- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
About this book
This important revision presents the accumulated knowledge of its highly-regarded author, Dr. Abraham Rudolph, who is internationally recognized as one of the world's leading pioneersin the field of Pediatric Cardiology. Fully revised and updated, the book includes sections considering the changes in pathophysiology with growth into adulthood and the effects of various treatment approaches. The author explains the physiology of normal fetal circulation and the effects of congenital cardiac lesions, with particular reference to the interactions between the lesions and fetal cardiovascular development.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Congenital Diseases of the Heart by Abraham Rudolph in PDF and/or ePUB format, as well as other popular books in Medicine & Cardiology. We have over one million books available in our catalogue for you to explore.
Information
CHAPTER 1: The fetal circulation
The circulation in the fetus differs from that in the adult. Knowledge of the course and distribution of the fetal circulation is important to our understanding of the manner in which various congenital heart lesions influence the normal circulation. The circulation undergoes continuous maturation during gestation, both morphologically and functionally, and these changes during development may be greatly influenced by congenital cardiac lesions. Furthermore, we now recognize that the clinical manifestations of congenital heart disease are intimately related to postnatal changes in the circulation. At birth, dramatic changes occur as the gas exchange function is transferred from the placenta to the lungs.
The presence of congenital heart lesions may profoundly affect the alterations in the circulation necessary for adaptation and postnatal survival. In this chapter I review current knowledge of the fetal circulation and its distribution and the changes that occur postnatally. The pulmonary circulation and the changes it undergoes after birth are described in Chapter 5 and fetal function and perinatal changes of the ductus arteriosus are discussed in Chapter 6.
Most of the information regarding the fetal circulation has been derived from the sheep, which has a gestational period of about 150 days as compared with the human of about 280 days. However, with the advent of ultrasound techniques, knowledge of the circulation of the normal fetus and of fetuses with congenital heart lesions has been increasing. It cannot be assumed that development in different species is the same at similar stages of gestation. This is not only because of inherent species differences but also because there are wide variations in the degree of maturity at the time of birth. The rat and the rabbit are relatively immature at birth, whereas the guinea pig is very mature at birth; the lamb is relatively mature and the human infant somewhat less mature. Furthermore, in considering distribution of the circulation, there are marked differences in body proportions. Whereas the brain in the mature lamb fetus is only about 3% of body weight, the human brain comprises about 12% of body weight in the term fetus. Despite these differences, observations we have made in previable human fetuses and ultrasound studies in the human fetus indicate that the course and distribution of the circulation are similar to those in the fetal lamb. However, as discussed below, the quantities of blood ejected by the ventricles and the volumes distributed to various organs differ considerably in human and lamb fetuses.
Because gestational period varies in different species, it is convenient, in making comparisons, to express gestation as a fraction of the normal period for the species. Thus, in the lamb with a 150-day gestation, 100 days is denoted as 0.66 gestation.
Postnatal circulation
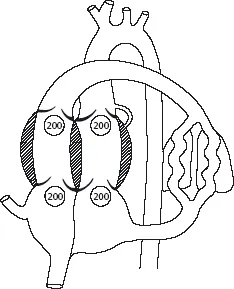
Postnatally, respiratory gases enter and leave the body through the lungs, and energy sources are provided from the gastrointestinal tract, entering the portal venous system to be distributed to the liver. The adult circulation is characterized by serial flow of venous blood into the right atrium (Figure 1.1). It is ejected by the right ventricle into the pulmonary circulation to be oxygenated in the lungs and returns to the left atrium and ventricle to be ejected into the aorta for distribution to body organs. Carbon dioxide is removed and oxygen taken up in the lungs; a variable proportion of oxygen is extracted, and carbon dioxide and metabolites are added to blood by the tissues. Apart from minor amounts of bronchial venous blood that may enter the pulmonary vein and coronary venous blood that may empty directly into the left ventricular cavity, there is essentially no mixing of pulmonary venous and systemic arterial blood with poorly oxygenated systemic venous and pulmonary arterial blood. Postnatally, metabolic substrates, absorbed from the gastrointestinal tract into the portal venous system, are first delivered to the liver and then enter the systemic venous system and pass through the lungs before being delivered to tissues by the arterial circulation.
Figure 1.1 Course of blood flow in the adult circulation. The volumes of blood ejected by each ventricle and returning to each atrium are similar postnatally.
Circulation in the fetal lamb
Course of blood flow
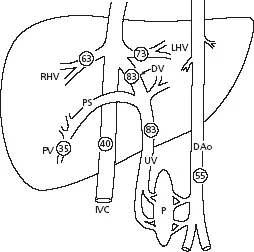
The course of the circulation in the fetus is shown in Figures 1.2 and 1.3. Blood is oxygenated in the placenta and returns to the fetus through the umbilical veins, which enter the body through the umbilicus and join the portal vein. Umbilical venous blood has a Po2 of about 32–35 mmHg when the mother is breathing ambient air and its oxygen saturation is about 80–85%. The umbilical vein passes from the umbilicus to the hilum of the liver; it provides branches to the left lobe of the liver and then divides into the ductus venosus and a large arcuate branch, which courses to the right in the hilum, where it is joined by the portal vein (Figure 1.3). Branches to the right lobe of the liver arise beyond this junction. The ductus venosus passes dorsally and cephalad through the liver parenchyma to join the inferior vena cava immediately beneath the diaphragm. The left hepatic vein joins the ductus venosus at its entry into the inferior vena cava, so there is a common entry orifice. In the sheep fetus this orifice is partly covered by a thin, valve-like membrane on its caudal edge [1]. The right hepatic vein enters the inferior vena cava separately, and the orifice is partly covered by a valve-like structure caudally. The function of these valve-like membranes is not known, but we have conjectured that they may facilitate directional flow of the various venous streams entering the inferior vena cava at this site. Previously, it was generally believed that umbilical and portal venous blood mixed in the porta hepatis and was then distributed to the left and right liver lobes and through the ductus venosus. However, Lind et al. [2] obtained umbilical venous angiograms in human fetuses immediately after delivery and suggested that umbilical venous blood passes preferentially to the left liver lobe and through the ductus venosus.
Figure 1.2 The general course of the mammalian fetal circulation. Ao, aorta; DA, ductus arteriosus; DV, ductus venosus; LA, left atrium; LV, left ventricle; PA, pulmonary artery; RA, right atrium; RV, right ventricle.
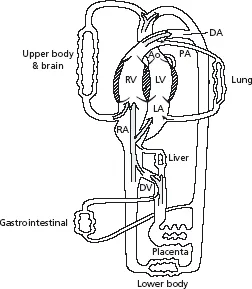
Figure 1.3 Course of blood flow in the region of the porta hepatis. Umbilical venous blood is distributed to the left lobe of the liver. The ductus venosus arises from the umbilical vein, which then arches to the right to join the portal vein. Portal venous blood is largely distributed to the right liver lobe and only a small proportion passes through the ductus venosus. IVC, inferior vena cava; LHV, left hepatic vein; RHV, right hepatic vein; SVC, superior vena cava.
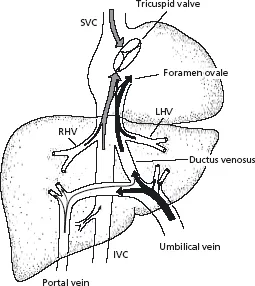
Using radionuclide-labeled microspheres, we were able to define not only the patterns of blood flow in the fetal liver but also the quantities of blood flowing through various channels in the fetal sheep [3]. Umbilical venous blood is distributed to the left lobe of the liver, through the ductus venosus, and via the arcuate branch, to the right liver lobe. Almost all portal venous blood is distributed to the right liver lobe. Only a small proportion, about 5–10% or less, passes through the ductus venosus and none is delivered to the left lobe. Thus the left lobe of the fetal liver receives well-oxygenated umbilical venous blood and a small supply from the hepatic artery. The right lobe receives a mixture of poorly oxygenated portal venous and umbilical venous blood, as well as a small amount from the hepatic artery. This accounts for the fact that the oxygen saturation of left hepatic venous blood is higher than that of right hepatic venous blood [4] (Figure 1.4).
Figure 1.4 Blood oxygen saturations are shown in vessels in the region of the liver in the fetal lamb. DAo, descending aorta; DV, ductus venosus; IVC, inferior vena cava; LHV, left hepatic vein; P, placenta; PS, portal sinus; PV, portal vein; RHV, right hepatic vein; UV, umbilical vein.
The distributions of ductus venosus blood, blood from the distal inferior vena cava, and blood from the left and right hepatic veins have also been examined using radionuclide-labeled microspheres in fetal sheep [5]. Umbilical venous blood passing through the ductus venosus into the inferior vena cava is preferentially directed across the foramen ovale into the left atrium and left ventricle; only a small proportion passes into the right atrium and through the tricuspid valve. Abdominal inferior vena cava blood, in contrast, preferentially streams across the tricuspid valve into the right atrium and right ventricle and only a relatively small proportion crosses the foramen ovale to the left atrium. Blood from the left hepatic vein tends to follow the course of the ductus venosus stream, being preferentially distributed across the foramen ovale, whereas right hepatic venous blood preferentially streams across the tricuspid valve, following the course of abdominal inferior vena cava blood (see Figure 1.3). This preferential distribution of blood to the foramen ovale or the tricuspid valve suggests that there is streaming within the inferior vena cava between the liver and the heart. This can be observed directly in the fetal lamb when a right thoracotomy is performed. Observation of the thoracic portion of the inferior vena cava reveals well-oxygenated and poorly oxygenated blood streams. The anterior and right portion of the vessel is seen to have a poorly oxygenated stream, but blood flowing in the posterior and left portion is clearly well oxygenated. The streaming patterns in the inferior vena cava have also been observed by color flow Doppler studies. The ductus venosus stream has a velocity of about 55 cm/s and is directed largely through the foramen ovale, whereas distal inferior vena cava blood has a considerably lower velocity of about 15 cm/s and streams across the tricuspid valve. It is likely that the high velocity of the ductus venosus stream contributes to maintaining its preferential distribution across the foramen ovale. Ultrasound examination of human fetuses have also shown similar differences in ductus venosus and distal inferior vena cava velocities, and similar preferential streaming patterns.
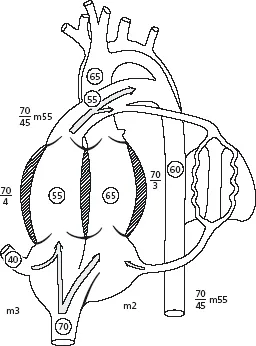
The inferior margin of the atrial septum separates the entrance of the inferior vena cava from the left atrium, but the crescentic edge of the superior portion of the atrial septum, the crista dividens, overlies the inferior vena cava (see Figure 1.3). The posterior left portion of the inferior vena cava thus connects directly through the foramen ovale to the left atrium. During phases of the cardiac cycle, the eustachian valve and the lower portion of the atrial septum move in unison, either to the left to facilitate movement of blood through the foramenovale, or to the right to enhance flow through the tricuspid valve [6]. The preferential streaming of ductus venosus and left hepatic venous blood through the foramen ovale distributes blood of higher oxygen saturation to the left atrium and ventricle and thus into the ascending aorta. Blood of lower oxygen saturation from the abdominal inferior vena cava and the right hepatic vein is preferentially distributed into the right ventricle and pulmonary artery.
The ductus venosus serves as a partial bypass of the hepatic microcirculation for umbilical venous blood. It may reduce the impedance to umbilical venous return by avoiding the need for all the blood to pass through the liver. Although it does facilitate passage of well-oxygenated blood to the left side of the heart, the proportion of umbilical venous blood that passes through the ductus varies greatly, both in the lamb and the human fetus, from about 20 to 90% [3,7]. In some species, such as the horse and the pig, the ductus venosus is not detectable in thelatter part of gestation. The importance of the ductus venosus in the fetus is thus questionable, but it may be important in initiating some of the effects of aortopulmonary transposition on development of the pulmonary circulation (see Chapter 18).
Superior vena cava blood is largely directed by the tubercle of Lower to the tricuspid valve and is distributed into the right ventricle. Only about 5%, or less, flows through the foramen ovale into the left atrium in the normal fetus. Ultrasound examination of the fetal lamb indicates that the small amount of superior vena cava blood that enters the foramen ovale does so indirectly, by first flowing retrograde into the upper portion of the inferior vena cava and then entering the foramen. This phenomenon is markedly accentuated during fetal hypoxemia [6].
Right ventricular blood is ejected into the pulmonary trunk, and the larger proportion passes through the ductus arteriosus to the descending aorta, with the remainder entering the pulmonarycirculation (Figure 1.5). Blood that passes from the pulmonary trunk through the ductus arteriosus is directed to the descending aorta; none passes retrogradely across the aortic isthmus to the ascending aorta and its branches. The left atrium receives blood from the foramen ovale and pulmonary veins, and then empties into the left ventricle, which ejects into the ascending aorta. Most ascending aortic blood is distributed to the coronary circulation, head and cerebral circulation, and upper extremities; only a small proportion passes across the aortic isthmus into the descending aorta. The major proportion of descending aortic blood is distributed to the umbilical–placental circulation and the remainder to the abdominal organs and the tissues of the lower trunk and lower extremities.
Admixture of oxygenated and systemic venous blood
In the adult circulation, there is essentially no mixing of oxygenated pulmonary venous and systemic venous blood. In the fetus, there are several sites of mixing. Portal and umbilical venous bloods enter the vessels in the porta hepatis. Blood from the ductus venosus, left and right hepatic veins, and abdominal inferior vena cava all enter the thoracic portion of the inferior vena cava. Admixture occurs in the left atrium, where blood entering the foramen ovale from the inferior vena cava is joined by pulmonary venous blood. As mentioned above, the preferential streaming of blood partly separates the well-oxygenated and poorly oxygenated blood, favoring distribution of oxygenated blood into the left ventricle and ascending aorta and providing blood with a higher oxygen content to the heart, brain, and other upper body tissues. Systemic venous blood is preferentially directed into the right ventricle, pulmonary trunk, and ductus arteriosus to the descending aorta and its branches to the lower body, as well as to the placenta.
Figure 1.5 Course of the circulation in the heart and great vessels in the late-gestation fetus. The figures in circles within the chambers and vessels represent percent oxygen saturation levels. The figures alongside the chambers and vessels are pressures in mmHg related to amniotic pressure level as zero. m, mean pressure. The aortic arch and its branches are shown for both the human and the lamb. In the lamb, a single vessel, the brachiocephalic trunk, gives rise to carotid and subclavian arteries. In the human, the innominate and left carotid and subclavian arteries arise separately.
Because umbilical venous and vena cava blood is mixed, the blood delivered to the fetal body and the placenta contains varied proportions of oxygenated and systemic venous blood. Hence some umbilical venous blood is returned to the placenta after passing through the ductus venosus and foramen ovale or ductus arteriosus shunts without first being delivered to fetal tissues to permit oxygen uptake. This situation is equivalent to that occurring postnatally with some congenital heart lesions (e.g., atrial or ventricular septal defect), in which oxygenated blood passes from the left atrium or left ventricle into the right side of the heart to be recirculated to the lung. This, termed a left-to-right shunt, imposes an additional workload on the heart. Similarly, with congenital heart lesions in which systemic venous blood is shunted through an abnormal communication into the left side of the heart to be distributed back to the body tissues without passing through the lung, a right-to-left shunt occurs. The blood returning to the heart from the superior and inferior vena cava that is distributed to the fetal tissues without first being delivered to the placenta for oxygenation is effectively a right-to-left shunt. This effective right-toleft shunt contributes to inefficiency of the fetal circulation. In the sheep fetus under normal conditions, right-to-left shunt represents about 45% of superior vena cava and 53% of inferior vena cava blood [8]. Umbilical venous blood that passesthrough the ductus venosus and foramen ovale or ductus arteriosus and which is distributed back to the placenta is an effective left-to-right shunt. This represents about 22% of umbilical venous blood, and the combined left-to-right and right-to-left shunts constitute about 33% of the combined ventricular output of the fetal heart.
Intravascular pressures in the fetus
In the postnatal animal or human, it is customary to express pressures with reference to atmospheric pressure as the zero. However, the fetus is surrounded by amniotic fluid in the uterus within the abdomen, and all pressures are subjected to an increase from the environmental pressure. Thi...
Table of contents
- Cover
- Title
- Copyright
- Preface
- CHAPTER 1: The fetal circulation
- CHAPTER 2: Perinatal and postnatal changes in the circulation
- CHAPTER 3: Oxygen uptake and delivery
- CHAPTER 4: Functional assessment
- CHAPTER 5: Prenatal and postnatal pulmonary circulation
- CHAPTER 6: The ductus arteriosus and persistent patency of the ductus arteriosus
- CHAPTER 7: Ventricular septal defect
- CHAPTER 8: Atrial septal defect and partialanomalous drainage of the pulmonary veins
- CHAPTER 9: Atrioventricular septal defect
- CHAPTER 10: Bicuspid aortic valve and aortic stenosis
- CHAPTER 11: Aortic atresia, mitral atresia, and hypoplastic left ventricle
- CHAPTER 12: Aortic arch obstruction
- CHAPTER 13: Total anomalous pulmonary venous connection
- CHAPTER 14: Pulmonary stenosis and atresia with ventricular septal defect (tetralogy of Fallot)
- CHAPTER 15: Pulmonary stenosis and atresia with intact ventricular septum
- CHAPTER 16: Tricuspid atresia and hypoplastic right ventricle
- CHAPTER 17: Ebstein malformation of the tricuspid valve
- CHAPTER 18: Aortopulmonary transposition
- CHAPTER 19: Truncus arteriosus communis
- Index
- Color plates are found facing