eBook - ePub
Neurovascular Examination
The Rapid Evaluation of Stroke Patients Using Ultrasound Waveform Interpretation
- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Neurovascular Examination
The Rapid Evaluation of Stroke Patients Using Ultrasound Waveform Interpretation
About this book
The use of neurovascular ultrasound is of increasing importance in neurological practice, both for radiologists and increasingly by neurologists themselves. Written by the world's most renowned expert, this book explains
- ultrasound examination of a stroke patient
- scanning protocols
- interpretation of the results
Case examples (with a standard template presentation correlating presentation to waveform output) reinforce the book's practical nature.
Illustrated with photos of the tests, explanations, and with actual waveforms, images, and result interpretation, and enhanced with 'pearls' and 'avoiding pitfalls' features, it is a practical reference for those learning ultrasound as well as those using ultrasound in their practices.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Neurovascular Examination by Andrei V. Alexandrov in PDF and/or ePUB format, as well as other popular books in Medicine & Medical Technology & Supplies. We have over one million books available in our catalogue for you to explore.
Information
1
Understanding the Mechanisms and Dynamics of Cerebrovascular Events
“What does the term CVA “really” stand for? … Confused Vascular Assessment!”
Strokology 101
The time-honored use of a nonspecific term, CVA (cerebrovascular accident), by many of our colleagues underscores the need for patients suspected of having a stroke or a transient ischemic attack (TIA) to be seen by vascular neurologists to determine why these events are happening. This, in turn, will yield answers to the questions of how to treat and prevent stroke.
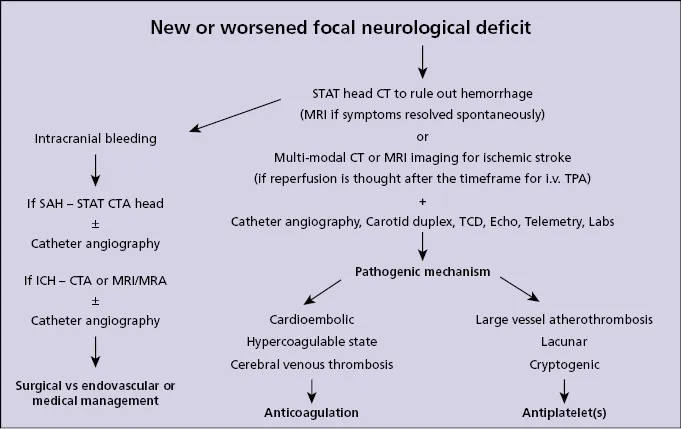
Our ability to diagnose the type of stroke (ischemic or hemorrhagic) relies solely on imaging, and patients with new symptoms suggestive of stroke should be granted emergency access to computed tomography (CT) and magnetic resonance imaging (MRI), depending on the clinical situation and resources available. Often both of these tests are done in sequence during their hospital stay or during observation/ outpatient diagnostic workup. Patients with stroke or TIA should also undergo several other tests. The reason is not only to see the parenchymal damage, if any, and tissue at risk of infarction but also to determine the pathogenic mechanism of the event because treatment options vary greatly (Figure 1.1). The focus of this book is the assessment of a stroke patient, linking the neurological findings with the evaluation of vessels, and, in turn, integrating these findings with parenchymal and perfusion imaging. This book will further explain how to obtain this information at the bedside, and how it can change patient management.
Figure 1.1 An overview of common sequences in the diagnostic workup and treatment options according to a specific pathogenic mechanism.
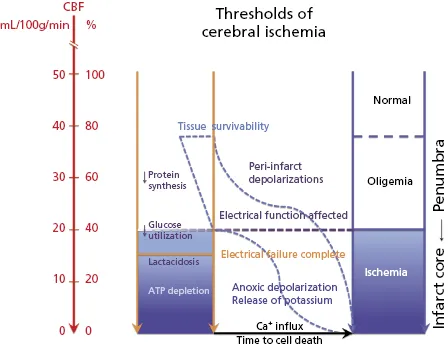
Lessons learned from cardiology and vascular medicine are invaluable for vascular neurology; however, these can only be applied to the brain vasculature to a certain extent. Unlike coronary vessels, the intracranial arteries are paper thin and cannot withstand too much mechanical or polypharmacological manipulations. They respond by vasodilation to a drop in blood pressure or volume in an attempt to maintain cerebral blood flow (CBF) as they also assure continuous diastolic flow, a feature of the low-resistance parenchymatous organs. When a patient develops stroke symptoms, this indicates that the blood flow to a specific area of the brain has dropped below the level that normally sustains neuronal function. Electrical function of neurons becomes affected at CBF falling below approximately 20 mL/100 g of brain tissue/min (Figure 1.2)[1–4]. Flattening of the electroencephalogram was seen in human subjects during endarterectomy when CBF was ≤19 mL/min [2]. The concept of ischemic penumbra emerged from studies correlating the neuronal electrical activity and CBF reduction thresholds [5]. It became clear that at certain CBF levels the neurons can remain structurally intact but functionally inactive. Without reperfusion treatment a further fall in CBF occurs, and the ischemic cascade may progress fast leading to influx of calcium and brain death. Further experimental research has focused on tissue viability thresholds [6, 7].
Figure 1.2 Neuronal dysfunction and levels of cerebral blood flow impairment. Two important concepts related to cerebral ischemia are schematically presented here. The decreasing levels of cerebral blood flow (CBF) due to occlusion or hypoperfusion can induce an oligemic state, subsequent electric cell dysfunction and failure, finally leading to cell death at very low CBF levels [1]. These thresholds of ischemia are hypothetically combined with the time to cell death and recoverability of tissue (dotted S-shape lines invoked from observations in reference [6]. The concepts arise from landmark studies of Austrup et al. [1] and Jones et al. [6].
The neurological symptom onset has been long equated with the timing of a thromboembolic occlusion. In reality, this is not correct [8]. Symptom onset is the time of the collateral or residual flow failure. This failure can occur shortly after an acute occlusion or it can develop over time. Furthermore, the time lapse between symptom onset and initiation of reperfusion therapy was further treated as a substitute for recoverability. In general, this time dependency is applicable to large groups of patients in clinical trials: patients' chances to recover completely double if fibrinolytic treatment with intravenous tissue plasminogen activator (tPA) starts at 2 hours from symptom onset, and these chances diminish rapidly over time [9]. The decision making for systemic tPA is fairly straight forward and within the first few hours it applies to the majority of patients regardless of the cause of cerebral ischemia. However, a closer look at an individual patient reveals that ischemic stroke is remarkably heterogeneous (Table 1.1). We will examine in turn different stroke types and what tests are suitable to ascertain these mechanisms, commonly referred to as the TOAST classification of stroke pathogenic mechanisms [10]. Stroke remains an extremely time-sensitive process and if therapeutic attempts to restore blood flow are not done in time, most patients will loose their battles with obstructive arterial lesions. Traditional time frames for reperfusion, however, have nothing to do with the severity of ischemia and its variable mechanisms. The question is what else besides systemic tPA can you offer as treatment? This depends on why stroke is happening, and this in turn leads to the choice of imaging modalities. Even the use of systemic thrombolytics could be better gauged by rapid multimodal imaging [8, 11]. The stress here must be on “rapid,” that is within minutes not half an hour to an hour to acquire imaging sequences.
Table 1.1 Main pathogenic types of ischemic stroke, or TOAST classification
Data from Adams et al. [10].
| Large-vessel atheromatous |
| ≥50% stenosis or occlusion with pre-existing atheromatous plaque in an artery feeding the territory of cerebral ischemia |
| Cardioembolic |
| Identification of a known risk factor or source for cerebral embolization from the heart, i.e. atrial fibrillation, intracardiac thrombus, etc. |
| Lacunar |
| A typical lesion affecting perforating vessels in subcortical areas or pons/ brainstem |
| Other |
| Arterial dissection, paradoxical embolism, hypercoagulable state, vasculitis, etc. |
| Cryptogenic |
| No pathogenic mechanism was identified upon adequate workup or two or more etiologies were found, i.e. cortical lesion unilateral to a severe carotid stenosis in a patient with known atrial fibrillation |
Our ability to understand stroke by imaging the brain with X rays and MRI is constantly evolving, and the majority of current and future stroke specialists spend a great deal of time learning how to base their decisions on multimodal CT or MRI imaging. They also become familiar with carotid duplex ultrasound, at least to order it as a screening test for carotid pathology of the neck. Far fewer take the time and effort to master ultrasound tests themselves, particularly transcranial Doppler (TCD). In my practice, I use all available tests when appropriate or feasible, as they provide complimentary information. Furthermore, I find reasons to treat (not excuses to withhold treatment), an approach opposite to minimalistic or nihilistic views as to what we can offer stroke patients. The latter results in under-utilizing imaging and vascular assessment, often resulting in patient receiving treatment that is not based on a pathogenic mechanism specific to their event.
The following case scenarios will show how we approach typical patient problems, what key questions we ask to begin patient management, and the complimentary use of diverse ultrasound tests for the neurological examination and the standard of care CT or MRI scanning. A brief case presentation is followed by questions and answers that illustrate the thought process and supportive facts. So, as we say at the beginning of stroke rotation, welcome to the (neurovascular) plumbing service!
Case study 1.1
A 62-year-old man, current smoker with otherwise unremarkable past medical history and no primary care doctor, is seen for an episode of weakness in the left arm that lasted for 10 min and resolved spontaneously. The National Institutes of Health Stroke Scale (NIHSS) score (Appendix 1.1) is 0. A noncontrast head CT done within 20 min of arrival to the hospital is normal. His BP is 153/70 mmHg, pulse regular. ABCD2 score (Tables 1.2 and 1.3) = 3 points [12].
Table 1.2 ABCD2 score
| Factor | Score |
|---|---|
| Age: ≥60 years | 1 |
| Blood pressure: ≥140/90 mmHg | 1 |
| Clinical features: | |
| Unilateral weakness | 2 |
| Speech impairment without weakness | 1 |
| Duration: | |
| ≥60 min | 2 |
| 10–59 min | 1 |
| Diabetes: Yes | 1 |
Table 1.3 Stroke risk within 2 days after TIA as predicted by the total ABCD2 score
| Risk | ABCD2 score (%) |
|---|---|
| Low | 0–3 (1.0) |
| Medium | 4–5 (4.1) |
| High | 6–7 (8.1) |
The ABCD2 score is predictive of the risk of stroke after TIA and is being used to stratify patients according to this risk [12]. However, it bears no information as to pathogenic mechanism of the TIA, and it has certain other limitations. It should not be used instead of multimodal imaging such as MRI because our definition of the TIA is based on imaging of the brain parenchyma and noncontrast CT scan is not sensitive to stroke for several hours after symptom onset, particularly with spontaneous early symptom resolution.
1. What is the diagnosis?
Likely a TIA (definition provided in Box 1.1[13]).
Likely a TIA (definition provided in Box 1.1[13]).
Box 1.1 Current definition of TIA
Transient ischemic attack (TIA): a trans...
Table of contents
- Cover
- Title page
- Copyright page
- Foreword
- Preface
- Acknowledgment
- Abbreviations
- 1: Understanding the Mechanisms and Dynamics of Cerebrovascular Events
- 2: Time Is Brain and Brain Is Flow!
- 3: The Power of Observation
- 4: Applied Principles of Ultrasound Physics
- 5: Applied Principles of Hemodynamics
- 6: Real-Time Ultrasound Measures
- 7: Emergent Examination
- 8: Diagnostic Waveforms and Algorithms
- 9: Differential Diagnosis
- 10: Integration of Information and Case-Based Problem Solving
- Index