![]()
Part 1: Epidemiology, Anatomy and Imaging
1
Epidemiology and pathophysiology of carotid artery disease
Kosmas I. Paraskevas,1 Nikolaos Bessias,1 Dimitri P. Mikhailidis2
1Red Cross Hospital, Athens, Greece
2Royal Free Hospital Campus, University College London, London, UK
Carotid artery disease can be the cause of cerebrovascular symptoms, namely transient ischemic attacks (TIAs), amaurosis fugax, and stroke. This chapter considers the epidemiology and pathophysiology of carotid artery disease.
Epidemiology
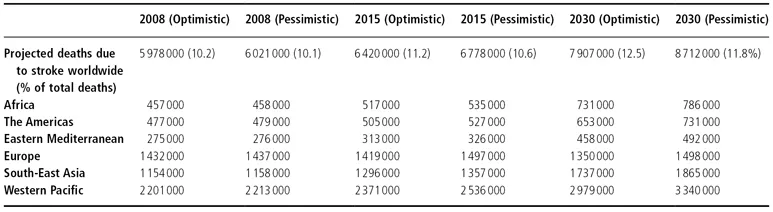
According to the most recent World Health Organization (WHO) report,1 cerebrovascular disease (stroke) is the second leading cause of death worldwide after ischemic heart disease. In 2004, stroke was responsible for 9.7% (n = 5 700 000) of deaths worldwide. A further analysis by national income, showed that whereas stroke was the fifth leading cause of death in low-income countries, accounting for 1 500 000 deaths in 2004 (5.6% of total deaths), it was the second leading cause of death in high-income countries, accounting for 800 000 deaths (9.3% of total deaths) and the leading cause of death in middle-income countries, accounting for 3 500 000 deaths in 2004 (14.2% of total deaths).1 Optimistic and pessimistic scenarios for the projected deaths due to stroke worldwide for the years 2008, 2015, and 2030 as calculated by the WHO are given in Table 1.1.
Table 1.1 Optimistic and pessimistic scenarios for projected deaths due to stroke for the years 2008, 2015, and 2030.2
Approximately 9 000 000 episodes of first-ever stroke occurred worldwide in 2004.2 A separate analysis by region showed 700 000 first-ever strokes in Africa, 900 000 in North and South America, 400 000 in the Eastern Mediterranean, 2 000 000 in Europe, 1 800 000 in South-East Asia, and 3 300 000 in the Western Pacific.2
Stroke is the third leading cause of death in the US after ischemic heart disease and cancer.3 Among adults older than 20 years, the estimated prevalence of stroke in 2005 was 5 800 000 (approximately 2 400 000 males and 3 400 000 females). Each year about 780 000 people experience a new or recurrent stroke. About 600 000 of these are first attacks and 180 000 are recurrent episodes. On average, every 40 s someone in the US has a stroke.3 Of all strokes in the US population, 87% are ischemic, 10% are intracerebral hemorrhage, and 3% are subarachnoid hemorrhage.3
Male stroke incidence rates are greater than female rates at younger ages but not at older ages. The male-to-female incidence ratio was 1.25 for 55–64 years; 1.50 for 65–74 years; 1.07 for 75–84 years; and 0.76 for over 85 years. Blacks have almost twice the risk of first-ever stroke compared with whites. The age-adjusted stroke incidence rates at 45–84 years are 6.6 and 4.9 per 1000 population in black males and females, and 3.6 and 2.3 in white males and females, respectively.3
Stroke accounted for 1 in every 16 deaths in the US in 2004.3 Stroke mortality for that year was 150 074 (58 800 males; 91 274 females). Stroke total mention mortality (includes deaths where the given cause was listed anywhere on the death certificate or was selected as the underlying cause, whether primary or secondary) in 2004 was approximately 253 000.
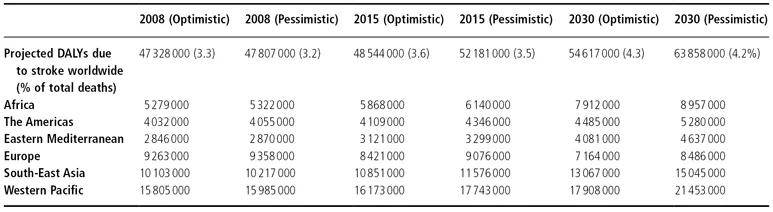
Apart from being a leading cause of death, stroke is also a major cause of moderate/severe disability. According to the data provided by the WHO, in 2004 there were 30 700 000 stroke survivors worldwide: 1 600 000 in Africa, 4 800 000 in North and South America, 9 600 000 in Europe, 4 500 000 in South-East Asia, and 9 100 000 in the Western Pacific.2 In terms of disease burden as measured using disability-adjusted life years (DALYs), where 1 DALY represents the loss of the equivalent of 1 year of full health, in 2004 and for all ages, stroke was the sixth leading cause of burden of disease, being responsible for 46 600 000 DALYs worldwide.4 This ranking is deceiving because it is the average from both low- and high-income countries. If we consider low-income countries alone, stroke does not appear in the top 10 causes of disease; instead conditions such as malaria and tuberculosis dominate.5 Thus, for medium- and high-income countries, stroke is in fact even higher in the ranking; it is the third leading cause of disease burden, being responsible for 27 500 000 and 4 800 000 DALYs, respectively.4 Optimistic and Pessimistic scenarios for the projected DALYs due to stroke worldwide for the years 2008, 2015, and 2030 as calculated by the WHO are shown in Table 1.2.
Table 1.2 Optimistic and pessimistic scenarios for projected disability-adjusted life years (DALYs) due to stroke for the years 2008, 2015, and 2030.2
Pathophysiology
Atherosclerosis is the primary pathologic entity responsible for the development of carotid artery disease, accounting for approximately 90% of lesions in the Western world. The remaining 10% are caused by a variety of diseases (Table 1.3).6
Table 1.3 Other causes of carotid artery disease.
- Fibromuscular dysplasia
- Arterial kinking
- Traumatic occlusion
- Intimal dissection
- Radiation-induced carotid stenosis
- Fibrinoid necrosis
- Amyloidosis
- Polyarteritis nodosa
- Wegener’s granulomatosis
- Granulomatous angiitis
- Giant cell arteritis
- Amphetamine-associated arteritis
- Infectious arteritis
- Moya-moya disease
- Allergic angiitis
|
Atheromatous lesions characteristically occur at branches or arterial bifurcations. The most common site is at the bifurcation of the common carotid artery, particularly the carotid bulb. The predilection of the carotid bifurcation for atheromatous plaques relates to arterial geometry, flow velocity profiles, flow streamline patterns, and wall shear stress.7
The initial lesion of atherosclerosis is the “fatty streak”.8,9 The formation of fatty streaks arises from a focal increase in the content of lipoproteins within the intima. These lipoproteins undergo chemical modifications, namely lipoprotein oxidation and non-enzymatic glycation.8,9 After the accumulation of extracellular lipid, recruitment of leukocytes (monocytes and lymphocytes) occurs.10 Low-density lipoprotein (LDL) particles augment the expression of leukocyte adhesion molecules and also promote the chemotaxis of leukocytes through induction of cytokine release from vascular wall cells, such as interleukin-1 (IL-1) and tumor necrosis factor-α (TNF-α).9 The monocytes differentiate into macrophages and begin to ingest the lipoprotein particles by receptor-mediated endocytosis, thus transforming into lipid-laden foam cells.11 Some lipid-laden foam cells may die as a result of programmed cell death (apoptosis). This death of mononuclear phagocytes results in formation of the lipid-rich center, often called “the necrotic core,” of more complicated atherosclerotic plaques.9 Cytokines and growth factors [such as transforming growth factor-β (TGF-β)] elicited by modified lipoproteins, vascular wall cells, and infiltrating leukocytes can modulate function of arterial smooth muscle cells. These molecules stimulate the migration of smooth muscle cells from the tunica media into the intima.9 The smooth muscle cells synthesize the bulk of the extracellular matrix of the complex atherosclerotic lesion. In addition to locally produced mediators, atherogenic signals, related to blood coagulation and thrombosis, contribute to the evolution of atheroma.9,12 Fatty streak formation begins under a morphologically intact endothelium.12 In advanced fatty streaks, however, microscopic breaches in endothelial integrity occur.12 Microthrombi rich in platelets form at such sites due to exposure of the highly thrombogenic extracellular matrix of basement membrane.12 Platelet adhesion to the exposed matrix is the initial step in thrombus formation.12
The atherosclerotic plaque evolves with time. A complex balance between entry and removal of lipoproteins, accumulating leukocytes, cell proliferation and cell death, extracellular matrix production, and accumulation of calcium (calcification of the plaque) contribute to plaque evolution and lesion formation.9 With time, the atherosclerotic plaque increases in size, causing stenosis of the vascular lumen. The increasing stenosis of the vessel lumen has an adverse effect on blood flow and may give rise to an auscultated bruit. Whether detection of a carotid bruit during the general physical examination should be considered an alarming sign or an accidental finding has been extensively debated.13,14 Carotid bruits predict cardiovascular events and probably deserve further investigation.13,14 In addition, carotid bruits are associated with vascular risk factors (e.g., smoking, hypercholesterolemia, hypertension, diabetes mellitus).13,14
As the atherosclerotic plaque increases in size, a number of additional events take place that explain many of the clinical manifestations of atherosclerosis. With time, the microthrombi on the endothelium give rise to larger thrombi.12 These further occlude the lumen, restricting blood supply to the tissues. Additionally, large plaques have a propensity to rupture.9,12,15 Plaques that have proved vulnerable to rupture tend to have thin fibrous caps, relatively large lipid cores, and a high content of macrophages. As a result of plaque instability and plaque rupture, the thrombi formed on the surface of the plaque are released into the circulation (emboli), giving rise to acute ischemic events (i.e., stroke).9,12,15 Following such an atheromatous discharge, an open cavity remains within the central portion of the lesion, a so-called carotid ulcer. Carotid ulcers are the nidus for platelet aggregation and further thrombus formation and, thus, the source of further atherosclerotic emboli (secondary arterial emboli).9,12,15
Carotid plaque echolucency, as assessed by ultrasonography, also defines which plaque is high risk for atheroembolic events.16–18 Plaque echolucency is associated with increased lipid content and macrophage density (and sometimes hemorrhage).16–18 On the other hand, fibrous tissue and calcification dominate echodense plaques.16–18 Echolucent carotid plaques are associated with a higher risk for future ischemic stroke episodes,16–18 as well as coronary events.19 These plaques are also associated with elevated levels of triglyceride-rich lipoproteins and reduced levels of high-density lipoprotein (HDL) cholesterol.17 Risk factor intervention may be more beneficial in patients with echolucent than in those with echodense plaques.16–18
Several risk factors have been associated with an increased risk for the development of carotid atherosclerosis and carotid artery disease. These include smoking,18,20–23 hypertension,18,20–23...