- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
New Mechanisms in Glucose Control
About this book
New Mechanisms in Glucose Control presents a clear overview of the new drugs and treatment therapies that have been developed in recent years to help improve glycaemic management for the diabetic patient, namely the incretin mimetics (GLP-1 agonists) and DPP-4 inhibitors. It also considers other drug classes currently in development and undergoing clinical trials including the SGLT2 inhibitors and other pipeline products. In addition to pharma cotherapeutic agents, the role of bariatric as a management tool for diabetes is covered as well as consideration of the organisation of diabetes care with a community focus.
This indispensable pocketbook details the newer treatments and offers a comparison with more traditional agents including sulphonyureas, glitazones and insulin. The pros and cons of traditional therapies are discussed as well as the epidemiology and pathogenesis of type 2 diabetes, helping to give the reader a better understanding of the disease area and its management.
New Mechanisms in Glucose Control is essential reading for health professionals working in primary or secondary care and involved in treating diabetic patients.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access New Mechanisms in Glucose Control by Anthony H. Barnett,Jenny Grice in PDF and/or ePUB format, as well as other popular books in Medicine & Endocrinology & Metabolism. We have over one million books available in our catalogue for you to explore.
Information
CHAPTER 1
Epidemiology and Pathogenesis of Type 2 Diabetes
Throughout the world the increasing prevalence of diabetes is posing significant strains on already overburdened healthcare systems. Type 2 diabetes accounts for most of the projected increase, which reflects not only population growth and the demographics of an aging population, but also the increasing numbers of overweight and obese people who are at increased risk of diabetes.
The current prevalence of diabetes
Latest estimates from the International Diabetes Federation indicate that in 2010 the global prevalence of diabetes will be 285 million, representing 6.4% of the world’s adult population, with a prediction that by 2030 the number of people with diabetes will have risen to 438 million (IDF, 2009).
In Europe, there is a wide variation in prevalence by country, but the total number of adults with diabetes in the region is expected to reach 55.2 million in 2010, accounting for 8.5% of the adult population (IDF, 2009). Estimates indicate that at least € 78 billion will be spent on healthcare for diabetes in the European Region in 2010, accounting for 28% of global expenditure (IDF, 2009).
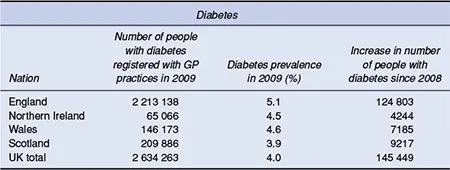
In the United Kingdom (UK), there are now more than 2.6 million people with diabetes registered with general practices and more than 5.2 million registered as obese (Tables 1.1 and 1.2) (Diabetes UK, 2009). A recent analysis of UK data from The Health Improvement Network (THIN) database has shown a sharp jump in diabetes prevalence (Massó-González et al., 2009). The study used data on 49 999 prevalent cases and 42 642 incident cases (1256 type 1 diabetes, 41 386 type 2 diabetes) of diabetes in UK patients aged 10 to 79 years in the THIN database. From 1996 to 2005, prevalence increased from 2.8% to 4.3%, while the incidence rose from 2.71 per 1000 person-years to 4.42 per 1000 person-years. The study also found that the proportion of patients newly diagnosed with type 2 diabetes who were obese increased from 46% to 56% during the decade, further highlighting the important role that obesity plays in the type 2 diabetes epidemic.
Table 1.1 Prevalence of diabetes in people registered in UK general practice
Source: Diabetes UK (2009). Reproduced with permission.
In the United States (US), recent predictions, which account for trends in risk factors such as obesity, the natural history of diabetes and the effects of treatments, suggest that the number of people with diagnosed and undiagnosed diabetes will double in the next 25 years from 23.7 million in 2009 to 44.1 million in 2034 (Huang et al., 2009). Furthermore, the researchers predict that even if the prevalence of obesity remains stable, diabetes spending over the same period will nearly triple to US$336 billion.
Factors driving the type 2 diabetes epidemic
Age
The prevalence of type 2 diabetes increases with age and with more people living well into old age the likelihood of developing the disease is increased. However, increases in prevalence have been observed in younger age groups in association with the rising prevalence of childhood obesity and physical inactivity (Ehtisham, Barrett and Shaw, 2000; Fagot-Campagna, 2000). This is a worrying finding given that the risk of complications increases with duration of disease.
Table 1.2 Prevalence of obesity in people registered in UK general practice
Source: Diabetes UK (2009). Reproduced with permission.
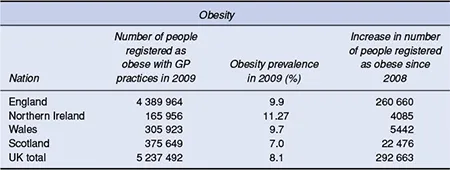
Figure 1.1 The growing epidemic of type 2 diabetes in relation to obesity (Mokdad et al., 2000). Data from Diabetes Care 2000; 23:1278–1283, Copyright 2000 American Diabetes Association.
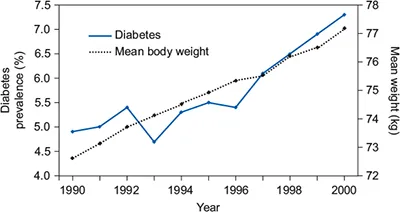
Overweight and obesity
More and more of the world’s population is being exposed to the dietary habits and sedentary lifestyles of the developed nations. The increase in calorie intake, mainly derived from carbohydrates and animal fat, with a decrease in physical activity, has led to excessive obesity and increasing resistance to insulin action. Type 2 diabetes is strongly associated with overweight and obesity (Figure 1.1) (Mokdad et al., 2000), and a high proportion of people with type 2 diabetes are overweight or obese at the time of diagnosis, which may reach up to 80% in some populations (Hedley et al., 2004).
In the UK, rates of obesity have dramatically increased in the past two decades. The ongoing Health Survey for England highlights the increasing trend. In 1993, 13% of men and 16% of women were estimated to be obese (body mass index (BMI) >30 kg/m2) (DoH, 1994). Just over a decade later the proportion of men and women classed as obese had increased to 24% for both sexes (DoH, 2004). The Foresight report ‘Tackling Obesities: Future Choices’, which was commissioned by the UK Government, has estimated that if no action is taken, 60% of men, 50% of women and 25% of under-20 year olds will be obese by 2050 based on current trends (Foresight, 2007).
Socioeconomic class
The prevalence of diabetes appears to be higher amongst low socioeconomic groups, with a 36% higher prevalence noted amongst men living in the most deprived areas of England and Wales compared with those living in the most affluent areas. For women the prevalence amongst those living in the most deprived areas is 80% higher than amongst those living in the least deprived parts. Interestingly, the reverse situation is found in developing countries (Mohan et al., 2001).The tendency for the increased prevalence of type 2 diabetes to be concentrated in lower socioeconomic groups in developed countries and higher socioeconomic groups in developing countries probably reflects the adoption of a healthier lifestyle by better educated people in developed countries, while it is generally the affluent in developing countries who enjoy a high calorie intake and low level of physical activity.
Ethnicity
Certain ethnic minorities (e.g. individuals originating from the Indian sub-continent, Pima Indians, Mexican Americans, and African Americans) appear to have an increased susceptibility to develop insulin resistance when meeting certain environmental factors including obesity and a sedentary lifestyle and are more prone to type 2 diabetes than Caucasians (Barnett et al., 2006). These populations may have an increased genetic susceptibility to lay down intra-abdominal fat, particularly when encountering a Western style of living.
In the UK, the risk of type 2 diabetes is increased four- to sixfold in South Asians compared with Caucasians (Barnett et al., 2006). The age at presentation is also significantly younger (UKPDS, 1994). As duration of diabetes is one of the strongest risk factors for complications, this places this population at particular risk.
Pathogenesis of type 2 diabetes
Type 2 diabetes is characterized by three main defects: peripheral insulin resistance (decreased glucose uptake in muscle, fat and the liver), excess hepatic glucose output, and a pancreatic beta-cell insulin-secretory deficit. The development of the condition is a gradual process, however, and in most individuals, insulin resistance is the first defect to occur (Haffner et al., 2000). Both genetic and environmental factors play a role in the pathogenesis of type 2 diabetes, but one of the most common causes of insulin resistance is obesity, particularly abdominal obesity.
Insulin resistance precedes abnormalities in insulin secretion by several years because pancreatic beta cells are initially able to compensate for insulin resistance by increasing insulin secretion sufficiently to maintain normal blood glucose levels. Eventually, the beta cells become exhausted, however, and can no longer produce enough insulin.
Following a meal, insulin is produced in two phases. First-phase insulin secretion is released rapidly after a meal, and it is this response that is lost very early in type 2 diabetes. When the first-phase insulin response fails, plasma glucose levels rise sharply after a meal producing postprandial hyperglycaemia. Initially, this precipitates an increased stimulation of second-phase insulin release, but eventually this too will be blunted and fasting hyperglycaemia will also result.
The results of the United Kingdom Prospective Diabetes Study (UKPDS) demonstrated that beta-cell function is already reduced at the time of diagnosis of type 2 diabetes and continues to deteriorate despite treatment (UKPDS 33, 1998). The mechanisms responsible for the progressive loss of beta-cell function are still unclear, although a number of hypotheses exist. Some data suggest that genetic abnormalities may result in increased apoptosis and decreased regeneration of beta cells. Over-stimulation of the beta cells in the early years of insulin resistance may lead to increased rates of beta-cell death. Another possibility is that prolonged hyperglycaemia could lead to beta-cell loss or dysfunction through glucotoxicity (Kaiser, Leibowitz and Nesher, 2003) or lipotoxicity mechanisms (Smiley, 2003).
In the past decade, research on the incretin hormones has increased our understanding of the pathogenesis of type 2 diabetes. The predominant incretin hormone is glucagon-like peptide-1 (GLP-1), which has a number of functions including: stimulation of glucose-dependent insulin secretion, suppression of glucagon secretion, slowing of gastric emptying, reduction of food intake, and improved insulin sensitivity. Secretion of GLP-1 is lower than normal in patients with type 2 diabetes (Vilsbøll et al., 2001), and increasing GLP-1 decreases hyperglycaemia, which suggests that the hormone may contribute to the pathogenesis of the disease (Drucker, 2003). As a result of research in this area, most new treatments for type 2 diabetes are being designed based on an understanding of the full pathophysiology of diabetes targeting all major defects.
References
Barnett AH, Dixon AN, Bellary S, et al. (2006) Type 2 diabetes and cardiovascular risk in the UK South Asian community. Diabetologia; 49:2234–2246.
Department of Health (DoH). Health Survey for England 1994: cardiovascular disease and associated risk factors. Available from: http://www.dh.gov.uk/en/Publicationsandstatistics/PublishedSurvey/HealthSurveyForEngland/Healthsurveyresults/DH_4001552. Last accessed February 2010.
Department of Health (DoH). Health Survey for England 2004: Health of ethnic minorities. Available from: http://www.ic.nhs.uk/statistics-and-data-collections/health-and-lifestyles-related-surveys/health-survey-for-england/health-survey-for-england-2004:-health-of-ethnic-minorities-full-report. Last accessed February 2010.
Diabetes UK [News release, 2 October 2009]. Diabetes and obesity rates soar. Available from: http://www.diabetes.org.uk/About_us/News_Landing_Page/Diabetes-and-obesity-rates-soar. Last accessed February 2010.
Drucker DJ. (2003) Glucagon-like peptides: regulators of cell proliferation, differentiation, and apoptosis. Mol Endocrinol; 17:161–171.
Ehtisham S, Barrett TG, Shaw NJ. (2000) Type 2 diabetes mellitus in UK children – an emerging problem. Diabet Med; 17:867–871.
Fagot-Campagna A. (2000) Emergence of type 2 diabetes mellitus in children: epidemiological evidence. J Pediatr Endocrinol Metab; 13 (Suppl 6):1395–1402.
Foresight (2007) Tackling Obesities: Future Choices – Modelling Future Trends in Obesity & Their Impact on Health. Available from: http://www.foresight.gov.uk/Obesity/14.pdf. Last accessed February 2010.
Haffner SM, Mykkanen L, Festa A, et al. (2000) Insulin-resistant prediabetic subjects have more atherogenic risk factors than insulin-sensitive prediabetic subjects: implications for preventing coronary heart disease during the prediabetic state. Circulation; 101:975–980.
Hedley AA, Ogden CL, Johnson CL, et al. (2004) Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA; 291:2847–2850.
Huang ES, Basu A, O’Grady M, Capretta JC. (2009) Projecting the future diabetes population size and related costs for the U.S. Diabetes Care; 32:2225–2229.
International Diabetes Federation (2009) IDF Diabetes Atlas, 4th Edition. Available from: http://www.diabetesatlas.org/content/europe. Last accessed December 2009.
Kaiser N, Leibowitz G, Nesher R. (2003) Glucotoxicity and beta-cell failure in type 2 diabetes mellitus. J Pediatr Endocrinol Metab; 16:5–22.
Massó-González EL, Johansson S, Wallander M-A, García-Rodríguez LA. Trends in the prevalence and incidence of diabetes in the UK – 1996 to 2005. J Epidemiol Community Health; doi:10.1136/jech.2008.080382.
Mohan V, Shanthirani S, Deepa R, et al. (2001) Intra-urban differences in the prevalence of the metabolic syndrome in southern India – the Chennai Urban Population Study (CUPS No. 4). Diabet Med; 18:280–287.
Mokdad AH, Ford ES, Bowman BA, et al. (2000) Diabetes trends in the US: 1990–1998. Diabetes Care; 23:1278–1283.
Smiley T. (2003) The role of declining beta cell function in the progression of type 2 diabetes: implications for outcomes and pharmacological management. Can J Diabetes; 27:277–286.
UK Prospective Diabetes Study (UKPDS) Group (1994) UK Prospective Diabetes Study XII: Differences between Asian, Afro-Caribbean and white Caucasian type 2 diabetic patients at diagnosis of diabetes. Diabet Med; 11:670–677.
UK Prospective Diabetes Study (UKPDS) Group (1998) Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet; 352:854–865.
Vilsbøll T, Krarup T, Deacon CF, et al. (2001) Reduced postprandial concentrations of intact biologically active glucagon-like peptide 1 in type 2 diabetic patients. Diabetes; 50:609–613.
CHAPTER 2
Overview of Current Diabetes Management
Following the sharp increase in diabetes prevalence that has occurred over the last few decades, 2.3 million people in England aged 17 years or over (NHS Information Centre, 2010) and 228 thousand people in Scotland (Scottish Diabetes Survey, 2009) were recorded on GP diabetes registers as of March 2010. With such a large population, routine clinical care for many of these patients is now managed mainly in primary care. Treatment should be aimed at alleviating symptoms and minimizing the risk of long-term complications with the overall aim of enabling people with diabetes to achieve a quality of life and life expectancy similar to that of the general population. Although this publication focuses on new mechanisms for glucose control, cardiovascular disease is the leading cause of morbidity and mortality in patients with type 2 diabetes, and management of diabetes needs to be multifactorial aiming to reduce complications by careful control of blood glucose as well as other cardiovascular risk factors.
Recommended targets for glycaemic control
Setting goals appropriate for the individual
People with type 2 diabetes form a diverse group varying significantly in terms of risk factors, disease dura...
Table of contents
- Cover
- Contents
- Title page
- Copyright
- Preface
- Chapter 1: Epidemiology and Pathogenesis of Type 2 Diabetes
- Chapter 2: Overview of Current Diabetes Management
- Chapter 3: The Incretin System
- Chapter 4: The Incretin Mimetics
- Chapter 5: Dipeptidyl Peptidase-4 Inhibitors
- Chapter 6: Sodium-glucose Cotransporter-2 Inhibitors
- Chapter 7: Pipeline Diabetes Therapies
- Chapter 8: Bariatric Surgery for the Treatment of Type 2 Diabetes
- Chapter 9: Organization of Diabetes Care
- Index