- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
ECGs for the Emergency Physician 2
About this book
An ideal accompaniment to ECGs for the Emergency Physician Volume 1
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access ECGs for the Emergency Physician 2 by Amal Mattu,William J. Brady in PDF and/or ePUB format, as well as other popular books in Medicine & Internal Medicine & Diagnosis. We have over one million books available in our catalogue for you to explore.
Information
Part 1
Focus on dysrhythmias
Case histories
1. 63 year old woman with palpitations, weakness, and dyspnea
2. 71 year old febrile man with pneumonia
3. 54 year old dehydrated woman with gastroenteritis and recurrent syncope, a) during an episode of "syncope", b) after spontaneous conversion
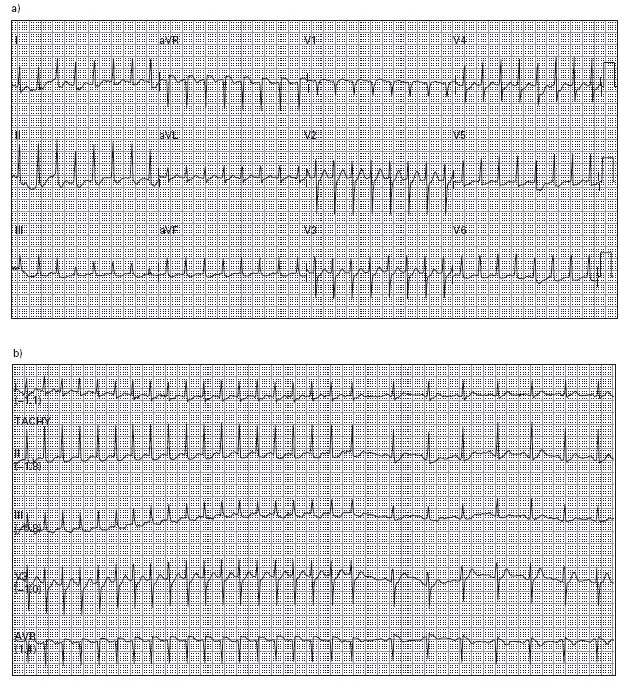
4. a) 18 year old woman with palpitations, dizziness, and hypotension, b) during treatment
5. 68 year old man with hypertension, managed with three medications, presenting with profound weakness
6. 57 year old woman with palpitations and exercise intolerance
7. 42 year old man 30 minutes after receiving fibrinolytics for an acute myocardial infarction
8. 53 year old man with past myocardial infarction presenting with hypotension and acute pulmonary edema
9. 79 year old woman with hypertension and chronic congestive heart failure complaining ofweakness and dyspnea
10. 29 year old man presenting with an ankle fracture; the patient is a long-distance runner
11. 71 year old woman with syncope
12. 79 year old man with progressive weakness
13. 59 year old woman being resuscitated during a cardiac arrest
14. 68 year old woman with sudden loss of consciousness
15. 66 year old man with a history of sick sinus syndrome and hypertension who notes extreme dizziness

16. 56 year old woman with recently diagnosed acute myocardial infarction
17. 26 year old woman with extreme anxiety after cocaine ingestion (nasal)
18. 18 month old child with fussiness and poorfeeding
19. a)–d) 54 year old man with chest pain suddenly becomes unresponsive
20. 60 year old man with dyspnea, profound weakness, and hypotension
21. 65 year old woman with chest pain suspected of acute myocardial infarction and sudden loss of consciousness
22. 67 year old woman with the sensation of a rapid heart beat
23. 65 year old man with chronic obstructive pulmonary disease and acute dyspnea
24. 75 year old woman with a decreased level of consciousness
25. 16 year old boy presents after a syncopal episode, now with recurrent sudden loss of consciousness
ECG interpretations and comments
(Rates refer to ventricular rate unless otherwise indicated)
1. Atrial fibrillation, ventricular rate 138. The rhythm is a narrow QRS complex, irregularly irregular tachycardia. The differential diagnosis includes atrial fibrillation, atrial flutter with variable conduction, and multifocal atrial tachycardia (MAT). Given the absence of distinct P-waves or flutter waves, the diagnosis of atrial fibrillation is made.
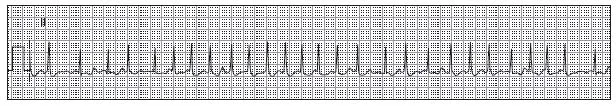
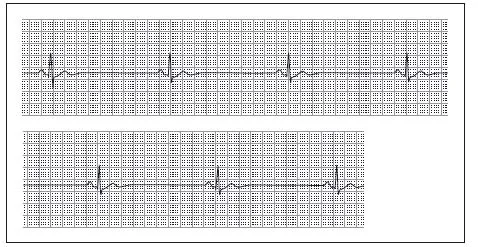
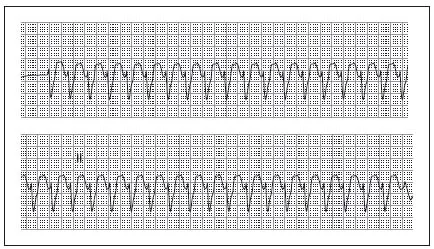
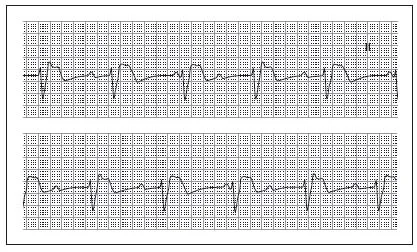
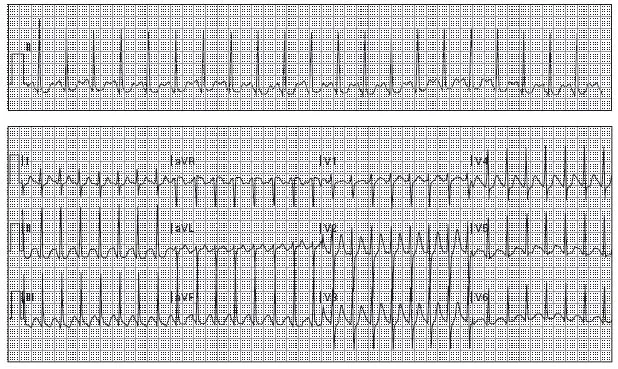
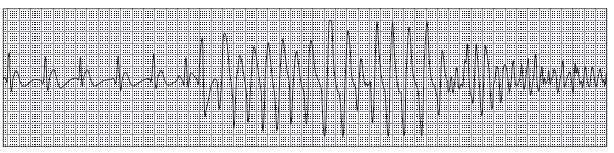
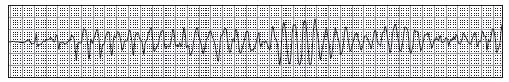
2. Atrial fibrillation, ventricular rate 96, artifact. The rhythm is initially irregularly irregular without distinct atrial activity, consistent with atrial fibrillation. The rhythm terminates with an episode of markedly irregular and rapid QRS complexes with changing morphologies. Considerations with this type of rhythm should include atrial fibrillation with Wolff-Parkinson-White syndrome (WPW), torsades de pointes, or artifact. The presence of “sharp points” at both the apices and nadirs of the QRS complexes is more consistent with artifact. See figure below.
This figure corresponds to case #2. Atrial fibrillation with subsequent wide QRS complex tachycardia
Note the arrows indicating QRS complexes which are occurring through this artifactual wide QRS complex event. The clinical correlation in this setting also aids in the interpretation—noting that the patient remains unchanged with a pulse corresponding to the original rhythm is helpful as well as observing rigors in this setting.
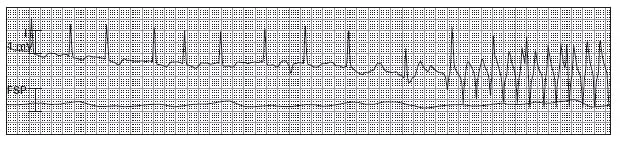
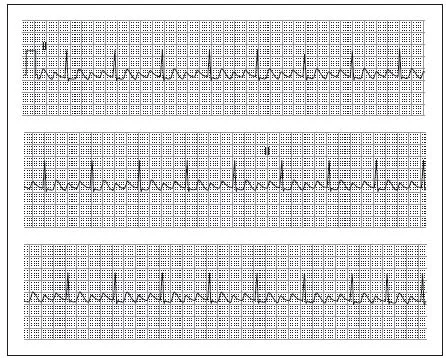
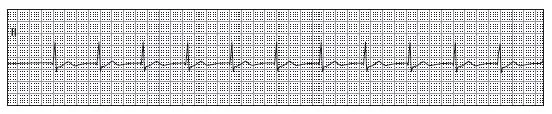
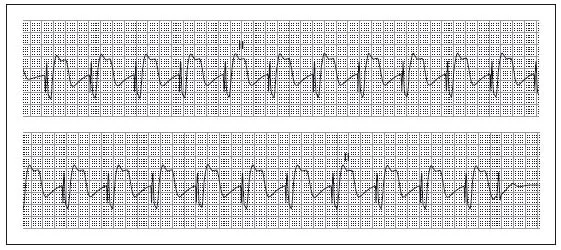
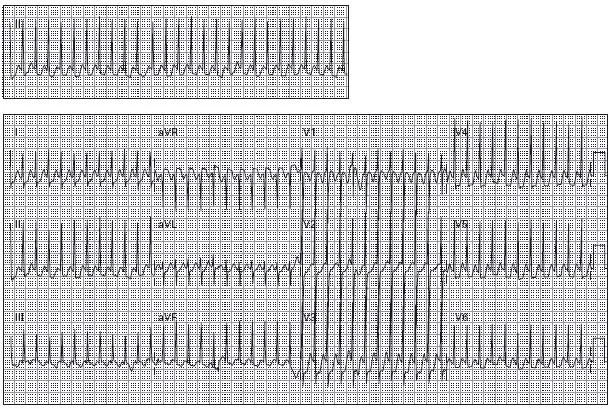
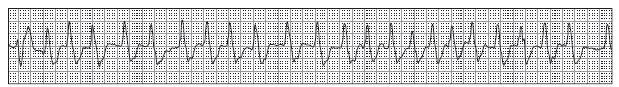
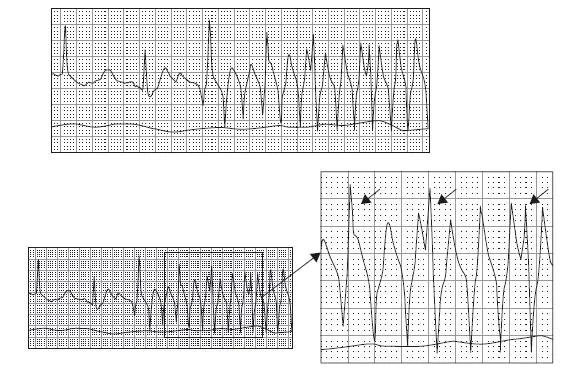
3. a) Polymorphic ventricular tachycardia, suspected torsade de pointes, rate 220. The rhythm is a wide QRS complex tachycardia with continuously varying QRS complex morphology, variation in the R-R intervals, and variation of the electrical axis consistent with polymorphic ventricular tachycardia. The QRS complexes appear to rotate around a fixed point, growing larger, then smaller, then larger, and so on. This pattern is suggestive of torsade de pointes. Torsade de pointes is a type of polymorphic ventricular tachycardia characterized by this unusual morphology. It is also defined when the baseline ECG demonstrates a prolonged QT-interval.
b) Sinus rhythm (SR), rate 64, premature atrial contractions (PACs) and premature ventricular contractions (PVCs), anteroseptal ischemia, prolonged QT-interval. The major abnormality here is prolongation of the QT-interval. The normal QT-interval will vary based on rate, and so the Bazett formula is used to correct the QT-interval based on the rate: corrected QT (QTc) = QT/√(RR). RR represents the R-R interval. The QTc is considered prolonged when >450 msec in men and >460 msec in women and children. A prolonged QTc indicates that the patient is at risk for torsade de pointes. The major risk for this dysrhythmia appears to occur when the QTc is ≥500 msec.1 In this case, there is marked prolongation (QT = 600 msec, QTc = 620 msec). The differential diagnosis of a prolonged QT-interval includes hypokalemia, hypomagnesemia, hypocalcemia, acute myocardial ischemia, elevated intracranial pressure, drugs with sodium channel blocking effects, hypothermia, and congenital prolonged QT syndrome. The QT-interval prolongation in this case (as well as the premature contractions) was caused by electrolyte abnormalities. T-wave inversions in leads V1–V3 suggest anteroseptal ischemia. See figure below.
This figure corresponds to case #3. Polymorphic ventricular tachycardia, torsade de pointes
It is important to note that the diagnosis of torsade de pointes requires demonstration of abnormal repolarization on the ECG, namely prolongation of the QT-interval. a) Note the significant beat-to-beat variation in the QRS complex morphology. b) Notethe significant beat-to-beat variation in the QRS complex amplitude.
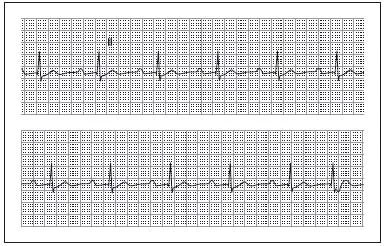
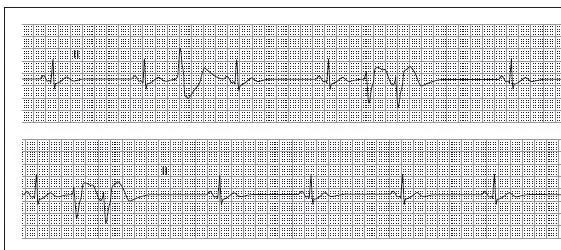
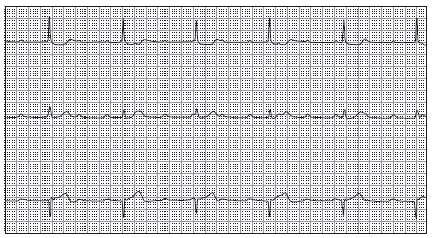
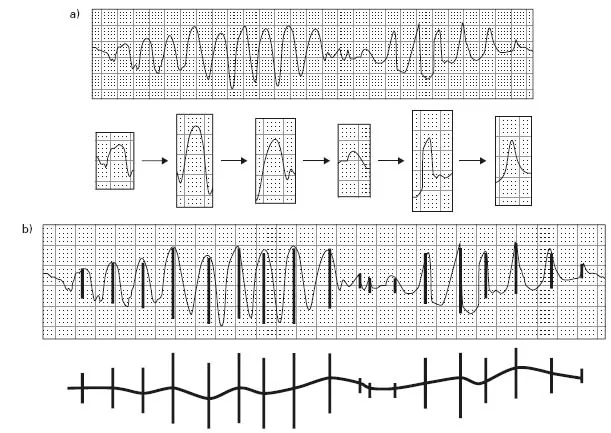
4. a) Paroxysmal supraventricular tachycardia, rate 190. The differential diagnosis of a regular, narrow QRS complex tachycardia includes sinus tachycardia (ST), paroxysmal supraventricular tachycardia (often simply referred to as supraventricular tachycardia, or SVT), and atrial flutter with 2:1 atrioventricular conduction. STand atrial flutter are characterized by distinct atrial activity on the ECG. SVTs, on the other hand, often have absence of clear atrial activity or they may demonstrate retrograde P-waves (P-waves that occur just after the QRS com plex, demonstrated in later cases). This ECG lacks obvious sinus P-waves or flutter waves, so the diagnosis of SVT is made. ST-segment depression is noted in the inferior and lateral leads, a common finding in cases of SVT and without clinical relevance as long as the ST-segment depression resolves after conversion to SR.
b) Paroxysmal supraventricular tachycardia, rate 190, with conversion to sinus tachycardia, rate 105. This multi-lead rhythm strip was obtained during intravenous adenosine infusion. A brief pause is followed by a return to SR.
5 Sinus bradycardia (SB), rate 20. A regular, narrow QRS complex bradycardia is present. A P-wave is associated with each QRS complex. The intrinsic rate of the sinus node is 60–100 beats/minute. When the sinus rate is <60 beats/minute, it is referred to as sinus bradycardia.
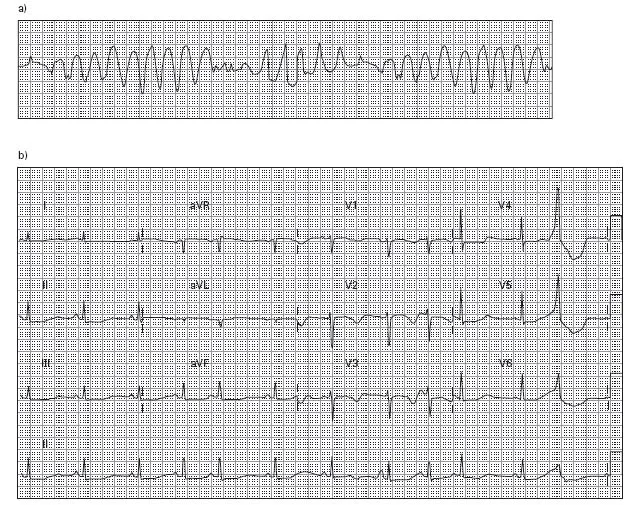
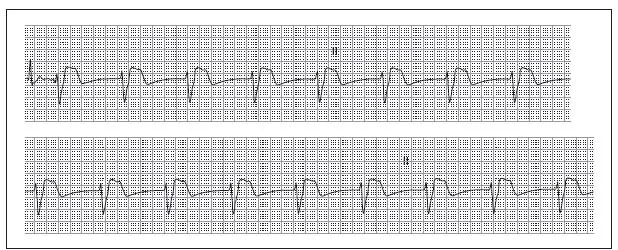
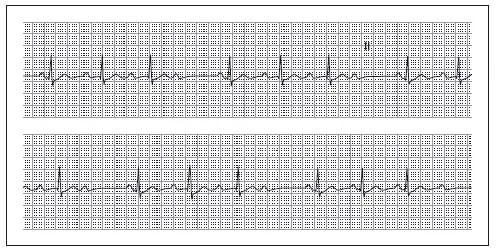
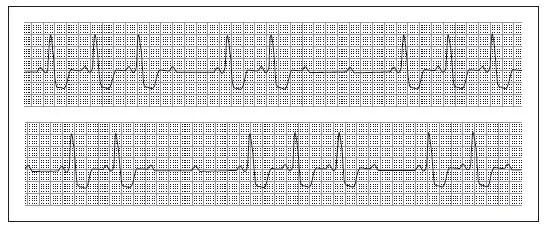
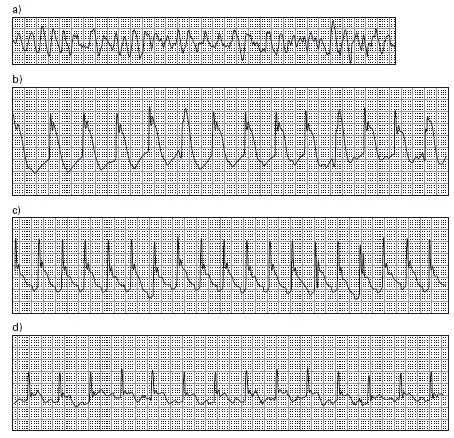
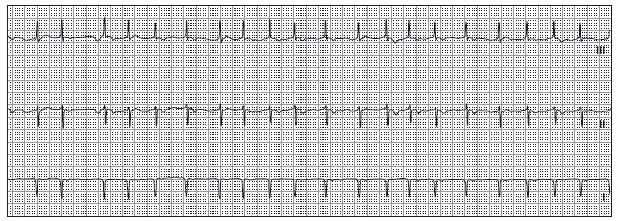
6 Atrial flutter with 4:1 atrioventricular (AV) conduction, rate 75. A regular, narrow QRS complex rhythm is present. Regular atrial activity is noted at a rate of 300 beats/minute (every 4th complex is hidden within a QRS complex) and produces a “saw-tooth” pattern typical of flutter waves between the QRS complexes. The ventricular response rate is one-quarter the atrial rate, consistent with a 4:1 AV conduction ratio. See figure below.
This figure corresponds to case #6. Atrial flutter
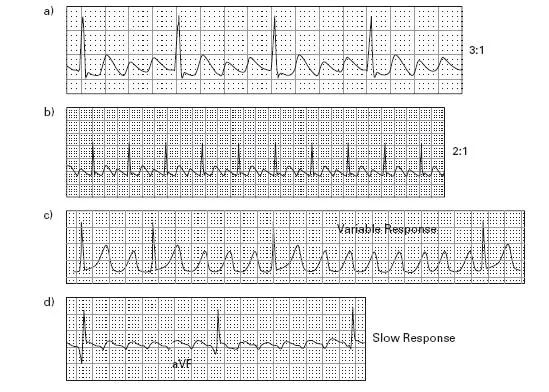
Note the “sawtooth” appearance of the atrial beats. These “sawtooth” waves are bestvisualized in the inferior leads (II, III, and aVF) and V1. The ventricular response ranges from slow to rapid with both regular and irregular response. The response is best expressed as a function of the number of P-waves relative to the QRS com pl ex that ultimately results from a conducted impulse. a) 3:1 conduction. b) 2:1 conduction. Notethat a ventricular rate of 150/minute should always prompt consideration of atrial flutter. c) Variable, or irregular, response. d) Slow response.
7. Accelerated idioventricular rhythm, rate 55. A regular, wide QRS complex rhythm is noted. No P-waves are present, ruling out an atrial origin for the beats. The likely rhythm, then, is ventricular. Because the normal ventricular escape rate is 20–40 beats/minute, this rhythm is termed an accelerated ventricular escape rhythm or accelerated idioventricular rhythm. This type of rhythm is commonly noted in patients with acute MI who spontan eously or therapeutically reperfuse. A junctional rhythm with aberrant ventricular conduction (e.g. bundle branch block) is also capable of producing a regular wide QRS complex rhythm at this rate and without P-waves; however, the QRS morphologies are not typical for the presence of either a left or right bundle branch block. A full 12-lead ECG would be helpful for clarification.
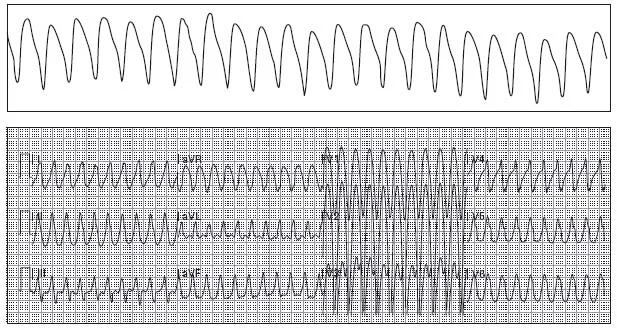
8. Probable ventricular tachycardia (VT), rate 170. The differential diagnosis of a regular, wide QRS complex tachydysrhythmia includes ST with aberrant conduction (e.g. bundle branch block), SVT or atrial flutter with aberrant ventricular conduction, and VT. Neither P-waves nor flutter waves are found, leaving SVT with aberrant ventricular conduction and VT as the two main diagnostic possibilities. Without any clinical information, it is estimated that >80% of the time these rhythms are confirmed as VT. Given the additional clinical information of the patient’s- age, past MI, hypotension, and acute pulmonary edema, however, the certainty of VT is nearly 100%. See figure opposite.
9. Accelerated AV junctional rhythm, rate 80. The QRS complexes are narrow and there are no P-waves noted, ruling out a ventricular rhythm and atrial rhythm, respectively. Narrow QRS complex rhythms of this type are likely to originate in the AV node. Because the intrinsic pacing rate of the AV node is 40–60 beats/minute, the rhythm is termed an accelerated AV junctional rhythm.
10. SR with first degree AV block, rate 60, premature junctional complex (PJC) with aberrant conduction. The rhythm has narrow QRS complexes which, with exception of the last QRS complex, are all followed by P-waves. The PR-intervals are constant and prolonged (320 msec; normal = 120–200 msec), diagnostic of a first degree AV block. The last QRS complex is a PJC with slight aberrant conduction: it appears early in the cycle, it is not preceded by a P-wav...
Table of contents
- Cover
- Title
- Copyright
- Foreword
- Preface
- Dedication
- Part 1: Focus on dysrhythmias
- Part 2 12-Lead ECGs (intermediate level)
- Part 3 12-Lead ECGs (advanced level)
- Appendix A: Differential diagnoses
- Appendix B: Commonly used abbreviations
- Index
- Advertisment