Practical Psychodermatology
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Practical Psychodermatology
About this book
Skin disease can be more than skin deep
Our skin is one of the first things people notice about us. Blemishes, rashes, dry, flaky skin – all these can breed insecurity, even suicidality, even though the basic skin condition is relatively benign. Skin disease can lead to psychiatric disturbance.
But symptoms of skin disease can also indicate psychological disturbance. Scratching, scarring, bleeding, rashes. These skin disturbances can be the result of psychiatric disease.
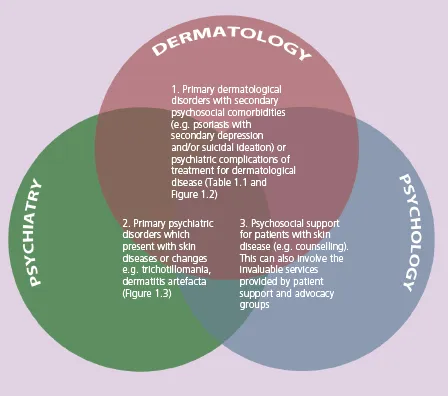
How do you help a dermatological patient with a psychological reaction? How do you differentiate psychological causes from true skin disease? These are challenges that ask dermatologists, psychiatrists, psychologists and other health care specialists to collaborate.
Practical Psychodermatology provides a simple, comprehensive, practical and up-to-date guide for the management of patients with psychocutaneous disease. Edited by dermatologists and psychiatrists to ensure it as relevant to both specialties it covers:
- History and examination
- Assessment and risk management
- Psychiatric aspects of dermatological disease
- Dermatological aspects of psychiatric disease
- Management and treatment
The international and multi-specialty approach of Practical Psychodermatology provides a unique toolkit for dermatologists, psychiatrists, psychologists and other health care specialists needing to care for patients whose suffering is more than skin deep.
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
Psychodermatology: interfaces, definitions, morbidity and mortality
- 17% of dermatology patients need psychological support to help them with the psychological distress secondary to a skin condition;
- 14% of dermatology patients have a psychological condition that exacerbates their skin disease;
- 8% of dermatology patients present with worsening psychiatric problems due to concomitant skin disorders;
- 3% of dermatology patients have a primary psychiatric disorder;
- 85% of patients have indicated that the psychosocial aspects of their skin disease are a major component of their illness;
- patients with psychocutaneous disease have a significant mortality from suicide and other causes.
| Primary dermatological disorders caused by or associated with psychiatric co-morbidity (Figure 1.2) | Primary psychiatric disorders that present with skin disease (Figure 1.3) |
|---|---|
| Psoriasis, eczema, alopecia areata, acne, rosacea, urticaria, vitiligo Visible differences (disfigurements) Inherited skin conditions (e.g. ichthyosis) May be caused, exacerbated by or associated with: Depression, anxiety, body image disorder, social anxiety, suicidal ideation, somatization, psychosexual dysfunction, schema, alexithymia, changes in brain functioning | Delusional infestation Body dysmorphic disorder Dermatitis artefacta Obsessive-compulsive disorders Trichotillomania Neurotic excoriation Dysaesthesias Somatic symptom disorders Substance abuse Factitious and induced injury Others |


The psychodermatology multidisciplinary team
- Dermatologists
- Psychiatrists
- Psychologists
- Dermatology and other nursing colleagues
- Child and adolescent mental health specialists (CAMHS)
- Paediatricians
- Geriatricians and older age psychiatrists
- Social workers
- Trichologists
- Primary care physicians
- Child and/or vulnerable adult protection teams
- Patient advocacy and support groups
DSM-IV and DSM-5
ICD-10
Table of contents
- Cover
- Dedication
- Title page
- Copyright page
- Contributors
- Foreword
- Preface
- SECTION 1: Introduction
- SECTION 2: Management in psychodermatology
- SECTION 3: Skin diseases with secondary psychiatric disorders
- SECTION 4: Psychiatric disorders with secondary skin manifestations
- SECTION 5: Cutaneous sensory (pain) disorders
- SECTION 6: Special populations and situations
- Glossary
- Appendix: Screening questionnaires and scales
- Index
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app