![]()
CHAPTER 1
Diagnosis in evidence-based medicine
Diagnosis and Screening
The main goal of diagnostic tests is to identify the likely cause of an illness in patients presenting with clinical features, and to direct subsequent treatment. Diagnostic tests often have other uses, such as giving information about the prognosis of a condition, or monitoring patients during the course of an illness. Screening tests, in contrast, are usually used in otherwise healthy individuals to identify those who have an illness that has not yet caused any symptoms or signs.
Some diagnostic and screening tests have been used for hundreds (or even thousands of years), such as physical examination. Others have emerged as our understanding of disease processes has increased, coupled with advances in science and technology. Individuals, clinicians and health-care systems are now faced with a dazzling variety of different tests, ranging from simple point-of-care blood tests to complex imaging systems.
Unfortunately, few diagnostic tests are 100% accurate. Similar to treatments, diagnostic tests need to be evaluated in rigorous research. However, studies of diagnostic tests are often reported poorly, and many clinicians have difficulty understanding the results of diagnostic tests. Indeed a survey of 300 physicians in the USA found that 95% did not use numeric measures of diagnostic accuracy (sensitivity, specificity, likelihood ratios), but rather relied on their experience of tests in their patients and setting. This suggests that understanding even these diagnostic accuracy measures is difficult for most clinicians, let alone considering other outcomes of diagnostic tests. The dangers with this approach are that clinicians’ biases can become entrenched in practice (some of which may be correct and some incorrect), and it becomes difficult to incorporate new tests or new diagnostic information into practice.
Evidence-based medicine emphasizes clinical research and a critical appraisal of that research, rather than unsystematic clinical experience or opinion. This does not mean that clinical experience and an understanding of the underlying pathophysiology have become redundant. In fact, especially in diagnosis, the clinical instinct or ‘gut feeling’ that is acquired through experience is an important diagnostic tool. Evidence-based diagnosis seeks to combine clinical expertise with the best available evidence, while taking into account patient preferences.
Roles of Diagnostic Tests in Health Care
| Role | Description | Examples |
| Confirming or excluding a diagnosis | Used to confirm (‘rule in’) or exclude (‘rule out’) particular diagnoses. Most tests will be better at one than the other. May vary between different clinical settings/different spectrum of disease | Normal blood pressure measurement to exclude hypertension
Raised cardiac troponins to confirm cardiac ischaemia |
| Triage | An initial test in a clinical pathway, which usually determines the need for further (usually more invasive) testing. Ideal triage test is usually fairly rapid, and should not miss any patients (i.e. minimize false negatives) | Blood pressure and heart rate in initial triage of patients with multiple trauma to identify those with possible shock
D-Dimer to screen for presence of pulmonary embolism in patients who have shortness of breath |
| Monitoring | Tests that are repeated at periodic intervals in patients with chronic conditions, or in those receiving certain treatments, in order to assess efficacy of interventions, disease progression or need for changes in treatment | Glycated haemoglobin (HbA1c) to monitor glucose control in patients with diabetes
Anticoagulation tests for patients taking oral anticoagulants (warfarin)
Viral load and CD4 cell counts in patients with HIV infection |
| Prognosis | Provides information on disease course or progression, and individual response to treatment | CT scans in patients with known ovarian cancer to determine the stage |
| Screening | Detecting conditions or risk factors for conditions in people who are apparently asymptomatic. | Mammography screening for breast cancer
Cholesterol testing to detect people at greater risk of cardiovascular disease |
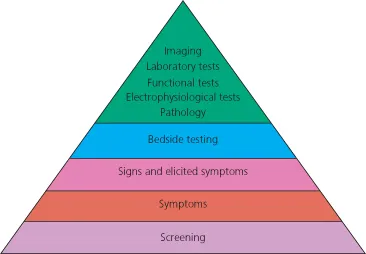
Different Types of Diagnostic Tests
In clinical practice, we use different types of tests, each with their own strengths and weaknesses. In general, tests that are readily available and painless are used in unselected patient groups (e.g. primary care), whereas tests with increasing level of invasiveness, costs and risks of harmful side effects are used in more highly selected patient populations (e.g. tertiary care hospital settings).
Screening
Screening is performed in individuals who do not currently have any symptoms or clinical signs to suggest the target condition. It is used in unselected target populations, who may be defined by age (e.g. screening for hypertension in elderly people) or gender (e.g. mammography in women), or other ‘risk factors’. The rationale and pitfalls of screening are discussed in Chapter 9.
Symptoms
In general, patients seek medical attention because they are experiencing certain symptoms. They might have a cough that is worrisome or feel pain. These symptoms can be used as diagnostic tests, and therefore have a diagnostic value for a particular target disorder. For example, a patient presenting to a clinician complaining of crushing central chest pain might be suspected of having a heart attack (myocardial infarction).
Signs and Elicited Symptoms
Symptoms and physical signs assessed during physical examination may have a different diagnostic value to those spontaneously reported by a patient. For example, certain symptoms that are commonly elicited from patients who are complaining of chest pain (such as worsening with exertion or spreading to the left shoulder) may increase the likelihood of a myocardial infarction. In addition, clinicians may observe physical abnormalities such as paleness or sweating, or an irregular pulse rate. Some physical signs are measures of physiological variables, such as blood pressure or fever. Developing clinical expertise involves not only learning how to elicit these clinical features, but also understanding their diagnostic value, including how reliable or repeatable they are (see Chapter 2 on inter- and intraobserver agreement).
Bedside or Point-Of-Care Testing
Many diagnostic tests are now available as point of care tests. These include tests on samples of urine (e.g. pregnancy tests), fingerstick drops of blood (e.g. glucose levels), or microbiological swabs (e.g. rapid antigen test for Group A streptococci in throat swabs). These tests are typically automated or simple to perform. Many tests that formerly required larger volumes of blood, or laboratory equipment, are now performed in real time during patient consultations. Point of care tests may be all that are required to exclude a condition (e.g. a negative throat strep test would usually exclude streptococcal tonsillitis) or confirm a condition (e.g. a positive urine pregnancy test).
Laboratory Tests
A vast number of more complex tests are typically performed only in laboratory or hospital settings, and involve a higher degree of skill to perform or interpret. These include the specialties of biochemistry, haematology, microbiology, radiology and pathology. Some involve no or minimal invasiveness (e.g. many blood tests, ultrasonography), whereas others may require more invasive procedures (e.g. coronary angiography, liver biopsy).
Additional types of diagnostic tests that are available only in hospital (or hospital outpatient) settings include many types of endoscopy, as well as functional tests (e.g. exercise ECG treadmill tests).
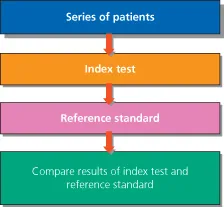
Basic Structure of Studies of Diagnostic Tests
The aim of diagnostic accuracy studies is usually to find out how well a test performs at ruling in (confirming) or ruling out (excluding) a clinical condition. This means that the results of a new test (the index test) are compared with the results of the reference standard (or ‘gold standard’). The reference standard is the test that is considered to be best at diagnosing the target condition in which you are interested.
Diagnostic test studies generally all share the same basic structure: a series of patients (or study participants) are selected; they all receive the index test, followed by the reference standard. Finally the results of the index test and reference standard are compared with each other.
Further Reading
Irwig L, Bossuyt PM, Glasziou P et al. Designing studies to ensure that estimates of test accuracy are transferable. BMJ 2002;324:669–71.
Knottnerus JA. The Evidence Base of Clinical Diagnosis. London: BMJ Books, 2002.
Knottnerus JA, Muris JW. Assessment of the accuracy of diagnostic tests: the cross-sectional study. J Clin Epidemiol ...