
Evidence-Based Interventional Pain Medicine
According to Clinical Diagnoses
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Evidence-Based Interventional Pain Medicine
According to Clinical Diagnoses
About this book
Unrelieved chronic pain is a worldwide epidemic
Chronic pain has been subject to multiple international initiatives through the World Health Organization. Interventional Pain Medicine, the use of minimally invasive techniques to relieve pain, is the best approach when simpler measures such as physical therapy or medications fail. However, these procedures can be associated with significant risk and expense. Establishing uniformity in diagnostic criteria and procedural performance can reduce both morbidity and unnecessary procedures, and hence healthcare expenditures.
While other texts explain how to perform these procedures, little focus has been given to diagnostic considerations: if and when these procedures should be performed. Evidence-Based Interventional Pain Medicine focuses on a balance between effectiveness and safety of interventional management for specific diagnoses, across all areas of chronic pain including:
- Head, neck and shoulder pain
- Lower back pain
- Neuropathic pain syndromes
- Complex Regional Pain Syndrome
- Pain in patients with cancer
- Vascular and visceral pain
Evidence-Based Interventional Pain Medicine provides essential knowledge for anyone who uses, or intends to use, interventional pain techniques.
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Information
| V1 only | 4% |
| V2 only | 17% |
| V3 only | 15% |
| V2 + V3 | 32% |
| V1 + V2 | 14% |
| V1 + V2 + V3 | 17% |
| Characteristic | Description |
| Character | Shooting, like an electric shock, stabbing, superficial |
| Seriousness | Moderate to very intense |
| Duration | Each pain attack lasts seconds but a number of different attacks can occur simultaneously after which there is a pain free interval |
| Periodicity | Periods of weeks to months without pain |
| Location | Distribution of T. neuralgia, mainly unilateral |
| Emanation | Within the area of the trigeminal nerve |
| Trigger factors | Light touching, such as when eating, talking or washing |
| Alleviating factors | Frequent sleep, anti-epileptics |
| Accompanying characteristics | Trigger zones, weight loss, poor quality of life, depression |
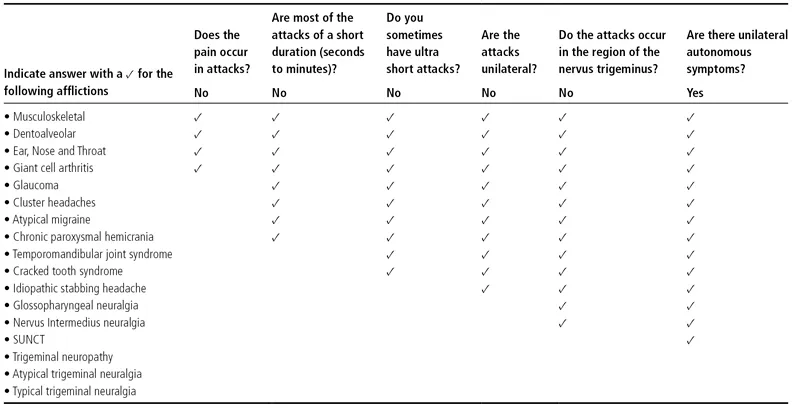
Table of contents
- Cover
- Title page
- Copyright page
- Contributor List
- Foreword
- Introduction
- 1 Trigeminal Neuralgia
- 2 Cluster Headache
- 3 Persistent Idiopathic Facial Pain
- 4 Cervical Radicular Pain
- 5 Cervical Facet Pain
- 6 Cervicogenic Headache
- 7 Whiplash-Associated Disorders
- 8 Occipital Neuralgia
- 9 Painful Shoulder Complaints
- 10 Thoracic Pain
- 11 Lumbosacral Radicular Pain
- 12 Pain Originating from the Lumbar Facet Joints
- 13 Sacroiliac Joint Pain
- 14 Coccygodynia
- 15 Discogenic Low Back Pain
- 16 Complex Regional Pain Syndrome
- 17 Herpes Zoster and Post-Herpetic Neuralgia
- 18 Painful Diabetic Polyneuropathy
- 19 Carpal Tunnel Syndrome
- 20 Meralgia Paresthetica
- 21 Phantom Pain
- 22 Traumatic Plexus Lesion
- 23 Pain in Patients with Cancer
- 24 Chronic Refractory Angina Pectoris
- 25 Ischemic Pain in the Extremities and Raynaud’s Phenomenon
- 26 Pain in Chronic Pancreatitis
- Index