![]()
Part One
Conflict
![]()
Chapter 1
Why Conflict?
When your work is health care, your daily routine requires constant negotiation and involves some measure of conflict. Decisions affecting a number of people have to be made. Competing priorities have to be balanced. There is the pressure of time and the need for constant vigilance that the job is done correctly.
Health care work is accomplished via an intricately structured and constantly evolving set of relationships. Formal and informal rules determine who speaks to whom, who makes what decisions, who has and who does not have what information. People are organized and decisions are aligned in a cautiously defined order. The most important or momentous information, person, or decision gets the uppermost attention, and the rest trails behind. This sequence is intended to yield systematic and value-based decision making.
Most important, the work is done by people and for people. There is perhaps no endeavor more intimately tied to who you are, your identity, than the duties you perform or the care you receive through the health system. Health care is on the cusp of life and death and the quality of life. Whether you are in the role of patient, provider, or manager, your values, beliefs, and personality are exposed and interlocked with the values, beliefs, and personalities of others amid the interpersonal proximity of health care decision making, negotiation, and conflict. And if your role is in the realm of health policy, service regulation, or finance—far removed from the immediate point of care or population served—values, beliefs, and personality remain just as important even though the impact may appear far more abstract. What you do affects how—and sometimes even whether—others live.
What if this complex puzzle does not smoothly fit together? What if there are differences about what or who is more important? What if a mistake occurs? What if there is a clash of personalities among people who must closely interrelate? What if there is dissonance between the policies and procedures and the people who inhabit these relationships? What if various professionals are working under different incentives? How will this affect what you do and how you do it?
Consider the following scenario.
It is another hectic night in the emergency department of Oppidania Medical Center. A frenzy of activity centers at the desk, where nurses, residents, attending physicians, and emergency medical technicians gather to exchange information, tell stories, and take a rare break.
Nearby, Artie Ashwood, a twenty-four-year-old graduate student, moans in one of the beds. The monitors and machines surrounding him are beeping, flashing, and filling him with life-saving fluids. He has an enlarged heart, arrhythmia, and shortness of breath. It has been three hours since he came in, and it is time to decide where he should go next. In the visitor's room, his mother, Anna Ashwood, and girlfriend, Cindy Carrington, nervously await news of his condition.
The attending physician, Dr. Beatrice Benson, oversees the work of the medical residents. On crazy busy nights, she sometimes has to remind herself, “The emergency department is for triage—not treatment.” She has to remember that their job is to assess the patient and decide the next step. If the problem is life threatening, they admit to intensive care. If the patient doesn't need to be in the hospital, they discharge with a treatment plan and instructions. If the problem is someplace in between, then they admit for observation and treatment. So, if it's an admission, the question is to which service?
A small cluster of staff have gathered to discuss Ashwood's condition. It defies a conclusive diagnosis: his young age is a concern. His symptoms could signal a dangerous situation. Hoping for more information, they hold him in the emergency department, waiting for stabilization. Nurses and residents are constantly monitoring his condition, but nothing changes.
Suddenly, Charlotte Chung, the triage nurse at the desk, announces the impending arrival of a patient with multiple gunshot wounds. The door to the specially equipped trauma room opens, and the staff move to their places around the gurney that will hold the seriously injured man.
Benson talks by telephone with the paramedics in the ambulance to assess the incoming patient's condition and prepare for briefing the staff. As she turns toward the trauma room, Chung suggests that the young man with the enlarged heart be admitted to one of the floors in the hospital, because it is looking like a busy night.
Preoccupied, Benson says, “Good idea,” and walks off with no further instruction. Chung snaps a pencil in two as she watches Benson head toward the incoming patient.
There are, so far, three people in our story. Artie Ashwood's fate is in the hands of the people who surround him. He is in great pain. He is frightened. He does not know what is happening to him and what it might mean for the rest of his life. People are asking him questions, many of them repetitive. Some of those who speak to him seem genuinely concerned about how he is doing. Others seem to be asking rote questions from a prescribed list. He is afraid of being lost in this loud mass of people. He overhears that a gunshot victim is on the way. Might the hospital explode in shots if the attackers come here to finish the job? Even more frightening, might the nurses and doctors who have been at his side forget him once someone sicker arrives? He has been waiting for a long time. Can't they just fix him up and move him along already? He is intimately dependent on people who now seem otherwise occupied.
As the attending physician in the emergency department (ED), Dr. Benson oversees and has responsibility for the work of the ED medical residents and physicians. She simultaneously tends to many constituencies and concerns and is interdependent with many parts of the system. She is vigilant on behalf of the patients, watchful over the residents, and in touch with others in distant departments. When she asks, “Is intensive care backed up?” she hears a variety of answers: “Yes, we can accept a patient severely cut in an accident at work.” “No, we are not taking a nine-months-pregnant, cocaine-addicted woman being dumped by a suburban hospital.” By its very nature, her work is in the short term: her responsibility is to keep the flow of patients moving. She sees patients for a matter of hours before they disappear into the labyrinth of the hospital or out to discharge. She rarely sees them again. The long term is an abstraction. She has some power and influence, though others in the hospital understate the authority she believes is hers. There is, however, no underestimating when it comes to responsibility. For a miscalculation, the attorneys will chase Dr. Benson with their lawsuits, the administrators will challenge her wastefulness, and the patients will complain about their delayed or inadequate care. She is constantly negotiating and continually trying to keep the many parts of the system in balance.
Ostensibly, as the triage nurse in the ED, Charlotte Chung has the role of screening patients and determining the severity and urgency of their conditions. In fact her function is to create order among the unpredictable and sometimes chaotic flow of patients arriving at the ED. That order must align with the contingent of nurses, physicians, and other personnel staffing the shift. It is a matter of creating a fluid balance. Patients arrive at the hospital in pain or discomfort and are all anxious to be seen at once. Family or friends who accompany them advocate, question, and worry. It is up to her to decide who will be seen when, by whom, and where: she holds the criteria and judges each case accordingly. Physicians, nurses, technicians, and housekeeping personnel scurry to keep up the pace, caring for one patient and preparing for the next. They depend on Chung to make the right calls, to hold off patients who cannot yet be seen, and when the staff are overloaded, to focus on only the most severely ill. Her desk is like a lightning rod for conflict. She mediates among the needs of patients, the capacity of the staff, and the personalities who may explode under the pressure and stress of the decisions she is required to make. Her greatest sources of irritation are the obstacles erected by those, especially physicians, who hold greater authority but who carry far less perspective and understanding than she does.
Each of these people is part of the same reality, yet their perspectives are very different. The question is whether their distinct responsibilities, concerns, and decisions can combine in a congruent manner, allowing each to satisfactorily achieve his or her reason for being in the ED this night. If they can, the interaction will be productive and mutually beneficial. If they cannot, friction is inevitable. Conflict often has its roots in common experiences seen from different perspectives and with expectations that are seemingly at odds.
Different Purposes
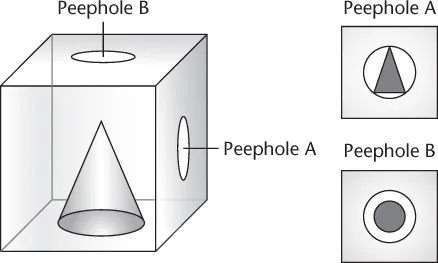
The complexity of health care interaction and decision making can be illustrated by the simple analogy of the cone in the cube (Figure 1.1). Two people peer into different holes in an otherwise opaque cube. Their task is to determine what is inside. The person peering into peephole A, on the side of the cube, sees a circle. The person peering into peephole B, on the top of the cube, sees a triangle. They are both viewing the same shape but from very different perspectives.
The person peering into peephole A points to his extensive education and expertise, declaring, “Do you realize how smart I am? If I say it's a triangle, then it's a triangle!” The person peering into peephole B counters, “I don't care how smart you think you are. I control the budget in this institution. If I say it's a circle, it's a circle!” Although this analogy is simple, it is emblematic of the failure to account for the multiple dimensions of a problem. Whether those involved are physician and nurse, patient and clinician, or administrator and payer, there are myriad ways for people to get mired in different perspectives and positions on the same problem. Achieving an integrated perspective is at the heart of the health care negotiation and conflict resolution process.
We often begin our health care negotiation and conflict resolution course with a classic game theory simulation exercise called Prisoners' Dilemma. (For a discussion of Prisoner's Dilemma and game theory, see Luce & Raiffa, 1957; Goldberg, Green, & Sander, 1987; Rahim, 1992.) This exercise demonstrates the difficulty of negotiating when people have little opportunity for direct or prolonged interaction, like prisoners in different cells trying to communicate. Each participant in the exercise is part of a foursome divided into two pairs. The two pairs sit with their backs to each other—which intentionally limits any direct interaction between the pairs—and an instructor moves messages on paper between them. In a series of transactions, they exchange X's and Y's, which when combined could translate into either gains or losses for each of the two sides.
To simulate conditions in real organizations, the directions for the exercise are purposefully ambiguous. One line in the directions encourages the participants to “do the best you can to achieve a high level of benefit from the transactions.” The unspoken quandary is that the high level of benefit is intentionally left open to interpretation. Because they must begin negotiating immediately, the players often do not have a common definition for what they are trying to achieve. As a result, one of the four players may assume that winning means his pair receives more points than the other pair. Another player may conclude that winning requires collecting more points while also reducing the other side's points. A third may assume that winning means each team receives an equal score. And finally, the fourth may surmise that winning means both teams get a score close to zero.
The problem is readily apparent. If each player assumes a different interpretation of high level of benefit, there is certain to be conflict. In essence, one person is playing one game, defeat the opponent, while his or her partner is playing another game, let's all win together.
Even among the most subdued of players, the interchange becomes eagerly animated. At face value they are only exchanging X's and Y's—symbols with no inherent value. The heated exchanges emerge from the underlying belief systems, perspectives, and objectives that influence the players' actions during the game. Each person is playing, in part, to advance and validate his or her own belief system. It is common for someone to say during the after-exercise debriefing, “It wasn't that I was going for points. I was trying to show that we can play to win together.” It is also common to hear, “I love to win, no matter what I am doing.” Each party strives to justify the principles that frame his or her behavior.
The cone in the cube problem and Prisoner's Dilemma parallel the situation in the ED: different perspectives on the same problem combined with differing objectives, a recipe for a high level of consequences and emotional conflict.
Artie Ashwood stares up at the tiles of the hospital ceiling. He is in a great deal of pain. He is frightened. He wants his computer. Then he could go online and get answers for himself about what is happening to his body. They won't even let him use his smart phone, which would let him turn to his online social networks for help. He hopes that the people around him will care for him well. His confidence in the system is flagging.
Ashwood's condition continues to defy a conclusive diagnosis. Hoping for more information, Dr. Dave Donley, the resident who has been following Ashwood, holds him in the emergency department, waiting for the stabilization. Nothing changes.
Her earlier suggestion to move Ashwood still unheeded, Charlotte Chung signals Dr. Benson over to the triage desk and asks if anyone might be ready to move along. The waiting room is full, and the gunshot wound is stretching everyone thin. Perhaps if Benson decides on her own, things will start happening. This is a nursing maneuver Chung learned a long time ago. Turn your problem into someone else's and then hand her your solution. When she chooses it, congratulate her wise decision. She dislikes having to play this game but smiles to herself every time it works.
Benson nods and shifts into command mode. She calls over to Dr. Donley, “We're too busy to hold this fellow any longer. Call cardiac intensive care and tell them we've got an admission. Tell them he needs to go up there right away.”
It has been a busy shift on the cardiac intensive care unit (CICU) as well. Seven of the CICU's eight beds are filled. Six of these patients require heavy-duty care. The seventh patient had been sent up by the ED three hours ago, and once the CICU nurses and physicians completed the workup and admission, it was clear that the ED had misjudged that patient: it was not a case requiring intensive care. The CICU had had enough of the ED for one night. With three hours left in the shift, the CICU staff were hoping the night would calm down.
The chief resident of the CICU, Dr. Eli Ewing, knows that he is running an expensive unit. That misjudged patient not only consumed a great deal of unnecessary time and work, it also cost the hospital and some insurer a lot of money. Ewing believes he has a responsibility to screen out patients who do not require this most technical level of care. Ewing also has a responsibility to the staff. In the parlance of the teaching hospital, a wall is a resident who succeeds in keeping out admissions to the unit. A sieve is someone who doesn't know how to say no. Walls are heroic, sieves are not—and Ewing is clear about which he prefers to be.
Ewing takes the call from Donley. Still smarting from the last case, Ewing listens sardonically to the report on Ashwood's enlarged heart. Donley admits he is not certain that the patient is in a medical crisis. Ewing's reaction is terse: the patient doesn't need to be admitted to the CICU and the unit is not going to take him. He suggests calling one of the general medical floors, which can do a far better and far less expensive job of babysitting. Ending the call abruptly, Ewing turns to the CICU staff and smiles, “Anoth...