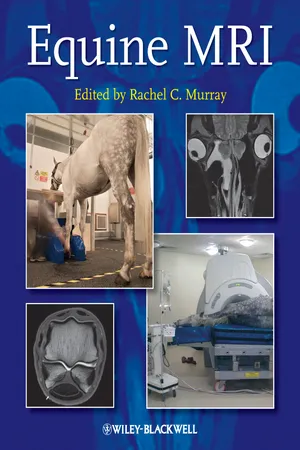
Equine MRI
About this book
Equine MRI is a unique, comprehensive guide to MRI in the horse. Edited by Rachel Murray, a leading authority and researcher in the field with over ten years of equine clinical MRI experience, the book also includescontributions from worldwide experts in the subject.
Divided into the following four sections, the book presents key information based on previous validation work and clinical practice:
- Principles of MRI, including the practicalities of image acquisition and interpretation
- Normal MRI anatomy and normal variations
- Different types of pathological change
- Options for clinical management and prognosis for different conditions
MRI is a rapidly expanding area in veterinary medicine that confers detailed, three-dimensional information on both bone and soft tissue. Expanding clinical knowledge, improvements in technology, and practical application of MRI to the standing and recumbent horse means this useful imaging modality has become an integral and essential part of the diagnostic evaluation in lameness and is a realistic option for investigation of ophthalmological, neurological and cranial pathology.
Equine MRI enables readers to understand the best ways to achieve good quality images, and provides a detailed explanation of the problems that may occur.
With close to 950 normal and abnormal images, this book offers considerable detail and examples of both common and uncommon problems, making it a great reference for equine veterinarians, veterinary students, specialists in equine surgery, and specialists in veterinary imaging.
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
- ill-defined osseous cyst-like lesions (OCLLs) in the spongiosa of the navicular bone without apparent communication with the flexor (palmar) cortex, or with equivocal radiolucent zones in the flexor cortex of the navicular bone associated with focal, moderate or intense increased radiopharmaceutical uptake (IRU)
- punctate focal core lesions in the DDFT in the pastern, with or without IRU in the region of the DDFT in pool phase scintigraphic images, or at its insertion in the distal phalanx in bone phase images
- enlargement of a collateral ligament (CL) of the distal interphalangeal (DIP) joint with or without change in echogenicity, or with focal IRU in the distal phalanx at the site of insertion of a CL of the DIP joint.
| Injured structure* | Number of horses (%) | Comments |
| Navicular bone | 21 (3.6) | + 31 horses with multiple injuries, 4 CL DIP joint |
| Navicular bone and DDFT | 60 (10.3) | + 60 horses with multiple injuries, 1 DSL |
| DSIL | 20 (3.4) | + 53 horses with multiple injuries, 5 navicular bone and DDFT, 1 navicular bone, 4 CL DIP joint, 1 distal phalanx |
| CSL | 3 (0.5) | + 57 with multiple injuries, 1 CL DIP joint |
| DDFT | 89 (15.2) | + 52 horses with multiple injuries, 3 primary distal phalanx pathology, 12 CL DIP joint |
| CL DIP joint | 179 (30.1) | + 106 horses with multiple injuries, 15 DDFT, 11 navicular bone and& DDFT, 4 primary distal phalanx pathology |
| SSL | 2 (0.5) | |
| Multiple injuries | 176 (30.1%) | |
| DIP joint | 8 (1.4) | + 10 horses with multiple injuries, 6 CL DIP joint, 1 DSIL |
| Primary injury of the middle and/or distal phalanges | 25 (4.3) | Includes 5 with evidence of previous penetrating injury + 23 horses with multiple injuries, 10 CL DIP joint, 1 navicular bone and DDFT |
| Distal border | Smooth extension of the distal border into the DSIL Entheseophyte formation Irregular thickness of distal cortex with mineralization extending proximally Enlargement of synovial invaginations Distal border fragment with no reaction in parent bone Distal border fragment with change in contour and signal intensity in adjacent navicular bone |
| Proximal border | Entheseophyte formation Endosteal mineralization Proximal border fragment |
| Flexor (palmar) border | Endosteal irregularity Increased thickness of flexor cortex Focal increased signal in flexor cortex in all image sequences Focal fluid accumulation palmar to bone consistent with fibrocartilage loss More extensive loss of fibrocartilage Linear increase in signal intensity through flexor cortex in STIR images Focal disruption of flexor cortex, with reaction (abnormal fluid and mineralisation) extending dorsally into the spongiosa Adhesions of DDFT |
| Dorsal border | Periarticular osteophyte formation Endosteal mineralization |
| Spongiosa/medulla | Discrete osseous cyst-like lesions in the distal third of the bone Diffuse increased signal intensity on STIR images Focal increased signal on STIR images at insertion of CSL and/or origin of DSIL Linear increased signal on STIR images between insertion of CSL and origin of DSIL Focal or diffuse decreased signal intensity on T1- and T2-weighted images consistent with mineralization |
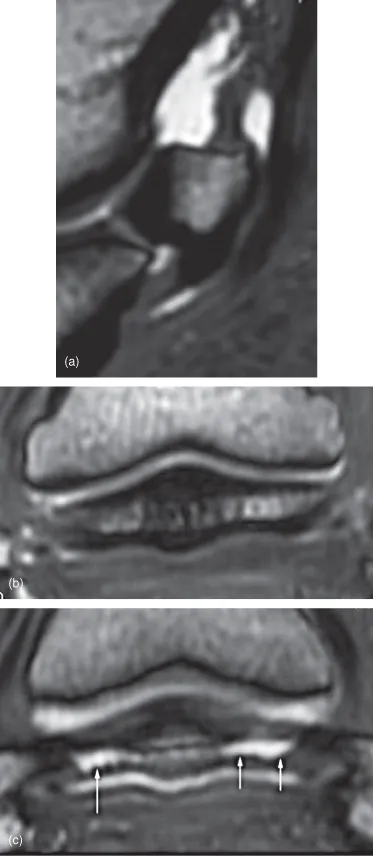
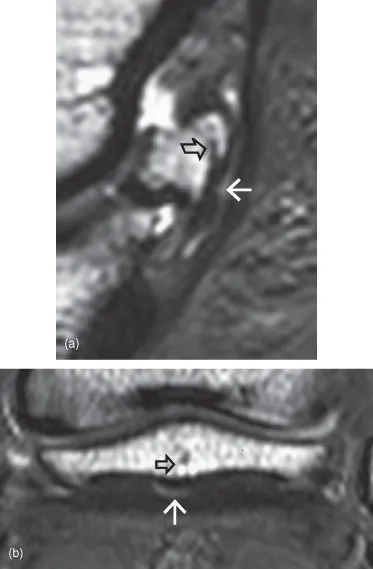
Table of contents
- Cover
- Half title page
- Title page
- Copyright page
- Contributors
- Foreword
- Preface
- Acknowledgements
- Part A: Principles of MRI in horses
- Part B: Normal MRI anatomy
- Part C: Pathology
- Part D: Clinical management and outcome
- Index
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app