eBook - ePub
ECG at a Glance
About this book
Highly Commended in the Cardiology category at the British Medical Association Book Awards 2009
This brand new title in the popular at a Glance seriescombines the science behind ECGs with how to use them to guide diagnosis and treatment. These key skills are fundamental for examination of the cardiovascular system and all medical students and specialist nurses are expected to be proficient at ECG interpretation.
The at a Glance approach provides a large number of clear diagrams and example ECGs alongside concise text, putting the ECGs into a clinical context, all in easy-to-absorb double-page sections.
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
1
Introduction to the ECG
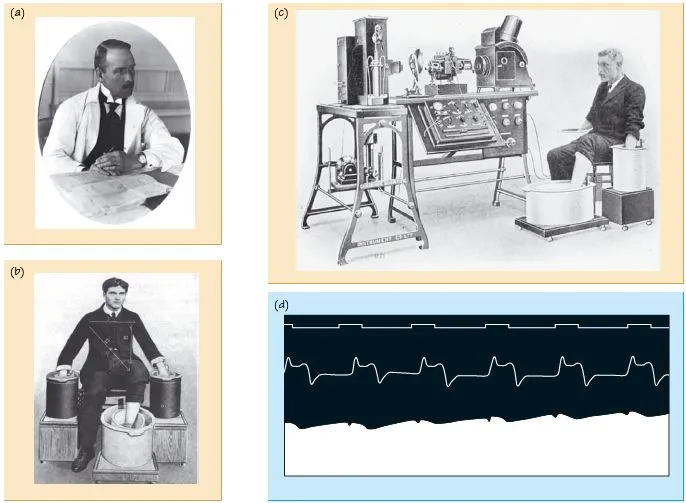
Fig. 1.1 (a) Willem Einthoven, in the early 1990s. (b) Early ECG recording required the arms and legs to be placed in saline buckets. (c) An early ECG machine. (d) One of the first ECGs recorded by Augustus Waller (top trace = time, middle trace = chest wall motion, bottom strip = the ECG).
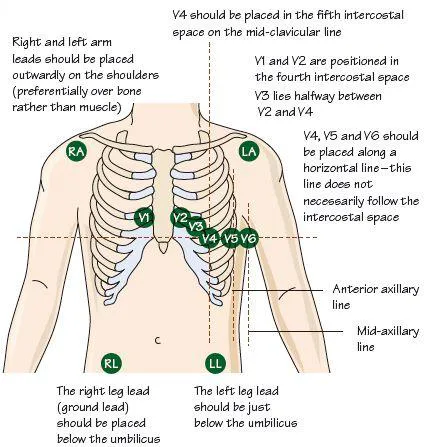
Fig. 1.2 ECG lead placement for an exercise ECG – in a resting ECG the leads to the legs are attached to electrodes just above the ankles. The ECG can be extended further beyond V6, to include leads V7–9, which extend posteriorly on the left chest. The leads can also be extended further rightward beyond lead V1, as ‘right-sided chest leads’.
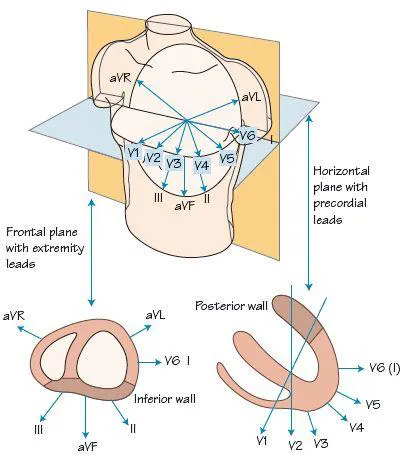
Fig. 1.3 The direction from which the basic 12-leads of the ECG examine the heart.
The electrocardiogram (ECG) is a wonderful tool, cheap, widely available, and incredibly useful. It informs diagnosis, guides and assesses the response to therapy and provides vital data on prognosis. In epidemiological use it gives great insights, e.g. it informs us that 30% of myocardial infarctions (MIs) are clinically silent, and that hypertensive heart disease when associated with certain ECG changes has a high mortality. The ECG informs us not only in acquired heart disease but also in genetic disease, e.g. hereditary long QT or Brugada syndrome. The diagnostic role extends beyond cardiac disease to pulmonary emboli, electrolyte imbalance, rheumatic disease, fitness level, liver disease, diabetes, starvation, etc. It is probably the most useful investigative tool in the whole of medicine.
A brief history of the ECG
The development of the ECG started in the mid 19th century with ideas concerning the role of electricity in the heart, then with the development of increasingly sensitive ways to measure this electricity. The early ECG machines were vast and required a water-cooled jacket! Technological advances in the early 20th century saw recording devices become increasingly small and by 1928 weighed ‘only’ 50 lbs (22 kg), described as being ‘portable’. Weight and size reduction continued and current devices weigh only a few pounds. The modern 12 leads of the ECG were formalized in 1942, with:
- the addition of the three augmented limb leads (aVR, aVL and aVF) of Emanuel Goldberger; to the
- pre-existing three standard leads (I, II, III) so fully explored by the ‘greats’ of the ECG, Einthoven, Lewis, Mackenzie, and Wilson; and the
- six chest leads (V for voltage 1–6, the technical aspects being formalized in 1938 by the American Heart Association and the British Cardiac Society).
Subsequent years saw an explosion in ECG-based research, and > 150 000 articles on the ECG have now been published!
The ECG in arrhythmias
The early use of the ECG was in arrhythmias, with the classic finding of Wenckebach in 1899 (Wenckebach block), of John Hay in Liverpool in 1905 (Mobitz type II block) and Arthur Cushny, a London professor, in 1907 on atrial fibrillation, an arrhythmia subsequently greatly investigated by Thomas Lewis (University College Hospital, London). Lewis obtained an ECG from a horse with atrial fibrillation and confirmed the diagnosis by examining the atria when the horse was slaughtered! Einthoven made vital contributions and earned the Nobel prize in 1924, the same year that Mobitz published his seminal ECG findings in second degree heart block. The surface ECG findings in many cardiac arrhythmias were elucidated in the mid 20th century, leading inexonerably to greater understanding and better treatment. Catheters allowing the recording of intracardiac ECG signals became available in the mid-century, leading logically to protocols to stimulate the heart to provoke arrhythmias (the electrophysiological study). These intra-cardiac recordings led to major progress in the diagnosis and treatment of arrhythmias. The external ambulatory recorder, developed by the Montana physician Holter in the 1950s led to discoveries in arrhythmias, circadian rhythm, and cardiac autonomic function (heart rate variability). Technology allowed the development of implantable ECG recorders (the Reveal device), and defined the role of the tilt-table test and carotid sinus massage. Advances continue, e.g. the discovery of the genetic pro-arrhythmic disease by the Brugada brothers in 1992.
The ECG and arrhythmia device therapy
Pacing therapy for slow heart beats had been known of for many years before external devices (bulky and unreliable) became available in 1952. The real breakthrough came in 1958 with the first implantable pacemaker. Subsequent years saw increasing miniaturization, longer battery life, sensing functions and full programmability. Though the knowledge that large direct current applied across the heart could terminate ventricular fibrillation was known from the work of Prevost and Batelli, professors at Geneva, from 1899, it was not until 1947 that Beck, in Cleveland was able to successfully demonstrate defibrillation from ventricular fibrillation (VF) during heart surgery. This led to successful closed chest cardioversion in 1956, and by the 1960s external defibrillators were routinely saving many lives. A logical development was the internal defibrillator, widely available by the mid 1990s. Even more recent is cardiac resynchronization therapy, useful in treating heart failure.
The ECG and coronary disease
The early 19th century saw the discovery of the classic changes of ‘full-thickness’ myocardial infarction and angina. It was realized early on that many patients with coronary disease had normal resting ECGs. Using exercise to provoke angina, and then record an ECG became widely accepted by the middle third of the century and in 1963 Bruce proposed his classic exercise test. The ability to diagnose coronary disease became widespread, underpinning both the need for and the development of coronary angiography and revascularization. In the 1980s the role of thrombolytic therapy in ST segment elevation but not non-ST segment MI was understood. The role of the ECG in risk stratifying MI continues to evolve, with multiple ECG-based risk scores now available.
2
Strengths and weaknesses of the ECG
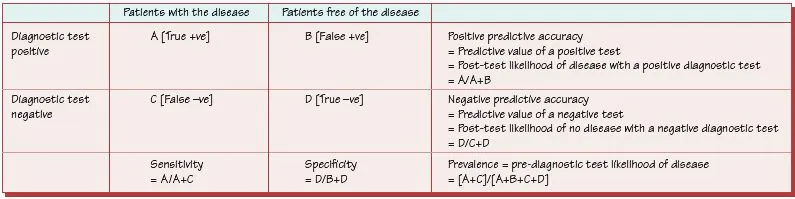
Fig. 2.1 The definition of sensitivity, specificity, positive and negative predictive accuracy.
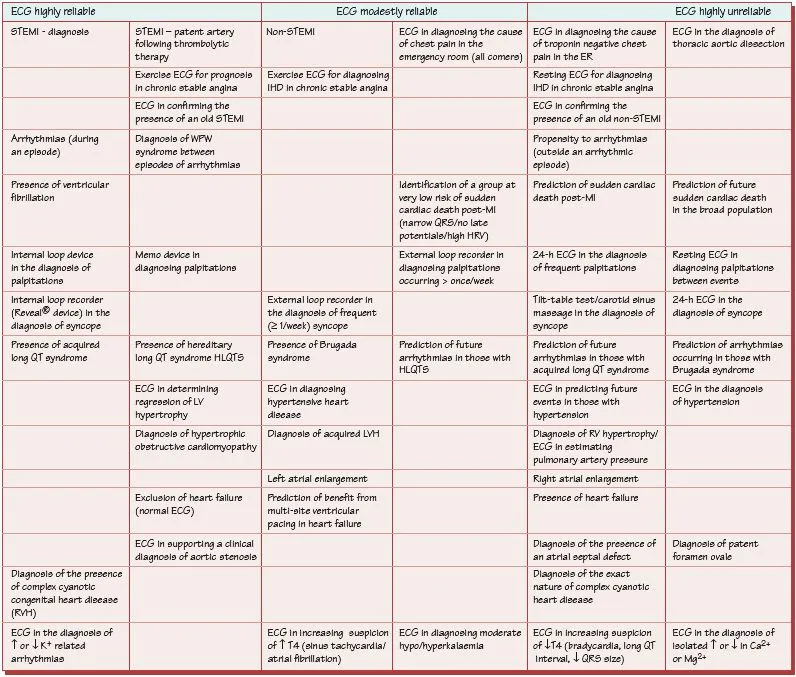
Fig. 2.2 The reliability of the ECG in diagnosis and management.
The ECG is a powerful tool, useful diagnostically and therapeutically in suspected cardiac disease, in non-cardiac problems, e.g. non-accidental poisoning, metabolic disturbance, etc, and in monitoring the heart rate of sick patients. ECGs are so widespread that physicians should understand its strengths and weaknesses.
Diagnostic role of the ECG
You should be aware of what proportion of those with a diagnosis have a diagnostic ECG, what proportion do not, and what proportion of people with a diagnostic ECG do not have t...
Table of contents
- Cover
- Table of Contents
- Preface
- 1 Introduction to the ECG
- 2 Strengths and weaknesses of the ECG
- 3 Basis of the ECG
- 4 The normal P wave
- 5 The normal QRS complex
- 6 The T and U waves
- 7 Abnormalities in the shape of the P wave – left and right atrial enlargement
- 8 Increased QRS amplitude
- 9 Q waves and loss of R wave height
- 10 QRS axis deviation
- 11 Long PR interval and QRS broadening
- 12 Delta waves
- 13 ST elevation
- 14 ST depression
- 15 Mild T wave flattening
- 16 Deep T wave inversion
- 17 QT interval and U wave abnormalities
- 18 Acute chest pain
- 19 Chronic chest pain
- 20 Acute breathlessness
- 21 Chronic breathlessness
- 22 Palpitations
- 23 Syncope
- 24 Hypertension
- 25 Shock
- 26 Stroke
- 27 Emotion and the ECG
- 28 Sudden cardiac death
- 29 Acute coronary syndromes
- 30 Non-ST segment elevation myocardial infarction
- 31 ST segment elevation myocardial infarction
- 32 Aortic valve disease and hypertrophic cardiomyopathy
- 33 Mitral valve disease
- 34 Cardiomyopathy and myocarditis
- 35 Pulmonary hypertension
- 36 Congenital heart disease
- 37 Endocrine disease and electrolyte disruption
- 38 Psychological disease and its treatment
- 39 Genetic pro-arrhythmic conditions
- 40 Distinguishing supraventricular from ventricular tachycardia
- 41 Narrow complex tachycardia
- 42 Atrial ectopic beats
- 43 Atrial fibrillation
- 44 Atrial flutter and atrial tachycardia
- 45 Atrioventricular nodal re-entrant tachycardia
- 46 Atrioventricular re-entrant tachycardia
- 47 Ventricular ectopics
- 48 Non-sustained ventricular tachycardia
- 49 Monomorphic ventricular tachycardia
- 50 Polymorphic ventricular tachycardia
- 51 Ventricular fibrillation
- 52 Sinus node disease
- 53 Left bundle branch block
- 54 Right bundle branch block
- 55 First degree atrioventricular block – long PR interval
- 56 Second degree atrioventricular block
- 57 Atrioventricular block – third degree (complete) heart block
- 58 Pacemakers – basic principles
- 59 Anti-bradycardic pacemakers
- 60 Anti-tachycardic and heart failure devices
- 61 External and internal loop recorders
- 62 Tilt-table test and carotid sinus massage
- 63 Twenty-four hour ECGs
- 64 The exercise stress test
- 65 Invasive electrophysiological studies
- Case studies and answers
- Appendix
- Index
- End User License Agreement
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn how to download books offline
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 990+ topics, we’ve got you covered! Learn about our mission
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more about Read Aloud
Yes! You can use the Perlego app on both iOS and Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app
Yes, you can access ECG at a Glance by Patrick Davey in PDF and/or ePUB format, as well as other popular books in Medicine & Cardiology. We have over one million books available in our catalogue for you to explore.
