- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
ABC of Asthma
About this book
Asthma is a common condition with increasing prevalence. This new edition of the highly regarded ABC of Asthma has been thoroughly revised with reference to the latest British Thoracic Society guidelines on the management of asthma in children and adults. It covers the advances in practice and methods, with a new emphasis on delivery systems, self-dose assessment and delivery of care with different pharmacological approaches.
The ABC of Asthma is a concise, up-to-date overview of all aspects of asthma and includes two new chapters focussing on GP practice issues including clinical management and organisation of asthma care. It is ideal for GPs, junior doctors and medical students, nurses, and anyone dealing with the treatment of asthma in children and adults.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access ABC of Asthma by John Rees,Dipak Kanabar,Shriti Pattani in PDF and/or ePUB format, as well as other popular books in Medicine & Pulmonary & Thoracic Medicine. We have over one million books available in our catalogue for you to explore.
Information
CHAPTER 1
Definition and Pathology
OVERVIEW
- Asthma is an overall descriptive term but there are a number of more or less distinct phenotypes which may have different causes, clinical patterns and responses to treatment
- The clinical characteristic of asthma is airflow obstruction, which can be reversed over short periods of time or with treatment
- In the great majority of asthmatics, treatment is available to suppress asthma symptoms to allow normal activity without significant adverse effects
- Five to ten percent of asthmatics have asthma where control is difficult or side effects of treatment are troublesome
- Inflammation in the airway wall is an important feature of asthma and involves oedema, infiltration with a variety of cells, disruption and detachment of the epithelial layer and mucus gland hypertrophy
Asthma is a common condition that has increased in prevalence throughout the world over the last 20 years. It is estimated that around 300 million people are affected across the world. There is no precise, universally agreed definition of asthma (Box 1.1). The descriptive statements that exist include references to the inflammation in the lungs, the increased responsiveness of the airways and the reversibility of the airflow obstruction
Box 1.1 A definition of asthma
The International Consensus Report on the Diagnosis and Management of Asthma (Global Strategy for Asthma Management and Prevention) gives the following definition:
‘Asthma is a chronic inflammatory disorder of the airways in which many cells and cellular elements play a role.
The chronic inflammation is associated with airway hyperresponsiveness that leads to recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, particularly at night or in the early morning. These episodes are usually associated with widespread, but variable, airflow obstruction within the lung that is often reversible either spontaneously or with treatment’.
Asthma is an overall descriptive term but there are a number of more or less distinct phenotypes which may have different causes, clinical patterns and responses to treatment.
The clinical picture of asthma in young adults is recognisable and reproducible. The difficulties in precise diagnosis arise in the very young, in older groups and in very mild asthma. Breathlessness from other causes, such as increased tendency towards obesity, may be confused with asthma.
The clinical characteristic of asthma is airflow obstruction, which can be reversed over short periods of time or with treatment. This may be evident from provocation by specific stimuli or from the response to bronchodilators. The airflow obstruction leads to the usual symptoms of shortness of breath. The underlying pathology is inflammatory change in the airway wall, leading to irritability and responsiveness to various stimuli and also to coughing, the other common symptom of asthma. Cough may be the only or first symptom of asthma.
Asthma has commonly been defined on the basis of wide variations in resistance to airflow over short periods of time. More recently, the importance of inflammatory change in the airways has been recognised. There is no universally agreed definition but most contain the elements from the Global Initiative for Asthma.
Low concentrations of non-specific stimuli such as inhaled methacholine and histamine produce airway narrowing. In general, the more severe the asthma, the greater the inflammation and the more the airways react on challenge. Other stimuli such as cold air, exercise and hypotonic solutions can also provoke this increased reactivity. In contrast, it is difficult to induce significant narrowing of the airways with many of these stimuli in healthy people. In some epidemiological studies, increased airway responsiveness is used as part of the definition of asthma. Wheezing during the past 12 months is added to the definition to exclude those who have increased responsiveness but no symptoms.
Airway responsiveness demonstrated in the laboratory is not widely used in the diagnosis of asthma in the United Kingdom but is helpful when the diagnosis is in doubt. The clinical equivalent of the increased responsiveness is the development of symptoms in response to dust, smoke, cold air, and exercise; these should be sought in the history.
Labelling
In the past, there was a tendency to use the term wheezy bronchitis in children rather than ‘asthma’ in the belief that this would protect the parents from the label of asthma. More recently, there has been a greater inclination to label and treat mild wheezing or breathlessness as asthma. Self-reported wheezing in the past 12 months is used as the criterion for diagnosing asthma in many epidemiological studies but the symptom of wheezing is not limited to asthma.
These diagnostic trends probably contributed to rising figures on prevalence. However, there were real changes as studies through the 1970s and 1980s also showed increasing emergency room attendance, admission and even mortality. Recent studies show a levelling off or decline in mortality and in asthma attendances in primary and secondary care (Bateman et al., 2008).
The relevance of the early environment has been increasingly evident in epidemiological studies. A significant degree of the future risk of asthma and course of disease seems to be dependent on factors before or shortly after birth (Figure 1.1).
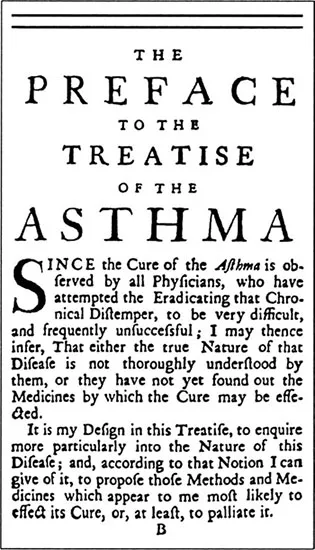
In the great majority of asthmatics, treatment is available to suppress asthma symptoms to allow normal activity without significant adverse effects. These are the goals of most asthma guidelines. However, these treatments are not always delivered efficiently and many patients with milder asthma remain symptomatic (Figure 1.2). Around 5–10% of asthmatics have asthma where control is difficult or side effects of treatment are troublesome. Although we understand more about the onset, pathology and natural history of asthma, little practical advance has yet been made in its cure or prevention.
In infants under the age of 2, wheezing is common because of the small size of the airways. Many of these infants have transient infant wheeze or non-atopic wheezing as toddlers and will not go on to develop asthma. In adults who smoke, asthma may be difficult to differentiate from the airway narrowing that is part of chronic bronchitis and emphysema that has been caused by previous cigarette smoking.
Figure 1.1 Genetics and the environment influence asthma.
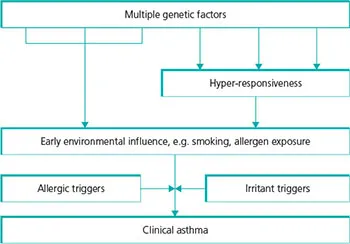
Figure 1.2 The preface to The Treatise of the Asthma by J Floyer, published in 1717.
Obesity is associated with an increased prevalence of asthma. The associations are complicated with increased airway responsiveness in obesity together with symptoms of breathlessness related to the higher mechanical load on the lungs.
The actual diagnostic label would not matter ifappropriate treatment were used. Unfortunately, evidence shows that children and adults who are diagnosed as having asthma are more likely to get appropriate treatment than children with the same symptoms who are given an alternative label. In adults, attempts at bronchodilatation and prophylaxis are more extensive in those who are labelled as asthmatic. Asthma is now such a common and well-publicised condition that the diagnosis tends to cause less upset than it used to. With adequate explanation, most patients and parents will accept it. The correct treatment can then be started. Persistent problems of cough and wheeze are likely to be much more worrying than the correct diagnosis and improvement in symptoms on treatment. The particular problems of the diagnosis of asthma in very young children are dealt with in Chapter 12.
Figure 1.3 In older smokers, COPD may be difficult to distinguish from chronic asthma.

Treating older patients
In older patients, the commonest dilemma is differentiation (Box 1.2) from chronic obstructive pulmonary disease (COPD) (Figure 1.3). Since both conditions are common, some patients will have both. A degree of increased airway responsiveness is found in COPD in relation to geometry from the narrower airways. Bron-chodilators will be appropriate for both conditions although the agent may vary. Inhaled corticosteroids are a mainstay of asthma treatment, when used early, but in COPD, they are less effective and are used to manage more severe disease or frequent exacerbations.
Box 1.2 Differential diagnosis in adults
| Chronic obstructive pulmonary disease | May be difficult to differentiate from chronic asthma in older smokers. The pathology differs, as does the degree of steroid responsiveness |
| Large airway obstruction | Caused by tumours, strictures, foreign bodies. Often misdiagnosed as asthma initially. Differentiated by flow-volume loop |
| Pulmonary oedema | Once called ‘cardiac asthma’: may mimic asthma, including the presence of wheezing and worsening at night |
Pathology
Since the 1990s, there has been a far greater interest and understanding of inflammation in the asthmatic airway (Figure 1.4). The inflammation in the airway wall involves oedema, infiltration with a variety of cells, disruption and detachment of the epithelial layer, and mucus gland hypertrophy (Figure 1.5). There is thickening of the smooth muscle. Changes occur in the subepithelial layer with the laying down of forms of collagen and other extracellular matrix proteins.
Figure 1.4 Inflammatory changes in the airway.
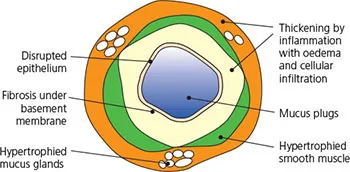
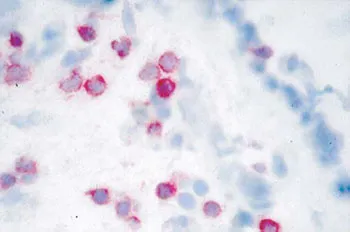
Figure 1.5 CD3+ lymphocytes in mucosa (courtesy of Professor Chris Corrigan).
This remodelling of the airway wall in response to persistent inflammation can resolve but may result in permanent fibrotic damage thought to be related to the irreversible airflow obstruction that may develop in poorly controlled asthma.
There is evidence that symptoms in very early life are related to lifelong change in lung function. Very early and prolonged intervention may be necessary to allow normal airway and lung development and prevent permanent changes. In older children, corticosteroids can suppress inflammation, but this returns, with associated hyper-responsiveness, when the drugs are stopped.
The inflammatory cells involved in asthma include eosinophils, mast cells, lymphocytes and neutrophils. Dendritic cells are monocyte-derived cells that present antigen and induce proliferation in naive T cells and primed Th2 cells. The antigen cross links immunoglobulin E (IgE) to produce activation and degranulation of mast cells. T lymphocytes appear to have a controlling influence on the inflammation characteristic of asthma. Th2 lymphocytes that produce interleukin 4, 5, 9 and 13 are increased in the airway in asthma. Inflammatory cells are attracted to the airway by chemokines and then bind to adhesion molecules on the vessel endothelium. From there, they migrate into the local tissue.
In acute inflammatory conditions such as pneumonia, the processes usually resolve. In asthma, chronic inflammation can disrupt the normal repair process; growth factors are produced by inflammatory and tissue cells to produce a remodelling of the airway.
There is proliferation of smooth muscle and blood vessels with fibrosis and thickening of the basement membrane. Hypertrophy and hyperplasia of smooth muscle increase responsiveness which, together with fibrosis, reduces airway calibre. Some of these changes may be reversible but others can lead to permanent damage and reduced reversibility in chronic asthma. A key question is whether early, effective anti-inflammatory treatment can prevent these changes.
The pathological changes may vary between asthmatics, some having predominantly eosinophilic infiltration while others may be mixed or neutrophilic (Anderson et al., 2007).
Clinical evidence
Early evidence on the changes in the airway wall came from a few studies of post-mortem material. The understanding advanced with the use of bronchial biopsies taken at bronchoscopy. These studies showed that, even in remission, there is persistent inflammation in the airway wall.
Alveolar lavage samples cells from the alveoli and small airways, giving another measure of airway inflammation. However, it cannot be repeated regularly and is not practical as a monitor in clinical practice. Induced sputum, produced in response to breathing hypertonic saline, is an alternative, more acceptable method which has been used to monitor control.
All these techniques sample different areas and cell populations and by themselves may induce changes that affect repeated studies. However, they have provided valuable information on cellular and mediator changes and the effects of treatment or airway challenge.
A simpler method involves analysis of the expired air. This has been used to measure exhaled nitric oxide produced by nitric oxide synthase, which is increased in the inflamed asthmatic airway. Other possibilities are measurement of pH of the expired breath condensate, carbon monoxide as a sign of oxidative stress or products of arachidonic acid metabolism such as 8-isoprostane. These methods hold promise for simpler methods of measuring airway inflammation but are not in routine use.
Mucus plugging
In severe asthma, there is mucus plugging within the lumen and loss of parts of the surface epithelium. Extensive mucus plugging (Figure 1.6) is the striking finding in the lungs of patients who die of an acute exacerbation of a...
Table of contents
- Cover
- Contents
- Title Page
- Copyright page
- Preface
- CHAPTER 1 Definition and Pathology
- CHAPTER 2 Prevalence
- CHAPTER 3 Diagnostic Testing and Monitoring
- CHAPTER 4 Clinical Course
- CHAPTER 5 Precipitating Factors
- CHAPTER 6 General Management of Chronic Asthma
- CHAPTER 7 Treatment of Chronic Asthma
- Chapter 8 General Management of Acute Asthma
- CHAPTER 9 Treatment of Acute Asthma
- CHAPTER 10 Methods of Delivering Drugs
- CHAPTER 11 Definition, Prevalence and Prevention
- CHAPTER 12 Patterns of Illness and Diagnosis
- CHAPTER 13 Treatment
- CHAPTER 14 Pharmacological Therapies for Asthma
- CHAPTER 15 Acute Severe Asthma
- CHAPTER 16 Clinical Aspects of Managing Asthma in Primary Care
- CHAPTER 17 Organisation of Asthma Care in Primary Care
- Index