![]()
28
Carcinoma of unknown primary
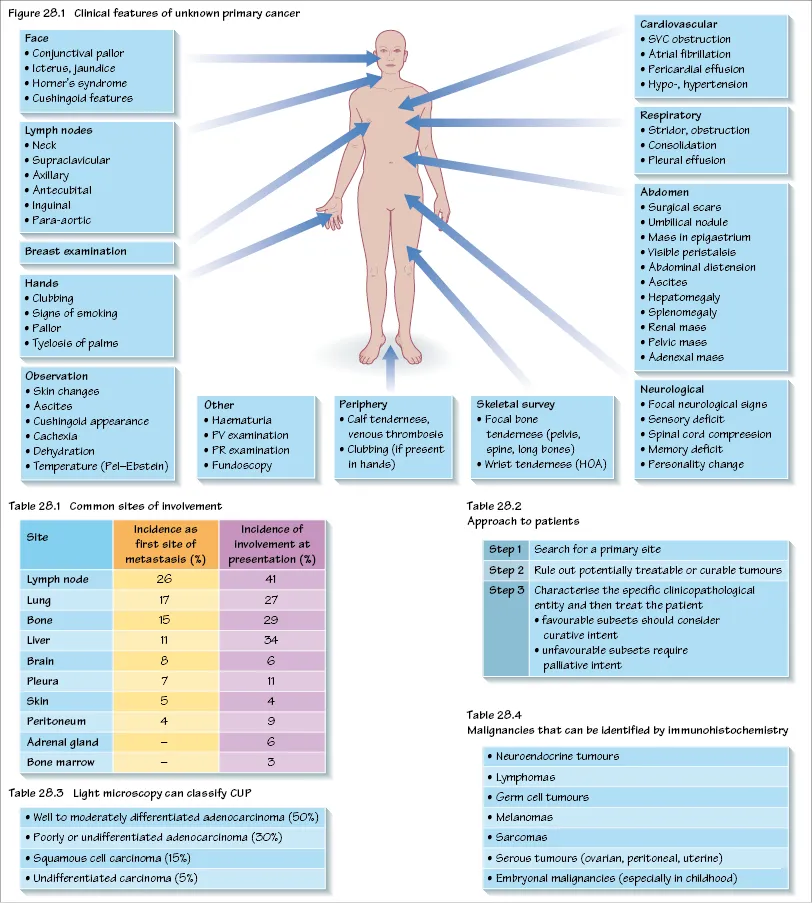
Epidemiology
Cancer will often present as a result of symptoms due to the primary site of the tumour, but sometimes the cancer is able to metastasise before the primary site is large enough to be detected. In contrast to known primary tumours, carcinomas of unknown primary (CUP) tend to have early dissemination, unpredictable metastatic pattern, aggressive nature and an absence of symptoms from the primary site. CUP is therefore defined as the detection of one or more sites of metastatic tumours for which investigations have failed to identify the primary site.
Up to 5% of all cancers are from an unknown primary, representing eight to 20 patients per 100 000 of the population per year. It is the seventh most frequent form of cancer and fourth most common cause of cancer death in both males and females. The median age at presentation is 60 years and 50% of patients present with multiple sites of involvement, with the rest having a single site in: liver, bones, lungs, or lymph nodes.
Aetiology
The usual histological diagnosis is that of adenocarcinoma or poorly differentiated carcinoma. Different tumours will spread in different patterns and this may be related to the chemokine and chemokine receptor expression by the tumour and stromal cells.
Clinical presentation
The clinical presentation will depend on the location of disease sites, but most patients (97%) have symptoms at metastatic sites (Table 28.1). Non-specific symptoms such as anorexia, weight loss and fatigue are common. See Chapter 10 for approach to clinical examination.
Investigations and staging
The first consideration is to exclude a potentially curable tumour, then to identify tumour types that are associated with a more favourable outcome, due to their responsiveness to treatment (Table 28.2). Despite extensive investigation, fewer than 20% of patients have a primary site identified antemortem, and even at autopsy 70% of cases have an unidentified primary site.
Primary sites are most frequently detected in the lung and pancreas, followed by other gastrointestinal and gynaecological malignancies.
Initial investigations
- Complete history and physical examination
- Full blood count
- Serum biochemistry and liver function
- Serum tumour markers (see Chapter 15)
- Urinalysis, stool testing for occult blood
- Chest X-ray
- Symptom-directed endoscopy
- Imaging of thorax, abdomen and pelvis (CT, MRI, or PET)
- Plain film imaging of bone pain sites
- Biopsy for histology (any site of disease) (Tables 28.3 and 28.4)
Patients should be referred to an oncologist who can advise on the required investigations, as there should be concern about overinvestigating the patient. This will have a cost effect and potentially can delay the initiation of appropriate treatment for the patient. Therefore a limited diagnostic approach with patient-benefit orientation aiming to recognise patients with good prognostic features is the best approach.
It is possible for patients to deteriorate during the investigation period and a precise diagnosis of the primary site may not be possible. Therefore, an approach is required that balances the need for sufficient tests to plan the management versus treatment of the disease.
Treatment
For patients with an incurable malignancy that is widely metastatic, treatment with combination systemic chemotherapy is the most appropriate. The choice of treatment will depend on the best assessment of likely primary site and consideration of the performance status of the patient. Radiotherapy is useful for specific sites of pain or discomfort. All treatment is administered with palliative intent and the aim of improving the patient’s quality of life. Furthermore, treatments should be discontinued if the patient is no longer gaining benefit or improvement in symptoms.
For patients with well or moderated differentiated adenocarcinoma of unknown primary, 90% demonstrate a low response rate to chemotherapy. Patients in this group have a poor prognosis.
Patients with potential ovarian or peritoneal primary sites can respond very well with appropriate chemotherapy; 40% achieve complete remission and 20% can achieve prolonged disease-free survival. Patients with axillary lymph node metastasis can be treated as for breast cancer and may require modified radical mastectomy.
Patients with poorly differentiated carcinoma or adenocarcinoma account for 30% of patients with CUP. They demonstrate a poor response to systemic chemotherapy, have a poor outcome and short survival. Such patients have a younger median age (40 years) and a rapid progression of symptoms. The most common sites of involvement include lymph nodes, mediastinum and retroperitoneum. Rarely, excellent responses and improved survival are demonstrated but no identified factors can predict response in these patients.
For patients with a single site of metastasis, consideration should be made for surgical resection and treatment with radiotherapy. This can produce significant periods of disease-free survival in some patients.
The presence of osteoblastic bone metastasis in a male patient should be considered for empirical hormonal therapy as for prostate cancer, regardless of the serum PSA level.
Prognosis
Patients with a diagnosis of carcinoma of unknown primary have a limited life expectancy with a median survival of 6–9 months. Patients with one to two sites of involvement, non-adenocarcinoma and no involvement of liver, bone, or adrenal gland have a median survival of 40 months. For patients with adrenal metastasis it is 5 months. Adverse prognostic factors include:
- adenocarcinoma histology;
- increasing number of involved organ sites;
- hepatic or adrenal involvement;
- supraclavicular lymph node involvement;
- male gender;
- poor performance status;
- weight loss (>10% of body mass).
![]()
29
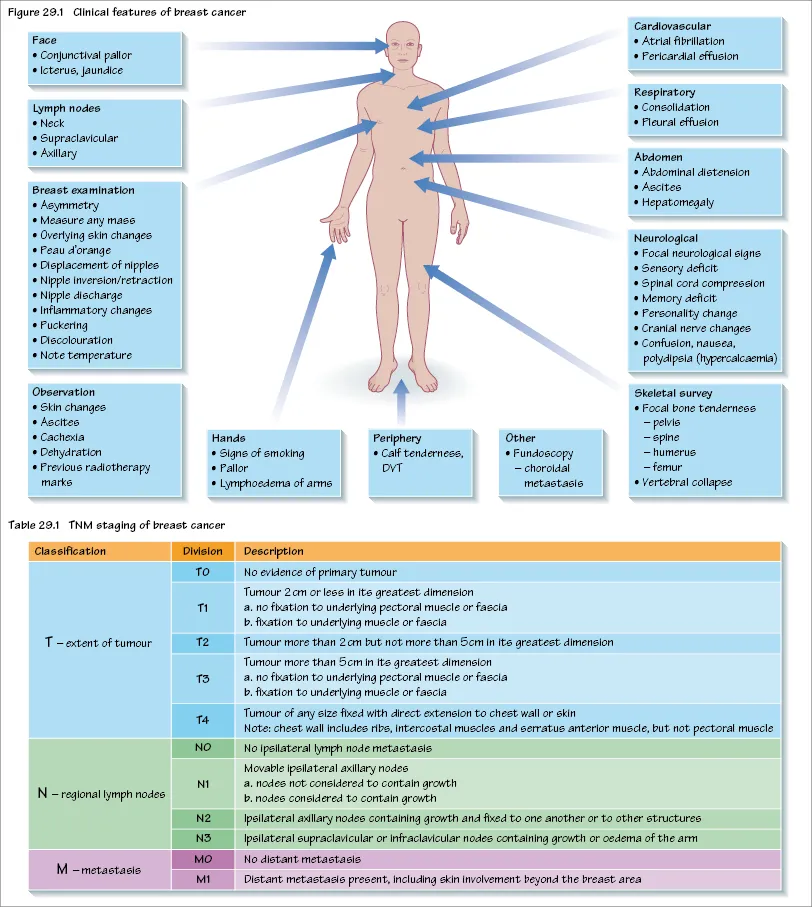
Breast cancer
Epidemiology
Breast cancer is the most frequent cancer in women after non-melanotic skin tumours (32% of female cancers) and is the commonest cause of death in women aged 35–54 years in England. It follows an unpredictable course with metastases presenting up to 20 years after initial diagnosis. England has one of the highest age-standardised incidences and mortality from breast cancer in the world, with a lifetime risk of breast cancer of 1 in 9. Earlier detection by screening and improved treatment are improving the 5-year survival.
Aetiology and pathophysiology
Both genetic and hormonal factors play a role in the aetiology of breast cancer. Hereditary predisposition is implicated in around 10% of breast cancer cases, including BRCA1 and BRCA2 hereditary breast cancer, and Li–Fraumeni syndrome. Prolonged exposure to oestrogen is thought to play a role and early menarche, late menopause, late first pregnancy (over 35 years old) and nulliparity are established risk factors.
The combined oral contraceptive pill does not significantly increase the relative risk for breast cancer (see Chapter 3), but hormone replacement therapy (HRT) has been shown to increase the incidence of breast cancer in long-term current users (relative risk 1.66).
Invasive ductal carcinoma with or without ductal carcinoma in situ (DCIS) is the commonest histology, accounting for 70% of cases, while invasive lobular carcinoma accounts for most of the remaining cases. DCIS constitutes 20% of screening-detected breast cancers, is multifocal in one-third of women and has a high risk of becoming invasive (10% at 5 years following excision only). Pure DCIS does not cause lymph node metastases, although these are found in 2% of cases where nodes are examined, owing to undetected invasive cancer. Lobular carcinoma in situ (LCIS) is a predisposing risk factor for developing cancer in either breast (7% at 10 years).
Clinical presentation
Breast cancer usually presents as a mass that persists throughout the menstrual cycle. A nipple discharge occurs in 10% and pain in only 7% of patients. Less common presentations include inflammatory carcinoma with diffuse induration of the skin of the breast, and this confers an adverse prognosis. Increasingly, women present as a consequence of mammographic screening. About 40% of patients will have axillary nodal disease, the likelihood of this rising with increasing size of the primary tumour. The involvement of axillary nodes by tumour is the strongest prognostic predictor. Distant metastases are infrequently present at diagnosis and the commonest sites of spread are: bone (70%), lung (60%), liver (55%), pleura (40%), adrenals (35%), skin (30%) and brain (10–20%).
Paget’s disease of the nipple accounts for 1% of all breast cancer cases and presents with a relatively long history of eczematous change in the nipple area with itching, burning, oozing, or bleeding. There may be a palpable underlying lump. The nipple contains malignant cells singularly or in nests. Prognosis is related to the underlying tumour.
Treatment
The management of carcinoma in situ is not well defined, as surgery with simple mastectomy or breast-conserving surgery followed by radiotherapy yield higher relapse rates, but salvage mastectomy at relapse can produce similar survival rates. The suggested treatment options for LCIS span from observation with annual screening to bilateral prophylactic mastectomy in selected patients. There appears to be no place for chemotherapy in either DCIS or LCIS, and the role of endocrine therapy is under evaluation.
For patients with early breast cancer, the treatment is wide local excision and axillary node surgery (dissection, sampling, or sentinel lymph node biopsy) followed by adjuvant breast radiotherapy. This achieves similar local control and survival rates to mastectomy with less mutilating surgery. Adjuvant radiotherapy is given to reduce the risk of local recurrence. This is reduced from 40–60% to 4–6% with the use of postoperative radiotherapy.
Adjuvant hormonal therapy with tamoxifen and aromatase inhibitors can improve disease-free and overall survival in pre- and postmenopausal patients who have tumours that express the oestrogen receptor (ER+). Patients at low risk with tumours that are small and ER+ require only adjuvant hormonal therapy. Patients with tumours that are ER+ and who are pre-menopausal should receive a luteinising hormone releasing hormone (LHRH) analogue, and postmenopausal patients, tamoxifen and an aromatase inhibitor.
Adjuvant chemotherapy is considered for patients at higher risk of recurrence. Factors that increase the risk of recurrence include a tumour >1 cm, tumour that is oestrogen receptor negative (ER–) or the presence of involved axillary lymph nodes. Such patients should be offered adjuvant chemotherapy, which improves ...