Phase 4: Reduced ventricular ejection
The ventricle relaxes and the rate of ejection begins to fall, although kinetic or inertial energy continues to propel the blood forward into the aorta. This phase coincides with ventricular repolarisation, which occurs approximately 150–200 ms after the QRS complex and appears as the T wave on the ECG. Atrial pressure starts to rise during this phase due to venous return (Klabunde 2005).
- The RA receives blood from the systemic circulation via the inferior and superior vena cavae at a low pressure (approximately 0–4 mmHg).
- After circulating through the lungs, blood returns to the heart via the four pulmonary veins into the LA. The pressure in the LA is usually between 8–12 mmHg.
Phase 5: Isovolumetric relaxation
In this phase, the pressure in the ventricles continues to fall and when the point is reached where the pressure is less in the ventricles than that in the outflow tracts (aorta and pulmonary veins), the aortic and pulmonary valves close abruptly, causing a second heart sound (S2). Aortic and pulmonary artery pressures fall slowly due to a combination of stored energy in the elastic walls of these vessels which controls pressure and flow, and because forward flow is impeded by systemic and pulmonic vascular resistance as blood is distributed through the systemic and pulmonary circulations (Klabunde 2005).
Key point
As the aortic valve closes before the pulmonic valve, there is a physiological splitting of the S2 sound and this may be heard with a stethoscope. Closure of the aortic and pulmonary valves result in a characteristic notch in aortic and pulmonary artery pressure tracings (Figure 1.2a). The aortic notch is important in setting timing for intra-aortic balloon counterpulsation.
Phase 6: Rapid ventricular filling
Low pressures in the heart allow blood to passively return to the atria. When the ventricular pressure falls below the atrial pressure, the AV valves open and the ventricles fill quickly. Blood flows into the atria and ventricles throughout diastole with the rate of filling decreasing as the amount of blood in the chambers distends the walls. About 70% of ventricular filling occurs passively at this time.
Key point
No prominent heart sounds should be heard at this time. If a third heart sound (S3) is heard during ventricular filling in adults, it may indicate tensing of the chordae tendinae and AV ring, often associated with ventricular dilation. It is a normal finding in children.
Phase 7: Rapid ventricular filling
There is no clear demarcation as to when this phase begins, but this is a stage during diastole when passive ventricular filling is near completion. As the ventricles fill, they become less compliant, causing intraventricular pressure to rise and the rate of ventricular filling starts to fall. Immediately following this phase, atrial systole occurs following firing of the sino-atrial node.
Key point
At slow heart rates, diastole is lengthened, resulting in increased filling time. In rapid heart rates, there is less filling time. This would compromise CO, if not for compensatory mechanisms.
Cardiac output
CO is an important index of cardiac function, and refers to the amount of blood that is ejected with each contraction (stroke volume) multiplied by heart rate (HR):
At typical resting values, if the heart rate is 75 beats/min and the stroke volume is 70 mL/beat, the CO should equal 5.25 L/min. Therefore the body’s total volume of blood (4–6 L/min) passes through the body each minute (Saladin 2001).
CO never remains at a constant rate: any factor that alters stroke volume or heart rate will alter CO and it can vary significantly according to normal physical exercise as well as impaired cardiac function. Other factors such as preload, afterload and contractility (inotropy) will indirectly affect CO.
Preload is defined as the actual stretch or tension on the ventricular myocardium prior to contraction (Totora & Gabowski 2002). The greater the preload on the myocardium (the larger the amount of blood that has filled the heart during diastole), the greater the contraction will be. A simple analogy to explain this concept is that the further you stretch an elastic band prior to releasing it, the further it will recoil. The same principle applies here: the greater the stretch or tension on the myocardium, the greater the force of contraction. When venous return to the heart increases, ventricular filling and preload also increase. The Frank Starling Law of the Heart (Starling’s Law) asserts that the more the ventricle is filled with blood during diastole (EDV), the greater the volume of blood that will be ejected (stroke volume) during the ensuing systolic contraction. Thus, altered preload is a mechanism by which the force of contractility can be affected (Klabunde 2005).
Contractility, also known as inotropy, is the ability of a cardiac myocyte to alter its tension development independently of preload changes (Klabunde 2005). Contractility is affected by autonomic innervation and circulating catecholamines (adrenaline, noradrenaline), and additionally changes in afterload and heart rate can augment contractility. A number of pharmacological agents positively or negatively affect contractility. Agents that affect contractility are called positive or negative inotropes, depending upon whether they increase or decrease contractility. Loss of myocardial contractility results in heart failure.
Afterload is defined as the force or pressure against which the ventricular myocardium must push prior to contraction (Totora & Grabowski 2003). This force or pressure is constantly present in the arteries as arterial blood pressure. Therefore, any increase in systemic blood pressure will result in the left ventricular myocardium having to contract more forcefully to eject its volume of blood. Any increase in t...