![]()
Chapter 1
Standard Clinical Evaluation
Richard H. Beigi
Department of Obstetrics, Gynecology and Reproductive Sciences, Magee-Women's Hospital of the University of Pittsburgh Medical Center, Pittsburgh, PA, USA
A thorough and reproducible approach is required for every patient being evaluated for any lower genital tract complaints to assure an objective and complete clinical evaluation. The following chapter serves as a guide to performing such an evaluation.
Introduction
The clinical evaluation of women presenting with genital tract complaints requires a standard approach that leads to an objective, reproducible evaluation. This is a critical point to understand given the diverse conditions that are being evaluated. These diverse conditions, however, often have very closely overlapping clinical presentations, requiring the standard approach to maximize diagnostic accuracy and optimize outcomes. In general, the evaluation of women with lower genital tract complaints without physical examination and/or laboratory testing has been demonstrated to be suboptimal. Self-diagnosis has also been demonstrated to be inaccurate, and is generally discouraged. The syndromic management of women, based on subjective presentation alone, has been used in developing countries (and still is in certain settings) where a health infrastructure is lacking. However, thorough and careful history-taking, physical examination, and selected laboratory methods can significantly improve objectivity and, whenever possible, are strongly recommended in developed nations with an existent healthcare infrastructure. A recommended and reproducible approach to all women with lower genital tract complaints is described below.
Clinical Evaluation
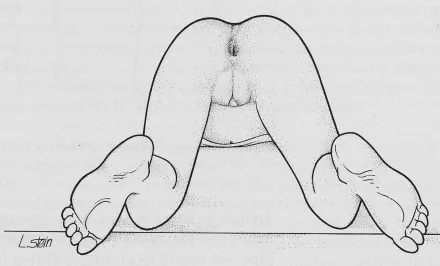
A thorough understanding of the vulvar, vaginal, and internal female genital tract anatomy is the key first step in assessingvulvovaginal complaints among women. As noted in Figure 1.1, the vulva is bound by the genitocrural folds laterally, the anus posteriorly, and the upper mons pubis superiorly. Importantly, hair follicles (coarse) are present on the inferior, lateral, and superior tissues of the vulva, but are lacking from the inner labia majora, labia minora, and the vaginal vestibule. The vaginal vestibule is separated from the inner labia minora by an artificial anatomic line, called the Hart line. This is an important landmark because it separates the nonmucous-secreting outer skin from the inner, mucous-secreting moist tissues of the vaginal vestibule and the hymenal ring. The vaginal vestibule is where the Bartholin and minor vestibular glands are located and produce lubricating fluids, where the vaginal orifice begins, and where the urethra opens at its meatus. Delineating and appreciating the exact anatomical location of physical findings is very important in deciphering the underlying etiology as well as administering effective treatment of sexually transmitted diseases (STDs) and the associated vulvovaginal syndromes/conditions.
The standard position for most gynecological examinations is the dorsal lithotomy (on back, with knees flexed, thighs flexed and apart, feet resting in stirrups). This positioning (Figure 1.1) allows in most scenarios the best physiologic view of the female anatomy and optimizes specimen collection for most laboratory analyses. Occasionally, due to anatomic restrictions, lack of mobility, or other factors, different positioning may be necessary or undertaken. This may be especially true for young women or girls who have never had pelvic examinations performed or are reticent for such an examination (covered more extensively in Chapter 2).
It is likewise essential for practitioners caring for women to have a thorough understanding of the internal female genital tract anatomy (Figure 1.2). This cross-section demonstrates the relationship of the vagina, cervix, uterus, and adnexae to each other as well as the relationship to the two other important organ systems in the pelvis – the gastrointestinal tract (large bowel) and the urinary system (urethra and bladder). Distinguishing signs and/or symptoms attributable to the genital tract versus the other adjacent organ systems is often challenging but occasionally very important to successful management.
With this basic understanding of the female anatomy, history-taking becomes the next key step (as in nearly all clinical evaluations). Focusing on specific symptomatology, exact timing of the onset of symptoms and length of time, alleviating and exacerbating factors, recent therapies (including self-chosen and nonprescription remedies) and presence/absence of partner(s) symptoms will help to narrow the differential diagnoses. The Centers for Disease Control and Prevention (CDC) has recommended an approach to sexual history-taking (5 Ps), which is covered more extensively in Chapter 17 (Prevention of Sexually Transmitted Diseases). This approach is strongly recommended to assist providers' ability to obtain key information in these evaluations that will lead to the correct diagnosis and management, thus improving clinical outcomes. Use of nonjudgmental, open-ended questions is suggested when eliciting a sexual history as this approach is more likely to produce meaningful and accurate information about sexual practices and risk factors.
After taking a thorough history and with a thorough understanding of the anatomy, all evaluations begin with an inspection of the vulvar area. Close attention to all elements of the external genital anatomy, the presence of any lesions, appearance and color of the skin, labia majora and minora, as well as any atypical findings is required. Obvious large lesions or other major findings should be noted and captured in a drawing for future reference. More subtle findings such as fissuring, labial agglutination, or small ulcers should also be sought, as they often give direct insight into the etiology of symptoms. Lymph nodes in the inguinal region should be routinely palpated for enlargement and/or tenderness (or rarely, fluctuance). For some of the vaginitides (i.e. vaginal candidiasis) and especially the noninfectious and/or dermatologic conditions, vulvovaginalinspection is often a high-yield component of the examination. After a thorough examination of the vulvar tissues (specific attention to color, tissue appearance, lesions, scaling, etc.), the vaginal introitus should be inspected for color changes, the presence of lesions, and vaginal tissue rugosity (as a sign of endogenous estrogen stimulation).
Subsequent to the thorough inspection of the external anatomy and vaginal introitus, anappropriately sized speculum should be placed into the vaginal vault, and the vaginal tissues and cervix inspected. Again, attention to tissue color, texture, presence of discharge, anatomic origin of the discharge (vaginal vs. cervical os), and other signs should be noted on every patient. Origin of discharge is a key point, as cervical discharge has a vastly different etiology, evaluation, and management compared to discharge emanating from the vaginal tissues. Evaluation of discharge microscopically is also a very important component of nearly all genital tract evaluations (when considering infectious conditions) and can often yield highly valuable information. The specifics of these techniques will be discussed in ensuing chapters. Close attention to the cervical appearance is also a key to this part of the examination. Once this is performed (and any appropriate specimens obtained for testing), the speculum is removed.
Internal bimanual pelvic examination is then carried out in the usual fashion using two fingers in the posterior vagina to palpate and move the cervix, while placing the other hand on the lower abdomen to simultaneously palpate the internal genital organs. This component of the examination is done with specific attention to the findings of pelvic tenderness on motion of the cervix (i.e. cervical motion tenderness) and any adnexal and/or uterine findings. This too is an important part of the examination that can often give vital information about upper genital tract infection that requires specific (often prolonged) therapy. Rectovaginal examination is also an often used method to help to discern further the nature of any findings on pelvic examination, as well as specific findings in the anorectal canal itself, and should be used liberally.
Conclusion
Use of this standard and reproducible approach on every patient will improve the ability of the provider to objectively determine the cause of the symptomatology. This in turn will improve the management and patient outcomes from these often physically and psychologically debilitating conditions.
![]()
Chapter 2
Specific Considerations for Pediatric and Adolescent Patients
Eduardo Lara-Torre
Department of Obstetrics and Gynecology, Virginia Tech Carilion School of Medicine, Roanoke, VA, USA
The evaluation and management of children and adolescents with exposure or infection with sexually transmitted disease requires special considerations and care. The difference in examination techniques and instruments to facilitate these examinations will assist the providers in performing the age appropriate examination and minimizing trauma. Prophylaxis for sexual assault cases as well as screening and treatment for certain diseases requires special considerations for children and adolescents. The Centers for Disease Control and Prevention (CDC) updated the recommendations in December, 2010 and provides a great resource for practitioners caring for this population.
Introduction
The management of sexually transmitted infections (STIs) in children and adolescents requires the practitioner to apply a different approach from the one used for adult women.
To understand the screening and treatment algorithms, one must understand some basic epidemiology and behaviors that differentiate these patients from their counterparts. It is also important to understand the indications, techniques, and alternative methods of screening utilized with this population, especially because these patients may be hesitant to be screened and examined in the traditional way. When dealing with children and adolescents, understanding local law and state statutes regarding the confidentiality of their reproductive healthcare is also important as it dictates the type of services they can receive without parental notification and also determines the rules and regulations for reporting. This is not only noted in the presence of certain infections such as chlamydia, but more importantly among those patients who might have been victims of sexual abuse.
In general, children are screened and treated for STIs related to involuntary intercourse or genital contact. Examples of these inappropriate contacts may include sexual abuse with penetration or simply the placement of male genitals in contact with the child's vulva. The management of children with STIs requires a multidisciplinary approach and should include collaboration between the governmental agencies (such as child protective services), laboratory, and clinicians. Some infections acquired after the neonatal period are consistent with sexual abuse (i.e. gonorrhea), while other diseases such as HPV may not be. A full understanding of the management of victims of sexual abuse is important for those caring for this population and is beyond the spectrum of this chapter.
Adolescents, on the contrary, are more commonly screened and treated for acquired infections due to consensual sex. The approach to each of these scenarios is different, and the evaluation and management for each patient and conditions will be presented in separate sections.
The Physical Examination
Prepubertal Girls
The initial step in the examination of children is to obtain the cooperation of the child. While explaining the examination to the patient, allow her to have some say in the process (e.g. give the child a choice of examination gown to wear). Starting with an overall assessment of the child before initiating the genitalia examination is recommended as it will provide an opportunity for the patient to become comfortable with the examiner and proceed with the genital examination.
In order to be able to visualize the genitalia of children, positioning plays a key component to the success of the examination. Multiple...