![]()
Part 1
The ECG in Clinical Practice
![]()
Chapter 1
What are the clinical applications of the ECG in emergency and critical care?
Rajan A.G. Patel, Christopher M. Rembold
University of Virginia, Charlottesville, VA, USA
Case presentations
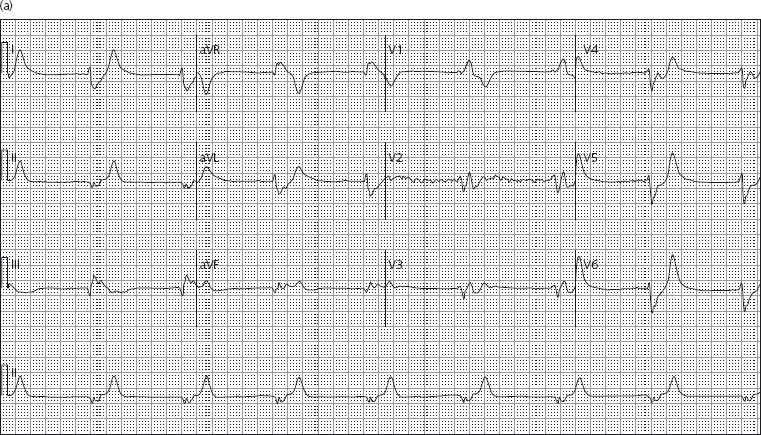
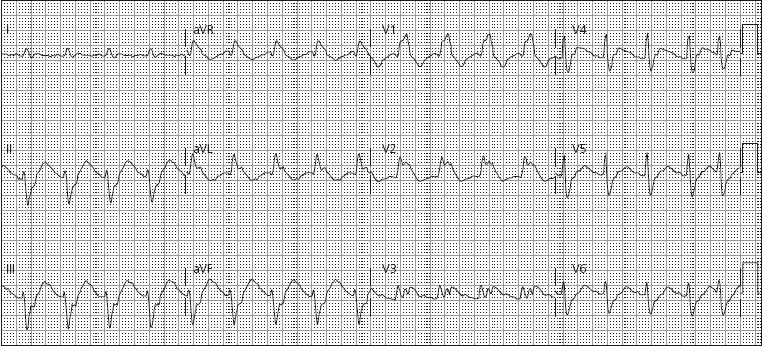
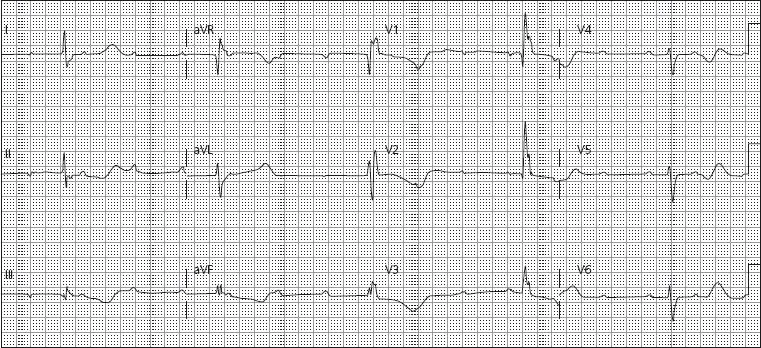
Case 1: A 56-year-old man with a history of hypertension and chronic kidney disease is brought to the emergency department (ED) by his wife, with a chief complaint of progressive lethargy and fatigue over several days. On physical exam the patient appears ill. His blood pressure is 90/50 mmHg. The electrocardiogram (ECG) (Figure 1.1a) demonstrates a regular wide complex QRS rhythm with a right bundle branch-like morphology. The QRS complex is not preceded by P waves and occurs at a rate of approximately 48 beats per minute (bpm). The emergency physician initiates appropriate treatment based upon the electrocardiographic findings; laboratory findings confirmed the diagnosis. Four hours later, the ECG (Figure 1.1b) demonstrates sinus tachycardia at a rate of 103 bpm. Note that the P waves have returned and the QRS complex is now narrow.
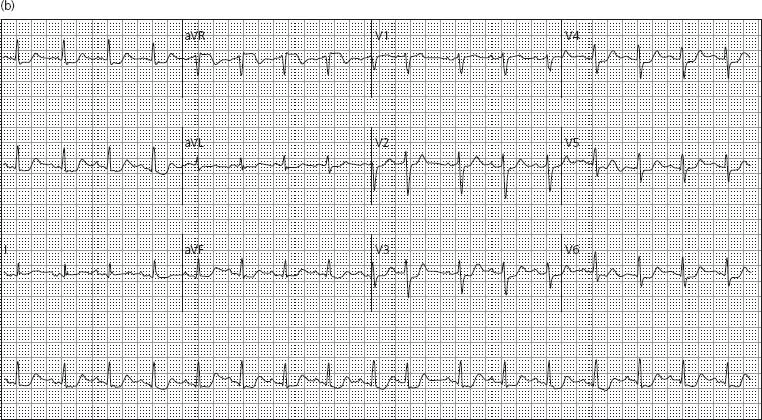
Case 2: A 24-year-old graduate student is brought to the ED after calling 911 stating that she overdosed on her anti-depressant medication. She is alert, crying, and complains of a dry mouth. Her initial heart rate is 96 bpm with a blood pressure of 120/80 mmHg. Her examination is remarkable for dilated pupils, flushed skin, and occasional twitching of muscles in her arms and legs. The baseline ECG demonstrates sinus rhythm with a markedly prolonged QT interval. The patient suddenly becomes lethargic and a 12-lead ECG (Figure 1.2) prompts the emergency physician to consider urgent therapy.
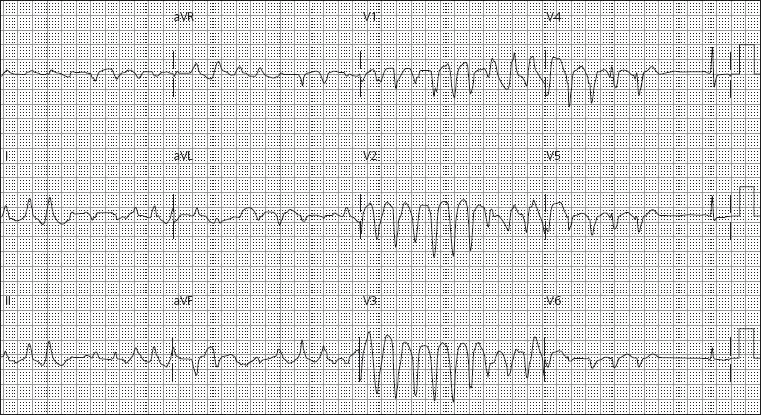
Case 3: A 59-year-old woman with a history of diabetes, hypertension and hyperlipidemia is brought to the ED having experienced increased difficulty breathing and neck discomfort. On physical examination, the patient is tachypneic with a respiratory rate of 30 breaths per minute. Her heart rate is 106 bpm with a blood pressure of 100/60 mmHg. An ECG (Figure 1.3) is obtained. The patient is emergently taken to the cardiac catheterization lab for primary percutaneous coronary intervention (PCI). Repeat ECG after the procedure demonstrates resolution of all electrocardiographic abnormalities.
Case 4: A 74-year-old woman with a history of tobacco use, hypertension, and hyperlipidemia presents with nausea and an episode of syncope. The initial ECG (Figure 1.4) in the ED shows sinus tachycardia and an inferior ST elevation myocardial infarction (STEMI). She presented 4 hours after the onset of symptoms. The cardiac catheterization laboratory is activated to perform primary PCI. Prior to transfer, the patient suddenly becomes diaphoretic and lethargic. Her heart rate decreases to 30 bpm and her blood pressure is 70/50 mmHg. The patient is treated promptly with intravenous atropine, and the sinus tachycardia returns.
Clinical applications of the ECG
Electrocardiography is performed widely throughout emergency and critical care medicine. In fact, some form of electrocardiographic monitoring is one of the most widely applied diagnostic tests in clinical medicine today – including both single- and multiple-lead analysis as well as the 12-lead ECG. The ECG can assist in establishing a diagnosis, ruling-out various ailments, guiding the diagnostic and management strategies in the evaluation, providing indication for certain therapies, determining inpatient disposition location, and assessing end-organ impact of a syndrome. In the ED environment, the ECG less often provides a specific diagnosis.
Metabolic abnormalities: The surface 12-lead ECG is a reflection of the changes in the transmembrane potential of cardiac myocytes that occur with atrial and ventricular depolarization and repolarization. The transmembrane potential is the electrical gradient from the interior to the exterior of cardiac myocytes. This gradient results from differences in the extracellular and intracellular concentrations of specific anions and cations as determined by the Nernst equation. The cations that contribute significantly to the creation or maintenance of this gradient include potassium, sodium, calcium, and magnesium. As such, shifts in the extracellular or plasma concentrations of these cations may result in changes in the surface ECG. These changes are readily appreciated when the baseline ECG is completely normal. However, abnormalities from infarction/ischemia can make changes from electrolyte shifts more difficult to appreciate. In critically ill patients, two or more electrolyte abnormalities may co-exist, resulting in several changes in the ECG, some of which may mask each other.
Hyperkalemia: The electrocardiographic hallmarks of moderate hyperkalemia are symmetric, tall, peaked T waves and low amplitude P waves. Severe hyperkalemia produces a widened QRS complex without P waves. The electrocardiographic changes associated with hyperkalemia are a reflection of changes in the depolarization/repolarization waveform of the cardiac myocytes. One of the first changes observed on the surface ECG when the extracellular potassium ion concentration increases above 6.0 mM is narrow, peaked, tall T waves. This phenomenon occurs because repolarization of the ventricles occurs more synchronously [1]. As the extracellular potassium ion concentration increases further (6.5–8.0 mM), the resting membrane potential of the cardiac myocytes depolarizes, resulting in a slower conduction velocity. Slow depolarization across the atria is appreciated on the surface ECG as prolonged P wave duration with low amplitude. The HV interval also increases further, contributing to the lengthening of the PR interval. Slow depolarization across the ventricles results in prolongation of the QRS complex. If the extracellular potassium ion concentration increases beyond 8.0 mM, then the P wave may be visible for longer on the surface ECG. In canine models of hyperkalemia, once SA node block occurs, action potential propagation from the atrial pacemaker site to the ventricles may occur via atrianodal pathways [2]. At high extracellular potassium ion concentrations, the QRS complex may resemble a left bundle branch-like or right bundle branch-like waveform. With further increases in extracellular potassium ion concentration, activation of multiple pacemaker foci may result in an irregular rhythm. The QRS complex may become so wide that it takes on the appearance of a sine wave. An explanation of this phenomenon is that cardiac myocytes in one area of the ventricle may repolarize before the action potential wavefront has traversed and depolarized the more distant cardiac myocytes. Once the plasma potassium ion concentration rises to 12–14 mM, ventricular fibrillation and asystole may occur [3]. This phenomenon is exploited during on-pump cardiac surgery by bathing or perfusing the heart with a cardioplegia solution.
Hypokalemia: The electrocardiographic hallmarks of hypokalemia are a prominent U wave and prolongation of the QT(U) interval. With profound hypokalemia or with hypokalemia in the presence of cardiac toxic medications, torsade de pointes may be precipitated. As with hyper-kalemia, the electrocardiographic changes associated with hypokalemia can be correlated with changes in the cardiac myocyte action potential waveform. Because the changes observed with hypokalemia affect the QT(U) portion of the ECG, it is changes in the ventricular action potential waveform that provide insight into the surface electrocardiographic changes. Hypokalemia results in prolongation of phase 3 repolarization. As the extracellular potassium ion concentration drops, the U wave amplitude increases and the T wave amplitude decreases. With a further decrease in potassium ion concentration, the U wave may begin to fuse with the preceding T wave. Hypokalemia can also result in increased arrhythmia. Davidson and Surawicz reported that the incidence of ectopic complexes was three times higher among patients who had a potassium ion concentration of ≤ 3.2 mEQ/L than control subjects [4]. Paroxsymal atrial tachycardia with block can also be observed in patients with hypokalemia. Severe hypokalemia can also precipitate ventricular tachycardia (VT), ventricular fibrillation (VF), or torsade de pointes [5]. Important non-cardiac manifestations of severe hypokalemia include rhabdomyocytis, metabolic alkalosis, and ascending paralysis.
Hypercalcemia: During phase 2 depolarization of the cardiac myocyte action potential, calcium slowly enters the cell. The duration of phase 2 correlates directly with the duration of the ST segment [6]. When the extracellular calcium ion concentration is elevated, phase 2 occurs relatively rapidly, producing a short ST segment [7]. Nierenberg and Ransil [8] reported a series in which the Q to apex of T wave interval corrected for rate was 0.27 seconds or less in over 90% of hypercalcemia cases.
The presence of hypercalcemia and hypokalemia produces an interesting ECG. This can be seen with multiple myeloma. The hypercalcemia results in a short ST segment and the hypokalemia results in a prominent U wave. Tachyarrhythmias due to hypercalcemia are uncommon in the literature. However, bradyarrhythmias with hypercalcemia are well described [9]. The classic case of hypercalcemia is that of patients presenting with metastatic non-parathyroid cancer that secretes recombinant parathyroid hormone (rPTH).
Hypocalcemia: The surface electrocardiographic changes associated with hypocalcemia are the opposite of those associated with hypercalcemia. Phase 2 depolarization of the cardiac myocyte action potential is lengthened, so the ST segment is prolonged. Suriwicz and Knilans [10] state that hypothermia and hypocalcemia are the only two conditions that increase the length of the ST segment without changing the T wave duration. Suriwicz and Lepeschkin [11] report that isolated hypocalcemia rarely causes the QTc interval to lengthen beyond 140% of normal. If the calculated QTc interval is over 140% of normal, then the measured QT interval may actually be the QU interval due to concomitant hypokalemia. Early after-repolarizations may be observed with hypocalcemia. Importantly, life-threatening arrhythmias can be precipitated with hypocalcemia in the presence of digoxin.
Vigilance for hypocalcemia is critical after thyroidectomy in the case of unintentional parathyroidectomy and, of course, after parathyroidectomy. Clinical scenarios other than primary parathyroidism in which hypocalcemia may occur include acute pancreatitis, rhabdomyositis, and other specific endocrine disorders involving calcium ion metabolism. Carlstedt and Lind [12] report that as many as 50% of critical care patients may have hypocalcemia. The classic clinical features of hypocalcemia include neuromuscular irritability, tetany, and tonic clonic seizure activity. Bedside tests consistent with hypocalcemia include Chvostek’s and Trousseau’s signs. Therapy for life-threatening arrhythmias and severe symptoms secondary to hypocalcemia includes intravenous calcium solution infusion along with treatment for any other co-existing electrolyte and metabolic conditions.
Other syndromes: Magnesium is largely an intracellular cation. Approximately 1% of total body magnesium is in the extracellular space [13]. No specific arrhythmias are associated with hyper- or hypomagnesemia. However, hypomagnesemia may occur in the context of hypokalemia. Intravenous magnesium sulfate is part of the recommended therapy for torsade de pointes after defibrillation. Additionally, intravenous magnesium sulfate is often given routinely prior to administration of ibutilide for chemical cardioversion of atrial fibrillation.
The presence of isolated hyper- or hyponatremia within the limits compatible with human life is not associated with any specific ECG changes that are well described in the literature. It is noteworthy that hypernatremia in the context of severe hyperkalemia, that would otherwise cause an intraventricular conduction delay, results in a relatively shorter QRS duration than predicted by the degree of hyperkalemia alone. Conversely, the QRS duration is further lengthened in severe hyperkalemia with an intraventricular conduction delay if hyponatremia is present.
Torsade de pointes: Torsade de pointes is a syndrome of ventricular tachycardia in which the electrical axis “twists” around. The QRS complex exhibits a crescendo-decrescendo variation in amplitude. The R-R interval is frequently in the range of 200–250 bpm. One of the characteristic features of torsade is a long period of ventricular repolarization so that the QT interval is typically at least 500 ms long. This prolonged QT interval is most readily observed in the QT interval immediately prior to the onset of torsade. Most cases of torsade are preceded by long-short R-R cycles [14]. For example, after a premature ventricular complex a compensatory pause will occur, and then a sinus beat with a long QT interval will occur. If another PVC occurs, torsade may be initiated. If a premature stimulus occurs near the zenith of the T wave, it may be more likely to induce a ventricular arrhythmia [15]. However, a short couple variant with a particularly high mortality has been described [16, 17]. It is important to distinguish polymorphic VT with a normal QT interval from torsade as the treatment and prognosis may be different.
The QT interval is measured from the onset of the Q wave to the end of the T wave [18]. The QT interval can vary with heart rate. Bradycardia is often associated with a prolonged QT interval while tachycardia is associated with a shortened ...