- English
- ePUB (mobile friendly)
- Available on iOS & Android
Basic Guide to Orthodontic Dental Nursing
About this book
The Basic Guide to Orthodontic Dental Nursing is a must-have introduction for those seeking to develop their knowledge and understanding of this core area of clinical practice.
Written in a clear and accessible format, with colour illustration throughout, the book is a guide for all dental nurses with an interest in orthodontics. It is designed to reflect sections of the syllabus of the Certificate in Orthodontic Dental Nursing. Chapters cover such key topics as tooth eruption patterns, removable and fixed appliances, de-bonding, and retention. There are also sections on care prior to treatment, including the requirements for a first appointment, and there is helpful guidance on maintaining motivation – particularly for young patients and their parents.
Published in a compact format for portability and easy reference, this is a valuable addition to the Basic Guides series. Please note Figures 1.2 and 2.4 have now been corrected in the print edition and are available to purchase. All electronic versions have already been corrected.
Tools to learn more effectively

Saving Books

Keyword Search

Annotating Text

Listen to it instead
Information
Chapter 1
Definition of orthodontics and factors influencing orthodontic treatment
- orthos – meaning straight or proper
- odons – meaning teeth
- a malocclusion, if it affects teeth alignment and the bite relationship
- the bite is fully functioning and the patient can bite and chew properly
- the oral hygiene is made easier, thus helping to prevent caries and gingivitis
- the malocclusion does not cause other damage
- the patient looks better and has better self-esteem
- straighten teeth
- improve the bite
- improve the function
- improve oral hygiene (and make teeth easier to clean)
- improve self-esteem of the patient
CLASSIFICATION OF OCCLUSION
- incisor relationship
- buccal segment occlusion, left and right
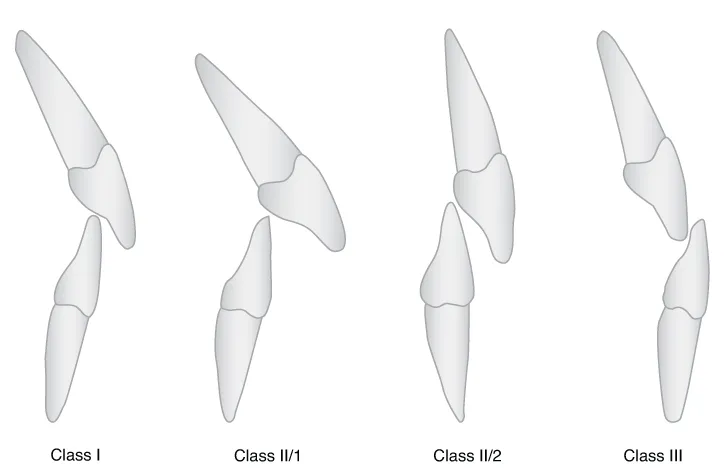
Incisor classification
- Classes have roman numerals, e.g. I, II, III
- Divisions do not, e.g. Class II/1 or Class II/2
- relates to the bite of the tip of the lower central incisors onto the back of the upper central incisors
- is divided into three horizontal sections and where the lower incisor occludes will determine the classification
Class I
- The incisal edge of the lower incisors bites on or below the cingulum plateau of the upper incisors
Class II/1
- The upper incisors are proclined or upright (Figures 1.3 and 1.4)
- The lower incisors bite behind the cingulum plateau of the upper incisors
- The position of these front teeth means they can be damaged more easily because of their vulnerable position

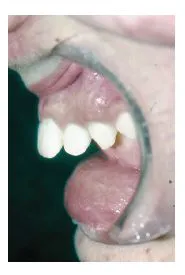

Class II/2
- The upper incisors are retroclined
- The lower incisors bite behind the cingulum plateau
- The position of the teeth can, when closed, lead to trauma to the lower labial gingivae and the upper palatal gingivae (Figures 1.5-1.7)


Class III
- The bite is edge to edge or reversed
- The incisal edge of the upper incisors can bite into the back (lingual) surface of the lower incisor (Figure 1.8)
- A horizontal overlap is called overjet
- A vertical overlap is called overbite
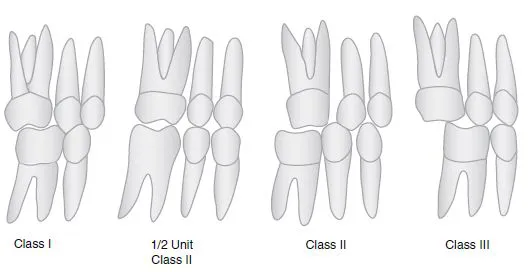
Buccal segment occlusion
- was devised by Edward Angle in 1890
- is still widely used today
- is based on the occlusion between the first permanent molar teeth, which erupt when the patient is about 6 years old
- Class I – This is as near to the correct relationship as you see
- Class II – This is at least half a cusp width behind the ideal relationship
- Class III – This is at least half a cusp width in front of the ideal relationship
THE MIXED DENTITION
- Age 6
- 1/1 lower central incisors
- 6/6 lower first molars
- 6/6 upper first molars

- Age 7
- 1/1 upper central incisors
- 2/2 lower lateral incisors
- Age 8
- 2/2 upper lateral incisors
- Age 11
- 3/3 lower canines (cuspids)
- 4/4 lower first premolars (bicuspids)
- 4/4 upper first premolars (bicuspids)
- Age 12
- 3/3 upper canines (cuspids)
- 5/5 lower second premolars (bicuspids)
- 5/5 upper second premolars (bicuspids)
- 7/7 upper second molars
- 7/7 lower second molars
- Age 18–25
- 8/8 upper third molars (wisdom teeth)
- 8/8 lower third molars (wisdom teeth)
- some deciduous teeth
- some permanent teeth
- some teeth yet to erupt
INDICATIONS FOR TREATMENT
- are overcrowded
- may have erupted out of position
- are protruding – Class II/1
- are in a reverse bite
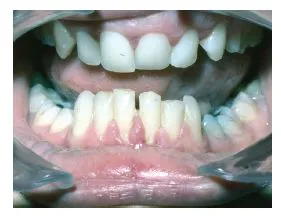
- are in a self-damaging bite (Figure 1.11)
- are spaced
- are absent – hypodontia
- are damaged


- with only very small irregularities
- where the tooth position does not compromise oral hygiene
- which does not interfere with function, e.g. biting off food, eating
- with overcrowded, protruding teeth
- with rotated teeth which make oral hygiene difficult and cause problems with caries (Figure 1.12)
- which visually deviate from average, e.g. a reverse bite
- which look unattractive and affect the smile
- which seriously affect function, e.g. makes chewing food difficult
UNDERLYING CAUSES OF MALOCCLUSION OF THE TEETH
- underlying skeletal abnormalities
- facial asymmetries
- hereditary (run in families, e.g. tendency to be Class III)
- a result of injury
- a result of illness affecting facial or skeletal growth
- a result of a syndrome or cleft
MULTI-DISCIPLINARY APPROACH
- restorative (e.g. hypodontia patients needing implants/bridges or microdontia patients needing veneers or crowns)
- surgical (e.g. patients needing an osteotomy)
- cleft (e.g. patients needing alveolar bone grafting)
Table of contents
- Cover
- Title page
- Copyright
- Dedication
- Foreword
- How to use this book
- Acknowledgements
- Chapter 1: Definition of orthodontics and factors influencing orthodontic treatment
- Chapter 2: The first appointment
- Chapter 3: Occlusal indices
- Chapter 4: Motivation
- Chapter 5: Leaflets
- Chapter 6: Oral hygiene
- Chapter 7: Removable appliances
- Chapter 8: Transpalatal arches, lingual arches and quad helix
- Chapter 9: Rapid maxillary expansion
- Chapter 10: Extra-oral traction and extra-oral anchorage
- Chapter 11: Functional appliances
- Chapter 12: Temporary anchorage devices
- Chapter 13: Fixed appliances – what they do and what is used
- Chapter 14: Fixed appliances–direct bonding
- Chapter 15: Fixed appliances – indirect bonding and lingual orthodontics
- Chapter 16: Ectopic canines
- Chapter 17: Debonding
- Chapter 18: Retention and retainers
- Chapter 19: Aligners
- Chapter 20: Multi-disciplinary orthodontics
- Chapter 21: Adult orthodontics
- Chapter 22: Mandibular advancement devices
- Chapter 23: Model box storage and study models
- Chapter 24: Descriptions and photographs of most commonly used instruments and auxiliaries
- Chapter 25: Certificate in Orthodontic Nursing and extended duties
- Chapter 26: Orthodontic therapists
- Chapter 27: Professional groups for orthodontic dental nurses
- Useful contacts
- Glossary of terms
- Index
- End User License Agreement
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app