![]()
Chapter 1
Introduction
Judi Edmans, Fiona Coupar and Adam Gordon
This chapter includes:
- Definition, impact, symptoms, causes, classification of stroke
- International Classification of Functioning, Disability and Health (ICF) Medical investigations
- Secondary prevention Neuroanatomy
- Damage to different areas of brain
- Policy documents: strategies and guidelines Self-evaluation questions
Stroke is a complex condition where the knowledge base is continuously increasing. There are constant advances in the understanding of the condition, assessment and intervention techniques. Occupational therapists are a vital component in the rehabilitation of patients with this condition. It is vital that they understand the condition itself and the theoretical basis for intervention.
Definition of stroke
The World Health Organization (WHO) defines stroke as ‘a clinical syndrome, of presumed vascular origin, typified by rapidly developing signs of focal or global disturbance of cerebral functions lasting more than 24 hours or leading to death’ (WHO, 1978).
Impact of stroke
Stroke is a major public health care concern and has a significant impact on individuals, their families and wider society. Within the UK, an estimated 150,000 people have a stroke each year (Office of National Statistics, 2001). Stroke is the third most common cause of death, after heart disease and cancer, with over 67,000 deaths each year (British Heart Foundation, 2005). However, the most significant and lasting impact of stroke is long-term disability. Stroke is the single, greatest cause of complex and severe adult disability in the UK (Wolfe, 2000; Adamson et al., 2004). A third of people who have a stroke will have some long-term disability (National Audit Office (NAO), 2005). Common problems following stroke include aphasia, physical disability, loss of cognitive and communication skills, depression and other mental health problems.
In addition to the individual impact, stroke places a significant burden on health and social services. In England alone, stroke costs the National Health Service (NHS) and the economy about £7 billion a year: £2.8 billion in direct costs to the NHS, £2.4 billion of informal care costs (e.g. the costs of home nursing borne by patients’ families) and £1.8 billion in income lost to productivity and disability (NAO, 2005). Unfortunately, outcomes in the UK compare poorly internationally, despite our services being among the most expensive, with unnecessarily long lengths of stay and high levels of avoidable disability and mortality (Leal et al., 2006).
Symptoms of stroke
The initial symptoms of stroke are (Warlow et al., 2008):
- Sudden weakness or numbness of the face, arm or leg on one side of the body.
- Sudden loss or blurring of vision in one or both eyes.
- Sudden difficulty speaking or understanding spoken language.
- Sudden confusion.
- Sudden or severe headache with no apparent cause.
- Dizziness, unsteadiness or a sudden fall, especially with any of the other signs.
However, there are more specific symptoms that will become apparent to the patient, family, medical and rehabilitation staff over the following weeks, months and years. These may include a variety of abnormalities, which will be described further in later chapters.
Face-Arm-Speech Test
The National Stroke Strategy for England (Department of Health (DH), 2007) highlighted the need to improve public awareness of stroke and the recognition of signs of a stroke, resulting in the ‘FAST’ acronym being developed by the Stroke Association in partnership with other stroke organisations and experts.
The awareness campaign highlights that stroke is a medical emergency and time is essential to protect the brain from excess damage. Therefore, it is essential for people to recognise the symptoms of stroke and act ‘FAST’ when these are present. The ‘FAST’ acronym represents:
Facial weakness – Can the person smile? Has his or her mouth or eyes drooped?
Arm weakness – Can the person raise both arms?
Speech problems – Can the person speak clearly and understand what you say?
Time to call 999.
Anyone exhibiting any of these signs should be treated as an emergency with 999 being called to get the patient to hospital as quickly as possible, to receive the treatment they need.
FAST was around before the stroke strategy, although ‘T’ stood for ‘Test all three’ rather than ‘Time to call 999’ (Mohd Nor et al., 2004).
Causes of stroke
The main causes of stroke are as follows.
Ischaemia leading to infarction
This describes impairment of blood supply to part of the brain, resulting initially in dysfunction and then tissue death (infarction). The causes of cerebral infarct are classified according to the TOAST (Trial of Org 10172 in Acute Stroke Treatment) (Adams et al., 1993) classification as:
- Large artery occlusion (usually carotid or middle cerebral artery occluded by thrombus or embolism).
- Cardioembolism (clot from the heart, most commonly the atrial appendages, migrating to the cerebral arteries, causing blockage and stroke).
- Small vessel occlusion (thrombus or embolism in the smaller cerebral arteries, causing a lacunar infarct).
- Other aetiologies (e.g. generalised brain underperfusion, causing infarcts in the watershed territories).
Haemorrhage
This is usually intracerebral haemorrhage (i.e. within the body of the brain) but can be subarachnoid haemorrhage (i.e. between the arachnoid mater and the brain). Intracerebral haemorrhages are commonly caused by hypertension-related changes in the small intracerebral arteries but can, less commonly, be caused by aneurysms (outpouchings of the arterial wall) or arteriovenous malformations (abnormal communications between arteries and veins).
Transient ischaemic attack
Transient ischaemic attack (TIA) is a term used to describe symptoms of stroke, resolving within 24 hours. This does not represent a completed stroke but is, instead, caused by transient impairment of tissue blood supply (ischaemia) with subsequent resolution. These patients are at high risk of proceeding to completed stroke and should be seen by a physician as an emergency, ideally within 24 hours of presentation (Intercollegiate Stroke Working Party (ISWP), 2008).
Classification of stroke
Bamford et al. (1991) described a classification of cerebral infarction to help clinicians identify the part of the brain affected. This classification is based on the signs and symptoms that patients experience and is now widely used. It is useful because it correlates to prognosis. Thus, based on a bedside examination, a clinician can make predictions about survival and long-term dependency in order to inform management decisions and discussions with patients/relatives.
The Bamford (or Oxford) classification is as follows:
Total anterior circulation stroke (TACS)
All of the following:
– Motor/sensory deficit affecting greater than two-thirds of face/arm/leg.
– Homonymous hemianopia.
– New disturbance of higher cortical function.
Partial anterior circulation stroke (PACS)
– Any two of the components of a TACS.
– Or isolated disturbance of higher cortical function.
– Or limited motor/sensory dysfunction (affecting a single limb or the face alone).
Posterior circulation infarction (POCI)
Any of:
– Cranial nerve palsy and contralateral motor/sensory deficit.
– Bilateral motor/sensory deficit.
– Conjugate eye movement problems.
– Cerebellar dysfunction.
– Isolated homonymous hemianopia.
Lacunar infarction (LACI)
Greater than two-thirds of arm/face/leg affected by:
– Pure motor stroke.
– Or pure sensory stroke.
– Or pure sensorimotor stroke.
– Or ataxic hemiparesis.
Disorders of higher cortical dysfunction commonly include aphasia, decreased level of consciousness, neglect syndromes, apraxia and agnosia syndromes.
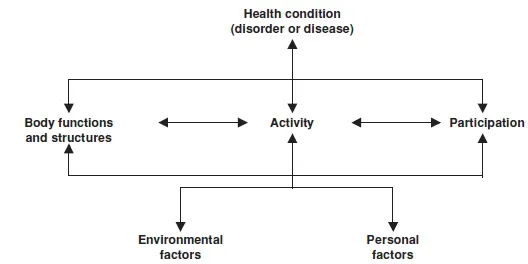
International Classification of Functioning, Disability and Health
The International Classification of Functioning, Disability and Health (ICF) (WHO, 2002) was produced by the WHO to replace the International Classification of Impairments, Disabilities and Handicaps. The ICF is not used exclusively in stroke; however, stroke patients often present with complex impairments which are a challenge for rehabilitation teams. The ICF provides a means of understanding and describing health status. It takes account of impairments of body structure and function and how these interact with personal and environmental factors to affect patient’s activities and participation in the wider world. Figure 1.1 illustrates the interactions between different aspects of the ICF.
The domains of the ICF are as follows:
Body functions: physiological functions of body systems (including psychological functions), for example, mental, neuromusculoskeletal and movement-related functions
Body structures: anatomical parts of the body such as organs, limbs and their components, for example, nervous system structures and structures related to movements Impairments (of body function and structure): abnormal body functions and structures such as a significant deviation or loss, for example, hemiparesis following stroke Activity: execution of a task or action by an individual, for example, dressing Activity limitations: difficulties an individual may have in executing activities, for example being unable to dress due to hemiplegia
Participation: involvement in a life situation, for example, attending a social gathering Participation restrictions: problems an individual may experience in involvement in life situations due to the activity limitation, for example, being unable to visit family and friends due to difficulty dressing
Environmental factors: physical, social and attitudinal environment in which people live and conduct their lives, for example, legal and social structures, architectural characteristics, coping styles, social background and experiences Personal factors: factors unique to the patient, which impact upon their health status, for example, personality and attitudes.
In ICF the term functioning refers to all body functions, activities and participation, while disability is similarly an umbrella term for impairments, activity limitation and participation restrictions.
Medical investigations following stroke and TIA
Medical investigations following stroke and TIA are performed to:
- Confirm the diagnosis of stroke.
- Determine the site and type of stroke.
- Establish the cause(s) of the stroke.
- Guide treatment to prevent further strokes.
Computerised tomography or magnetic resonance imaging
Imaging (either computerised tomography (CT) or magnetic resonance imaging (MRI)) helps to establish the pathological diagnosis by detecting either cerebral infarction or haemorrhage. The distinction between haemorrhage and infarction is important as treatment with aspirin or anticoagulants is likely to be indicated for cerebral infarction but would be contraindicated in cerebral haemorrhage. A CT scan should therefore be performed on all patients within 24 hours of a stroke (ISWP, 2008).
It is also useful for excluding other intracranial pathologies that mimic stroke, for example, tumours or subdural haematomas. Practice varies with regard to routine scanning of TIAs; it is, however, increasingly common for physicians to perform a CT scan on these patients, particularly if there is some concern that the history is long, or atypical.
ModernCTscannerscandetectabnormalitieswithinafewhoursofalargearterystroke; however, smaller infarcts can be difficult to detect if scanned early. Another difficulty can arise when identifying a new acute l...